Trigeminal neuralgia
Loes Braun, Carolien Toxopeus and Robin Smithuis
Antoni van Leeuwenhoek and OLVG hospital in Amsterdam and the Alrijne hospital in Leiderdorp, the Netherlands
Publicationdate
Trigeminal neuralgia is a disorder characterized by recurrent unilateral brief electric shock-like pains, abrupt in onset and termination, limited to the distribution of one or more divisions of the trigeminal nerve.
Several conditions may cause trigeminal neuralgia, but the most common cause is neurovascular compression.
In this article we will discuss the many causes of neuralgia in relation to the anatomical location.
This can help you to systematically study all the important regions in the course of the trigeminal nerve.
Introduction
The pathology of the trigeminal nerve is related to the location.
In the illustration the five different segments of the trigeminal nerve are presented, which will be discussed in more detail in the following chapters.
Brainstem: trigeminal nucleus
- Demyelinisation: MS
- Neoplasm: metastases, glioma
- Vascular: cavernoma, infarction, AVM
- Infection:
rhombencephalitis
Cisternal segment
- Neurovascular compression
- Neoplasm: schwannoma, meningioma, epidermoïd, perineural spread
- Infection
/ inflammation: neuritis, meningitis, apicitis (from the petrous bone)
Meckel's cave
- Neoplasm: schwannoma, meningioma,
epidermoïd, perineural spread, skull base lesion.
Cavernous segment
- Neoplasm: schwannoma, meningioma, metastasis, perineural spread, skull base lesions
- Vascular: aneurysm
- Infection
/ inflammation: Tolosa-Hunt
Peripheral segment
- Neoplasm: perineural spread, schwannoma, neurofibroma
- Infection / inflammation: sinonasal
Brain stem segment
Pathology in the
brain stem segment is most often due to demyelination by multiple
sclerosis.
Other types of pathology in the brain stem segment are neoplasms
(mostly glioma and metastases), vascular lesions (infarction, cavernoma) and
infections (rhombencephalitis).
The trigeminal nerve originates from two separate nuclei in
the pons: the sensory division from the sensory nucleus (green dot) and the motor division
from the motor nucleus (red dot).
This first part is called the brain stem segment.
From these nuclei, the trigeminal nerve courses anteriorly, to the ventrolateral surface of the pons to continue with the cisternal segment in the prepontine cistern.
The trigeminal nerve is the largest of all cranial nerves.
It consists of a sensory and a motor division.
The sensory division – which is the largest of the two – innervates sensibility in the whole face.
The smaller motor division innervates:
- masticator muscle
- temporalis muscle
- pterygoid muscles
- mylohyoid muscle
- anterior belly of the digastric muscle,
- tensor veli palatine muscle
- tensor tympani muscle.
The sensory nucleus is situated laterally in the tegmentum, anterolateral to the fourth ventricle (green dot).
The motor nucleus is situated anteromedial to the sensory nucleus (red dot).
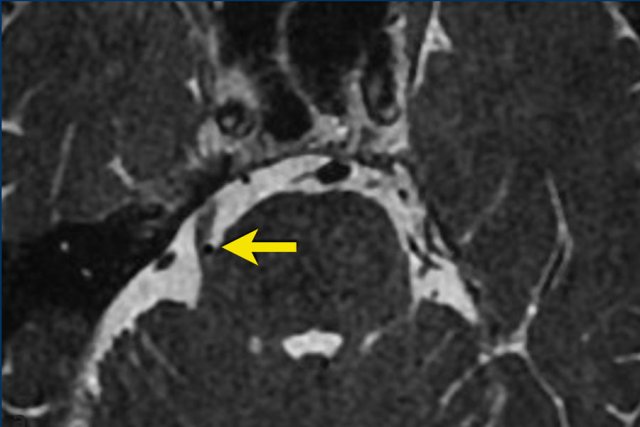
This image is of a 26 year old male who developed slowly progressive facial hypesthesy on the right.
The axial T2W image shows a hyperintense lesion at the
trigeminal nucleus (arrow).
This may be a sign of demyelinsation, for
instance in multiple sclerosis
Cisternal segment
The cisternal segment is – almost without exception - the source of a true trigeminal neuralgia caused by neurovascular compression.
Other causes of pathology in the cisternal segment causing trigeminal neuropathy are far less common, like neoplasms, mostly schwannoma, meningioma and epidermoid.
