Special Ankle Fractures
Detection of 'Not So Obvious' Fractures
Robin Smithuis
Radiology Department of the Rijnland Hospital, Leiderdorp, the Netherlands
Publicationdate
The ankle is the most frequently injured joint.
Management decisions are based on the interpretation of the AP and lateral X-rays.
In this article we will focus on detection of fractures, that may not be so obvious at first sight.
Before you read this article, you need to understand the classification of ankle fractures and exorotation injuries that were highlighted in Ankle - Fractures 1 and 2.
Posterior malleolus fractures
Almost all fractures of the posterior malleolus are part of a rotational injury resulting in a Weber B or Weber C fracture.
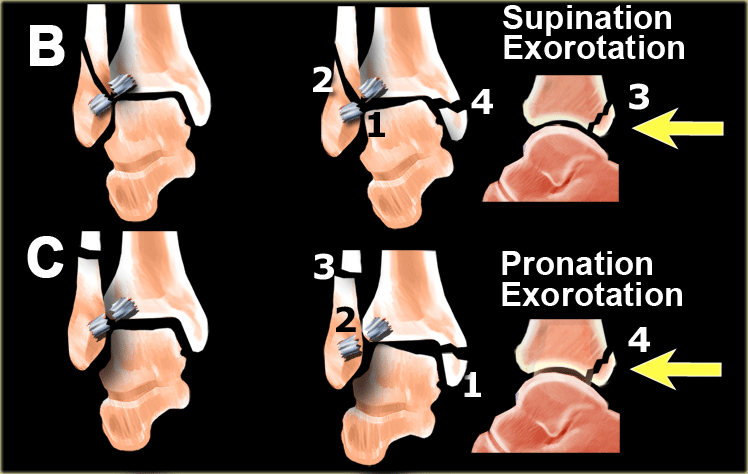
The tertius fracture is stage 3 in Weber B and stage 4 in Weber C (figure).
In some cases the tertius fractures are easily seen on the x-rays, but frequently they can be difficult to detect.
It is important to find these fractures, since a tertius fracture can be the only clue to an unstable ankle injury.
When we study the radiographs of a patient with an ankle injury, we have to study the region of the posterior malleolus very carefully.
In many cases there is only a small gap between the fracture parts and detection depends on optimal radiography and a high level of suspicion.
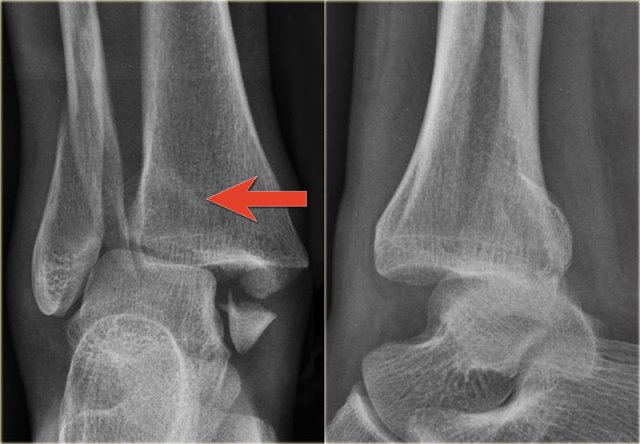
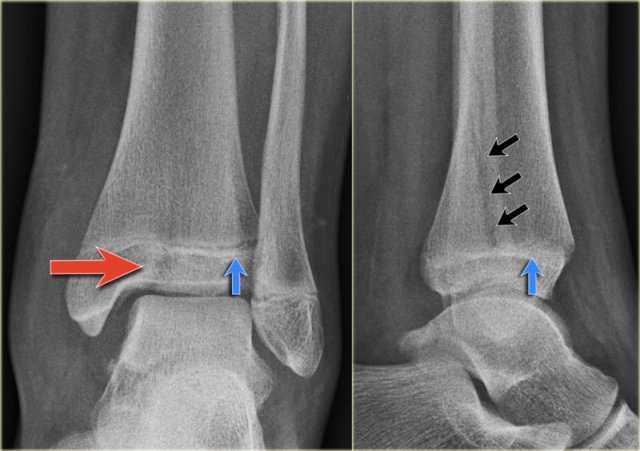
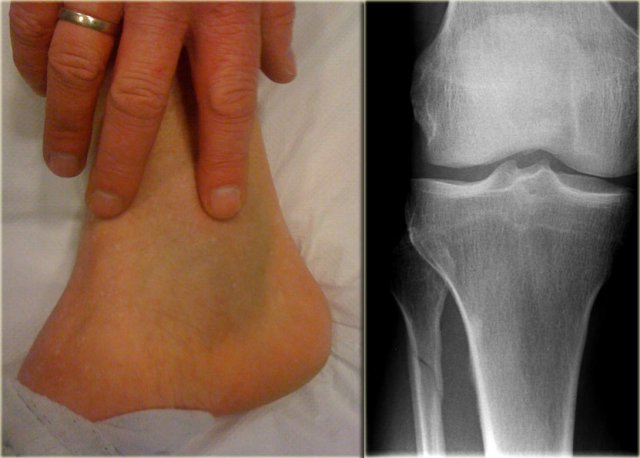
The images show an obvious Weber B fracture.
