Crohn's disease - role of MRI
Carl Puylaert, Jeroen Tielbeek and Jaap Stoker
the Academic Medical Centre, Amsterdam, the Netherlands
Publicationdate
In this article we will discuss the MRI-features used to evaluate Crohn's disease of the small bowel and the colon.
A systematic approach is presented to grade disease activity resulting in a simple classification of mild, moderate and severe disease.
This is sufficient for most therapeutic decisions.
Introduction
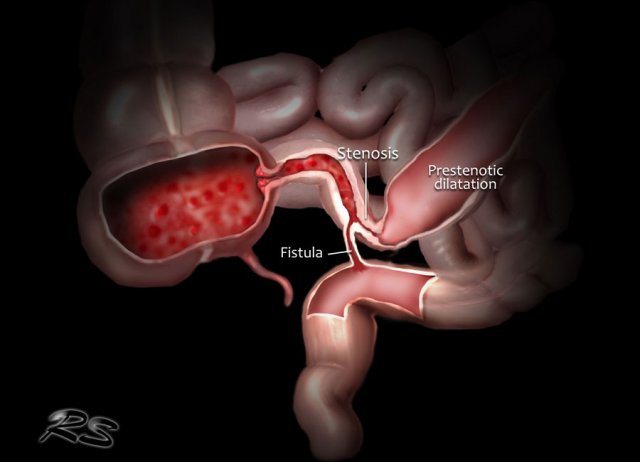
Crohn's disease is characterized by inflammatory lesions in the gastrointestinal tract, most commonly in the terminal ileum and colon.
The lesions are usually transmural, which can lead to complications like stenoses, fistulas and abscesses.
While most patients first present with inflammation only, about two thirds of patients will develop complications within 10 years (1).
There is no cure for Crohn's disease.
Immunosuppressive drugs can decrease disease activity, maintain remission and prevent relapse.
Eventually 90% of patients with ileocolic disease require surgery (2).
MRI protocol
Bowel distention
There are two techniques to acquire distension of the small bowel:
- MR enterography: oral administration of contrast.
- MR enteroclysis: administration of contrast via a nasojejunal tube.
We routinely perform MR enterography as it suffices in the large majority of patients while being less burdensome and more time efficient.
Oral contrast
For oral contrast several options are available.
We use a Mannitol in water solution (2%), which provides good contrast between lumen and bowel wall on both T1 and T2 sequences and is well accepted by patients.
There is one precaution: no colonoscopy with electrocoagulation should be performed directly after the MRI because of methane resulting from Mannitol breakdown.
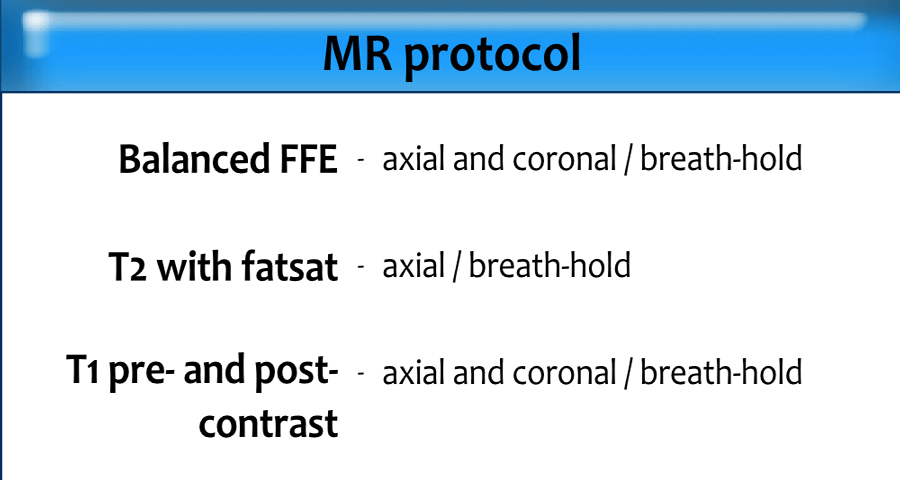
MRI sequences
We use the following sequences:
- Balanced FFE (axial and/or coronal) in breath-hold
- T2 with fat sat (axial) in breath-hold
- T1 pre- and post-contrast (axial/coronal) in breath-hold
Optional sequences:
- T2-FSE without fat sat for additional overview and comparison with T2 with fat sat.
- Diffusion Imaging (DWI).
- Balanced FFE cine-study for motility.