Furthermore, the cisternal segment may be subject to infection or inflammation, for instance trigeminal neuritis.
Neurovascular compression
Neurovascular compression is defined by specific radiologic criteria:
- The blood vessel concerned is almost always an artery
- The nerve and the blood vessel run perpendicular to each other
- There is mass effect of the vessel on the nerve
- The contact between blood vessel and nerve occurs in the root entry zone of the nerve.
Neurovascular compression of the trigeminal nerve is most often caused by contact with the superior cerebellar artery (SCA) or less frequently the anterior inferior cerebellar artery (AICA), or smaller branches of the basilar artery.
Only a few cases have been reported in which neurovascular compression was caused by contact with an aneurysm, vertebrobasilar dolichoectasia, an AVM, an AV-fistula or even a vein.
Root entry zone
The cisternal segment starts where the trigeminal
nerve enters the prepontine cistern.
This is called the root entry zone.
The root entry zone comprises the transition zone from central
myelin (oligodendrocytes) to peripheral myelin (Schwann cells).
This transition zone measures approximately 2 mm long and is situated at approximately 5-7 mm from the surface of the pons.
At this point, the nerve is vulnerable to pressure.
In the prepontine cistern, the sensory and motor divisions have a parallel but separate course, creating a characteristic fan-like appearance (arrow).
A 74 year old male has been experiencing
an ‘220V-like’ pain in his right eyebrow, cheek and mandible.
These symptoms are
evoked by washing his face and brushing his teeth.
Scroll through the axial 3D FIESTA images and the postcontrast axial 3D T1W images. Then continue reading.
Both the axial 3D FIESTA and postcontrast axial 3D T1W
images show:
- A close relationship between the right trigeminal nerve (arrow) and the superior cerebellar artery (dashed arrow)
- Located at the root entry zone of the nerve
- The nerve and the vessel course perpendicular to each other
- The nerve is displaced laterally
These findings fulfill the criteria for a neurovascular compression.
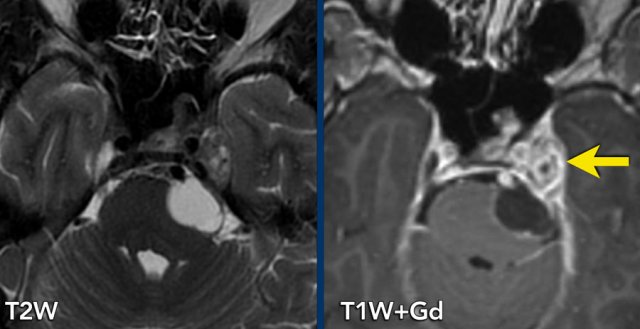
These images are of a 49-year old male with sensory problems in the left side of his face and pressure behind his left eye.
The axial T2W shows
a lesion in Meckel’s cave and the cisternal segment of the trigeminal nerve.
The component in Meckel’s cave is solid and shows homogeneous enhancement on
post-contrast T1W imaging (arrow).
The component in the cerebellopontine cistern is
almost completely cystic and shows only rim enhancement.
The lesion is a
trigeminal schwannoma.
The growth of this lesion along the nerve, leading to
a constriction at the entrance of Meckel’s cave, causes the classic ‘dumbbell
shape’.
Meckel's cave segment
Pathology in Meckel’s cave leading to trigeminal neuropathy, mostly concerns neoplasms, either primary, secondary or extrinsic.
Primary lesions, originating from the nerve itself, are mostly schwannomas, meningeomas, and epidermoids.
Secondary neoplasms – involving the nerve, but not originating from it - are mostly based on perineural spread. The spread can be retrograde (from the peripheral branches) or antergrade (from the cisternal segment).
Extrinsic lesions mostly originate from the skull base.
After traversing the cerebellopontine and prepontine
cisterns, the trigeminal nerve enters Meckel’s cave, which forms the third
segment.
In Meckel’s cave the trigeminal ganglion is located also known as Gasser’s or semilunate ganglion.
At the ganglion, the sensory division of the trigeminal nerve divides into three parts:
- ophthalmic nerve (nV1)
- maxillary nerve (nV2)
- mandibular nerve (nV3)
The motor division does not pass through the ganglion, but rather underneath it. Together with nV3, the motor division leaves the
intracranial compartment via the foramen ovale.