On the AP-view the linear lucency is the clue to a tertius fracture (red arrow).
It results from subtle malalignment of the fracture fragment.
Likewise in some cases malalignment can result in a linear density.
In this case there is a Weber B fracture with avulsion of the medial malleolus.
The bright line on the AP-view indicates a large tertius fracture fragment.
This tertius fracture can also be seen on the lateral view, but in many cases we need all the information of both the lateral and AP-view to diagnose a tertius fracture.
Here more examples of the bright line that indicates a tertius fracture.
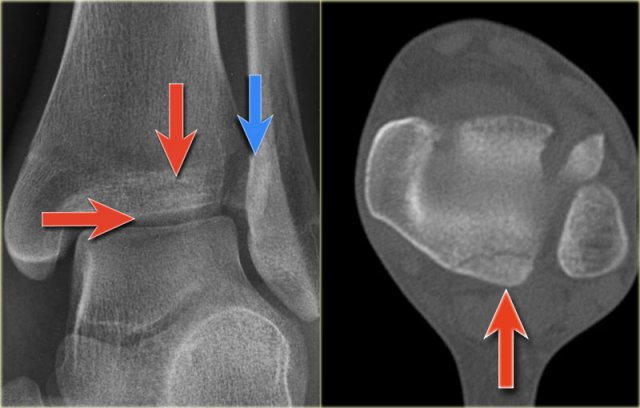
In some cases a fracture of the posterior malleolus is barely or not visible on the radiographs and can only be seen on CT.
First study the radiographs and then continue with the CT.
By the way....there are two fractures.
You can enlarge the images by clicking on them.
The CT shows an avulsion of the tertius at the insertion of the posterior syndesmosis (red arrows).
The alignment is so perfect, that you do not see the fracture on the radiographs.
Maybe the fracture is seen on the AP-view as indicated by the red arrows, but this is questionable.
Notice that there is also an avulsion at the tibial insertion of the anterior syndesmosis, i.e. Tillaux fracture.
This combination of findings implicate that the ankle is unstable.
A syndesmotic screw has to be inserted.
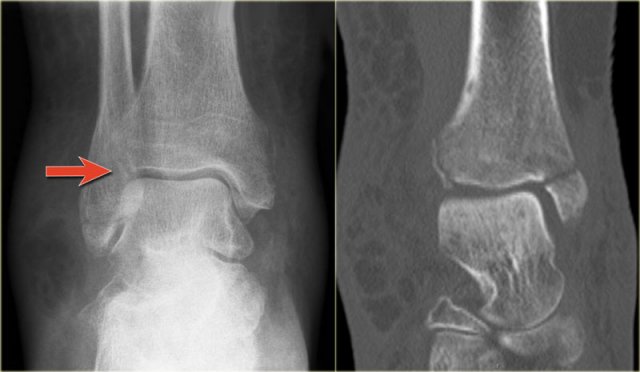
Here we have images of an extremely difficult case.
This woman had a distortion of the ankle and had pain on both medial and lateral side.
She was referred to the radiology department by her general practitioner.
The technician made the standard AP-, Mortise- and lateral view and showed them to the radiologist, who was a little bit puzzled.
First study the images and then continue reading.
The findings are:
-
Soft tissue swelling both medial and lateral (red arrows).
Especially the medial swelling should make you consider a pronation exorotation injury (Weber C). - Lucent line on Mortise view (black arrow) and lateral view. This should make you consider a tertius fracture.
The radiologist decided first to order a CT to find out if there really was a tertius fracture.
Continue with the CT and be amazed.
Scroll through the images.
It is amazing, that such a large tertius fragment is so difficult to see on the radiographs.
Also notice the soft tissue swelling on the medial side indicating rupture of the medial collateral ligaments (arrow).
Do you have an idea what kind of injury this is?
Medial soft tissue swelling and a tertius fracture are both indications of a Weber C or Pronation Exorotation injury.
Since there is no fibula fracture seen on the x-rays of the ankle, there must be a high fibular fracture.
At physical exam there was some swelling on the medial side and although the patient did not complain of any pain higher in the lower leg, there was some tenderness when the fibula was palpated.
This spot was marked and a fracture was found.
This case illustrates the importance of medial soft tissue swelling aswell as the finding of a tertius fracture.
According to Lauge Hansen we can conclude that this patient first had a rupture of the medial collateral ligaments (stage 1), followed by a rupture of the anterior syndesmosis (stage 2) and a high fibula fracture (stage 3) and finally an avulsion of the posterior malleolus, i.e. PE stage 4.
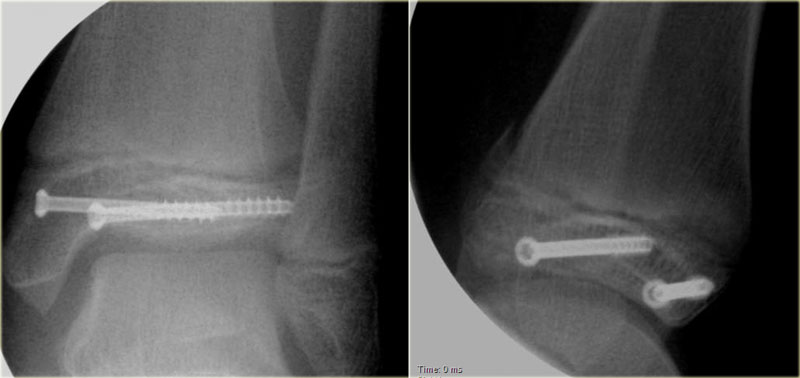
At surgery the ankle was found to be unstable and syndesmosis screws were inserted.
There was an indication for fixing the posterior malleolar fracture, since the fragment involved more than 25% of the articular surface of the distal tibia.
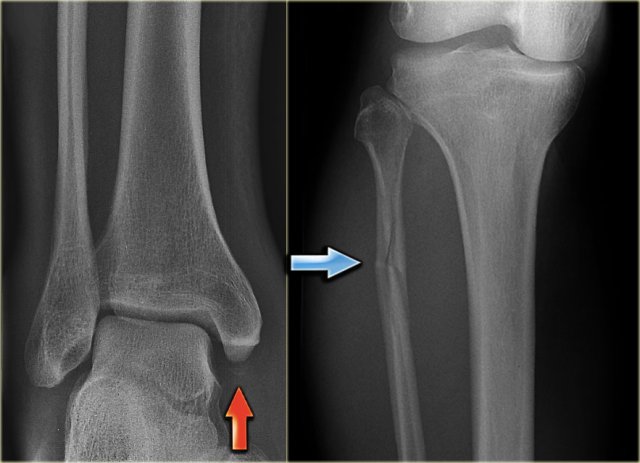
This patient had a twisted ankle and the only abnormality is seen on the lateral view.
This was thought to be an avulsion of the posterior malleolus.
Knowing that this can be the only clue to a high Weber C, additional radiographs were taken.
Continue with the images of the lower leg.
A subtle high fibula fracture is seen (arrow).
Final diagnosis is a Weber C fracture or according to Lauge Hansen: Pronation Exorotation injury stage 4.
Isolated Tertius fracture
A fracture of the posterior malleolus as an isolated finding is very uncommon.
It is seen when someone's foot hits the ground and a fragment of the posterior malleolus is pushed off by the talus.
The size of this fragment depends on the direction of the force (figure).