A 45 year-old
female with a history of pain on the right side of the mandible, alleviated
by extraction of multiple dental elements.
However, since one month, she is
experiencing the same type of pain once more. The pain is sharp and radiates
from the chin, via the right side of the face to the skull. The pain is
evoked by talking, eating, and touching the right sides of the face.
Image
3D FIESTA shows
a lesion in Meckel’s cave, hyperintense on DWI, hypo-intense on ADC (not
shown), extending into the cisternal segment.
This lesion is
suspicious for an epidermoid.
Cavernous segment
Primary lesions originating from the cavernous segment itself are quite rare.
These lesions – mostly schwannomas, meningeomas
and epidermoids – usually originate from the third segment, extending into the cavernous sinus.
Trigeminal lesions in the cavernous segment are mostly secondary due to perineural spread or
metastases.
Furthermore, pathology of the cavernous segment may be due to extrinsic lesions, for instance lesions originating from the skull base, the meninges or vascular structures, for instance carotid aneurysms.
Moreover, the cavernous segment may be subject to infectious or inflammatory pathology, for instance Tolosa-Hunt syndrome, which is a severe unilateral periorbital headache associated with painful and restricted eye movements.
The first two
branches of the trigeminal nerve – the ophthalmic nerve and the
maxillary nerve – continue their course from Meckel’s cave into the
cavernous sinus.
The course of the ophthalmic nerve is quite long and follows the lateral wall of the sinus.
The course of the maxillary nerve is much shorter
and follows the caudal border.
Some sources even state that the maxillary
nerve does not pass through the
sinus at all, but rather underneath
it.
67- year old female with a history of breast cancer with metastases to bone and liver. She presents with numbness on the left side of her face.
Axial 2D FLAIR
show an asymmetric cavernous sinus, with dural thickening on the left.
Post-contrast imaging shows increased enhancement of the left side of the
cavernous sinus, extending into Meckel’s cave.
Suspicious for metastasis of breast carcinoma.
Peripheral segment
Pathology of the peripheral branches of the trigeminal
nerve mostly concerns perineural spread from malignancies in the head and neck
region.
Due to its extensive branching pattern, the trigeminal nerve is especially
vulnerable to this type of pathology. Perineural spread may be recognized as
thickening and enhancement of the nerve, mostly – but not exclusively - in
retrograde direction.
Furthermore, the peripheral branches may be subject to primary neoplasms, mostly schwannomas or neurofibromas.
Moreover, the peripheral branches may be affected by infectious or inflammatory processes, mostly neuritis originating from the paranasal sinuses.
Ophtalmic nerve
The nV1 leaves the cavernous sinus through the superior
orbital fissure and enters the orbit. It subdivides into three smaller
branches. The main branch continues its course via the supra-orbital foramen to
form the supra-orbital nerve.
Maxillary nerve
The nV2 leaves the cavernous sinus via the foramen rotundum
and enters the pterygopalatine fossa. There, the nerve subdivides into four
smaller branches. The main branch continues via the infra-orbital foramen into
the orbit and via the infra-orbital canal into the face to form the infra-orbital
nerve.
Mandibular nerve
The nV3 does not pass through the
cavernous sinus. Instead it leaves Meckel’s cave – together with the motor
division – via the foramen ovale and enters the infratemporal fossa. There, it
subdivides into four smaller branches.
The main branch – the inferior alveolar
nerve – continues its course via the mandibular foramen into the mandible and
through the mandibular canal and the foramen mentale into the face to form the
mental nerve. After entering the infratemporal fossa, the motor
division subdivides into two smaller branches: the masticator nerve and the
mylohyoid nerve.
70 year old male with a history of melanoma and orbital exenterition. Recently, he has been experiencing tingling and numbness in the left side of his face. These symptoms cannot be evoked and respond well to pain medication.
Scroll through the axial and coronal postcontrast 3D T1W images. Then continue reading.
Axial and coronal postcontrast 3D T1W images show thickening and enhancement of nV1 in the supra-orbital fissure (a and b, arrow), nV2 in the foramen rotundum (a and b, dashed arrow), and nV3 in the foramen ovale (c and d, arrow).
These abnormalities are suspicious for perineural spread of melanoma.
Click on the image below and watch the video of Medical Action Myanmar of Dr Frank Smithuis, who is the brother of Robin Smithuis.
If you like the Radiology Assistant please donate to Medical Action Myanmar.