Salter-Harris fractures
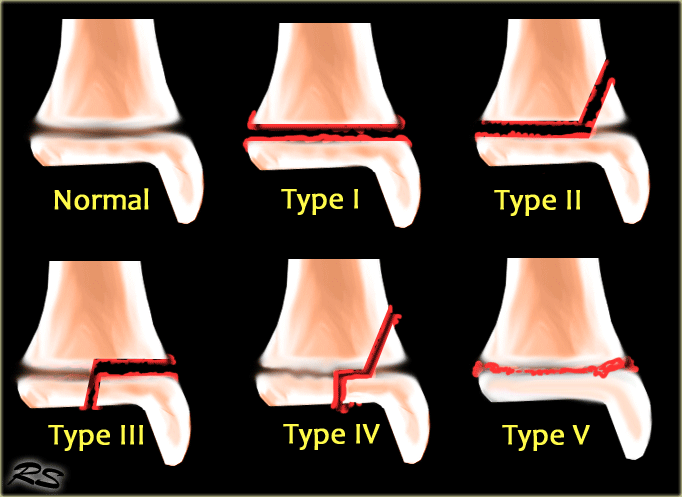
The Salter-Harris classification describes fractures that involve the epiphyseal plate or growth plate.
The most common is type II, which accounts for 75%.
- Type I - transverse fracture through the growth plate or physis
- Type II - fracture through the growth plate and the metaphysis, sparing the epiphysis
- Type III - fracture through growth plate and epiphysis, sparing the metaphysis
- Type IV - fracture through all three elements of the bone, the growth plate, metaphysis, and epiphysis
- Type V - compression fracture of the growth plate
These Salter-Harris fractures can be easily missed.
In many cases there is only minimal or no displacement.
The fracture through the growth plate is usually obscure and difficult to differentiate from normal variations of the growth plate.
And finally we tend not to look carefully at the epiphysis.
Type I
Type I Salter-Harris fractures tend to occur in younger children (5).
It is a transverse fracture through the cartilage of the growth plate or physis.
Often, x-rays of a child with a type I growth plate fracture will appear normal.
Most type I growth plate injuries are treated with a cast.
Healing of type I fractures tends to be rapid and complications are rare.
Type II
A type II growth plate fracture starts across the growth plate, but the fracture then continues up through the metaphysis.
This is the most common type of growth plate fracture, and tends to occur in older children. Often type II growth plate fractures must be repositioned under anesthesia, but healing is usually quick and complications are uncommon.

Type III
Type III is a fracture through the growth plate and epiphysis sparing the metaphysis.
A type III fracture also starts through the growth plate, but turns and exits through the end of the bone, and into the adjacent joint.
These injuries can be concerning because the joint cartilage is disrupted by the fracture.
Proper positioning is essential after a type II growth plate fracture.
These injuries also tend to affect older children in whom the growth plate is partially closed.
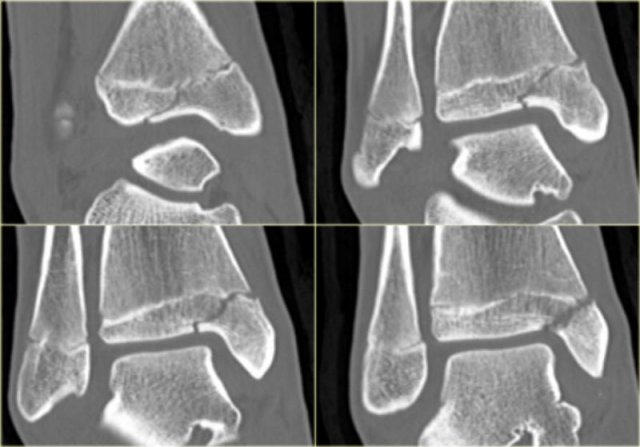
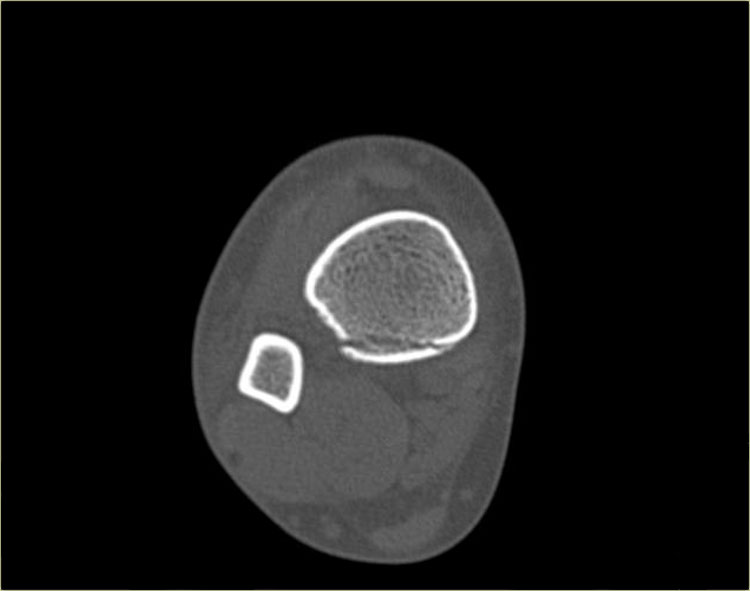
Study the images and then scroll to the next images.
The fracture through the epiphysis can be easily missed (blue arrow).
The fracture through the growth plate is only seen on CT.
Continue with the CT images.
The CT-images nicely display the fracture through the growth plate and the epiphysis.

Study the images and then scroll to the next images.
This is also a Salter-Harris type III fracture.
Notice that there is also a Tillaux fracture.
We will discuss these fractures in a moment.
Type IV
Type IV is a fracture through all three elements of the bone, the growth plate, metaphysis and epiphysis.
Notice that the epiphyseal fracture is in the sagittal plane, the fracture through the growth plate is in the axial plane and the metaphyseal fracture is in the coronal plane.
These fractures are also named triplane fractures.
These are discussed in the next chapter.
Proper positioning is also essential with type IV growth plate fractures, and surgery may be needed to hold the bone fragments in proper position.
Type V
Type V growth plate injuries occur with the growth plate is crushed.
Type V growth plate fractures carry the most concerning prognosis as bone alignment and length can be affected.
These types of fractures may permanently injure the growth plate, requiring later treatment to restore alignment of the limb.
Triplane fracture
This fracture is named triplane because it occurs in the coronal, sagittal and axial plane.
It is actually a Salter-Harris type IV.
It is seen exclusively in young adolescents in the period, when the medial tibial epiphysis is closed, while the lateral portion is still open leaving it vulnerable to injury.
As the force cannot continue into the medial part of the growth plate since this is already closed, the epiphysis will fracture.
As in most ankle fractures the mechanism is external rotation.
The injury results in:
- Epiphyseal fracture in the sagittal plane
- Injury to the growth plate in the axial plane
- Metaphyseal fracture in the coronal plane
Study the images and then continue reading.
At first this looks like a Weber B fracture with an oblique fracture in the fibula as seen on the lateral view (black arrows).
Notice however that this fracture line stops at the level of the epiphyseal plate.
So this is the fracture of the metaphysis in the coronal plane.
On the AP-view there is a lucency within the epiphysis, which is the epiphyseal fracture in the sagittal plane.
Notice also that the medial epiphysis is already closed, while the lateral portion is still open(blue arrows).
We have to assume that there is an epiphysiolysis of this lateral portion.
Here another example.
There is only a small metaphyseal fragment, which is usually the case (red arrow).
The fracture through the epiphysis is indicated by the blue arrow.
Maisonneuve fracture
In 1840 Maisonneuve described a frature of the proximal shaft of the fibula, which was caused by exorotation force applied to the ankle.
It is a high Weber C fracture.
These fractures are easily overlooked because the patients rarely complain of pain in the region of the proximal fibula, since the ankle is most painful.
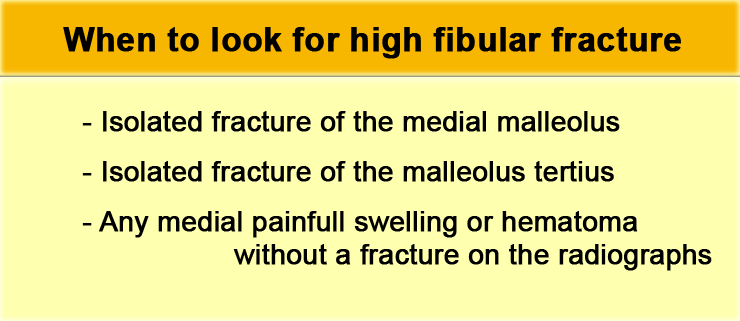
There are three situations in which we should suspect a high Weber C or Maisonneuve fracture:
- Isolated fracture of the medial malleolus
- Isolated fracture of the posterior malleolus without a fracture on the lateral side
- Any painful swelling or hematoma on the medial side without a fracture on the radiographs
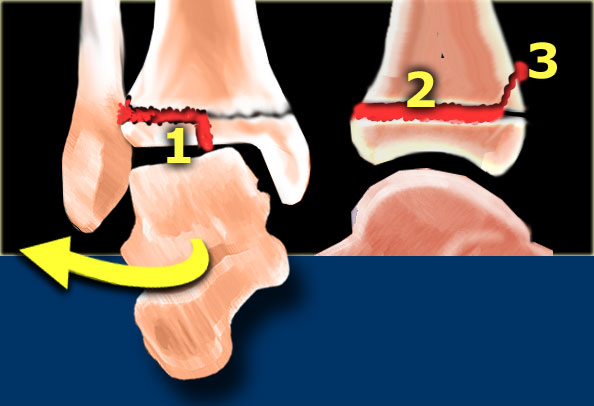
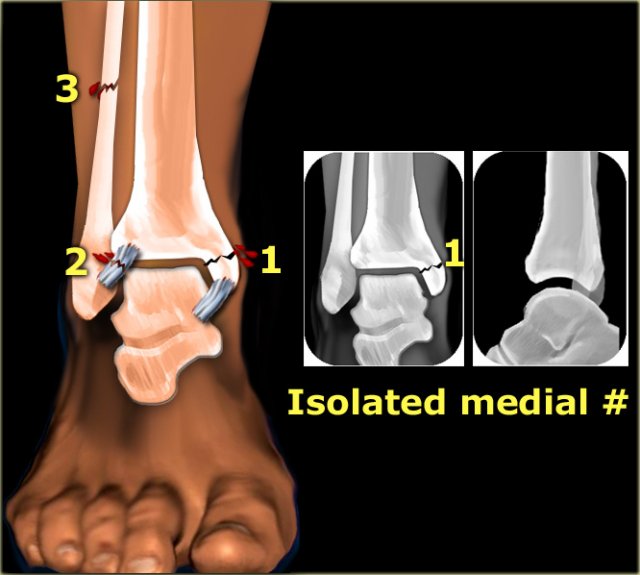
Isolated fracture of the medial malleolus
According to Lauge-Hansen this is the first stage of a pronation exorotation injury, which results in a Weber C fracture.
So we have to look for higher stages.
The injury can continue to the following:
- stage 2: rupture of the anterior syndesmosis
- stage 3: high fibular fracture
- stage 4: rupture of the posterior syndesmosis
In all these subsequent stages, purely ligamentous injury will not be visible on the radiographs of the ankle.
So even in a Weber C stage 4 sometimes only a fracture of the medial malleolus will be visible.
In the illustration we see the fractures and ligamentous injury on the left and the resulting x-rays on the right.
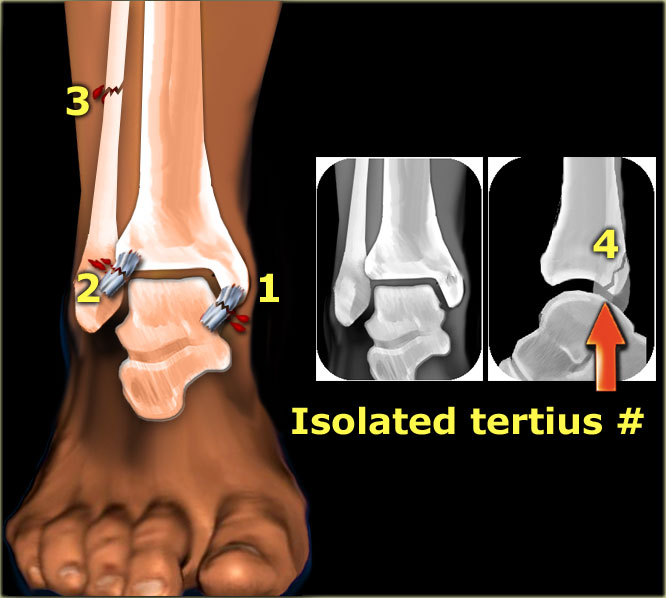
Isolated fracture of the posterior malleolus
Truely isolated fractures of the posterior malleolus are very uncommon.
Most fractures of the posterior malleolus are part of a complex ankle injury, either Weber B or Weber C.
A Weber B fracture is easily detected because of the characteristic oblique fracture.
So if there is a tertiu sfracture and no sign of a Weber B fracture, then we have to start looking for a high Weber C fracture.
In that case we have the following combination:
- stage 1: rupture of the medial collateral ligament stage 2: rupture of the anterior syndesmosis
- stage 3: high fibular fracture
- stage 4: tertius fracture
An isolated tertius fracture on the ankle radiographs indicates the presence of an unstable ankle injury.
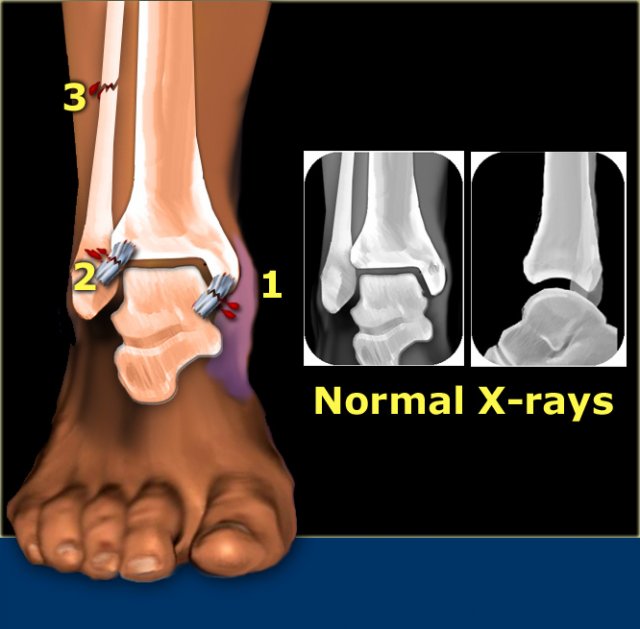
Any medial painful swelling or hematoma
Normal radiographs do not rule out a Weber C fracture.
We may have the following combination:
- stage 1: rupture of the medial collateral ligament, which causes the swelling and hematoma
- stage 2: rupture of the anterior syndesmosis
- stage 3: high fibular fracture - not visible on the radiographs of the ankle
- stage 4: rupture of the posterior syndesmosis
Example 1
On the left images of a patient with a hematoma on the medial side.
- First impression
We can exclude a Weber A or B fracture, because we see no fracture.
A high Weber C is still a possibility, i.e.- medial ligament rupture
- high fibular fracture
- posterior syndesmosis rupture.
- Re-examination
Additional radiographs of the lower leg were taken and demonstrated a high fibular fracture, also known as Maisonneuve fracture. - Final report
Weber C stage 4, i.e. medial collateral ligamentous rupture, rupture of the anterior syndesmosis, high fibular fracture and probably a rupture of the posterior syndesmosis.
This case demonstrates that there can be an unstable ankle injury that needs surgery even when the radiographs of the ankle do not show a fracture.
In any patient with an ankle injury you should always ask yourself the question......can I exclude a high Weber C fracture or do I need additional imaging.
Example 2
- First impression
There is a fracture of the posterior malleolus.
Classification according to Weber is not possible.
An isolated fracture of the posterior malleolus is uncommon, but as part of a supination exorotation (Weber B) or pronation exorotation injury (Weber C) it is quite common.
So we have to re-examine the films to look for signs of a Weber B or C fracture.
- Re-examination
No sign of an oblique fracture of the lateral malleolus, so we can exclude a Weber B fracture.
There is still the possibility of a Weber C fracture, i.e. medial rupture or avulsion, high fibular fracture and finally a posterior malleolar fracture.
Now we notice the subtle avulsion of the medial malleolus (red arrow).
Additional radiographs of the lower extremity demonstrate a high fibular fracture (blue arrow). - Final report
Weber C stage 4.
Example 3
In this case no fracture is seen, but only soft tissue swelling on the medial side.
In such a case, you have to rule out a Maisonneuve fracture, which is a high Weber C fracture.
Additional x-rays of the lower leg were taken.
There is a high fibula fracture.
Tillaux fracture
External rotation injury of the ankle is the most common ankle injury and can lead to a Weber B or Weber C fracture.
One of the first stages in this injury is rupture of the anterior tibiofibular ligament (or anterior syndesmosis).
Less frequently it leads to an avulsion of the anterolateral tibial epiphysis.
Whenever you see such a fracture, you have to look for higher stages of this exorotation injury.
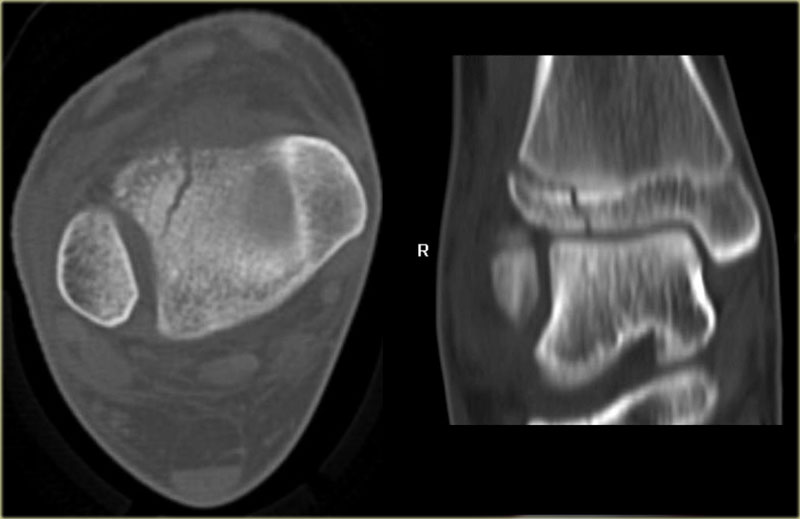
The x-ray shows a subtle Tillaux fracture, which is better appreciated on the CT-images.
Study these images carefully and remember the stages of an exorotation injury.
What is going on here?
There is a Tillaux fracture due to avulsion of the anterolateral part of the distal tibia by the anterior syndesmosis.
This can be a stage 2 of a Weber C fracture.
Stage 1 is rupture of the medial collateral ligaments and stage 3 is a fibula fracture above the level of the syndesmosis.
So now we start looking for stage 4, which is rupture or avulsion of the posterior syndesmosis.
Do you now see the tertius fracture on the axial CT-image?
This patient has an unstable ankle injury and a syndesmotic screw needs to be inserted.
Another Tillaux in a patient with a strange combination of findings. There is an avulsion of the lateral malleolus, a Tillaux and a medial malleolar fracture.
juvenile Tillaux
A Tillaux fracture is more commonly seen in adolescents at the age of 12 -15 years.
At that age it is a fracture through the growth plate and is then called a juvenile Tillaux.
It occurs before the distal tibial epiphysis has completely fused.
The fracture occurs when the medial epiphysis has fused and the lateral part becomes avulsed at the attachment of the anterior tibiofibular ligament (or syndesmosis).
Study the images and then continue reading.
You can enlarge the images by clicking on them.
There is a subtle widening of the lateral part of the growth plate of the right ankle.
There is also a very subtle fracture through the epiphysis.
Continue with the CT.
The CT-images show a epiphysiolysis fracture Salter Harris type 3.
This juvenile Tillaux is especially seen in young athletes.
Always look for higher stages of an exorotation injury.
Charity
All the profits of the Radiology Assistant go to Medical Action Myanmar which is run by Dr. Nini Tun and Dr. Frank Smithuis sr, who is a professor at Oxford university and happens to be the brother of Robin Smithuis.
Click here or on the image below to watch the video of Medical Action Myanmar and if you like the Radiology Assistant, please support Medical Action Myanmar with a small gift.