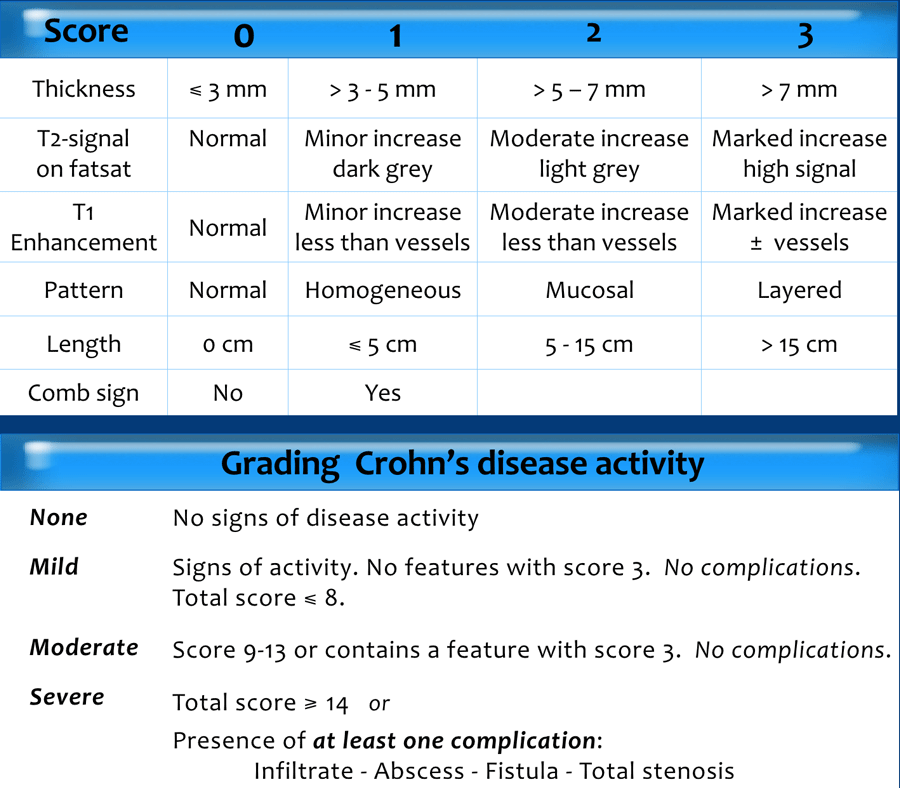
Grading Crohn's disease activity
There are several systems for grading disease activity in Crohn's disease.
The scoring system, that we use, grades disease activity into none, mild, moderate and severe.
It is based on the score of the bowel wall abnormalities and the presence of complications as presented in the table (3).
Additional findings
Other findings that should be mentioned in the radiology report are:
- Location of the lesions
- Exact wall thickness
- Length of the disease
- Ulcerations
- Comb sign
- Creeping fat
- Loss of haustration of the colon
- Partial stenosis
- Sinus tracts
MRI signs of Crohn's disease
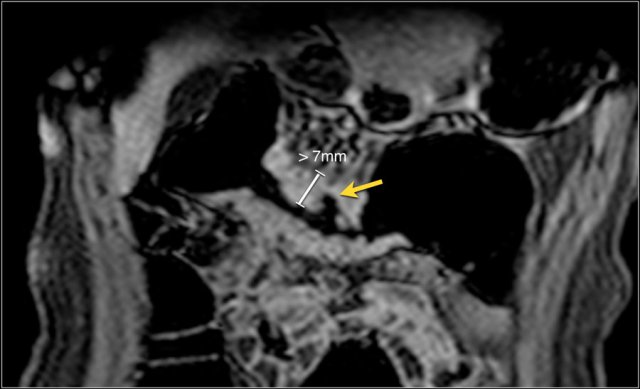
Bowel wall thickness
With adequate distension the normal bowel wall has a thickness of 1-3 mm.
A common categorization is 3-5 mm for mild thickening, 5-7 mm for moderate thickening and > 7 mm for marked thickening of the bowel wall.
T1 weighted post-contrast images or non fatsat T2 weighted images (if available) are preferable for measurement of bowel wall thickness.
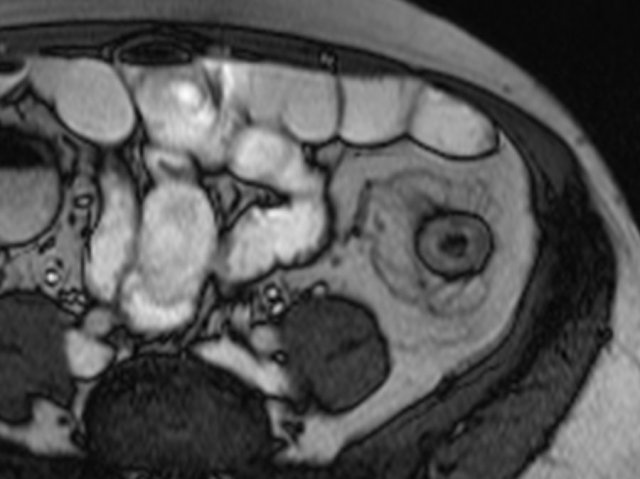
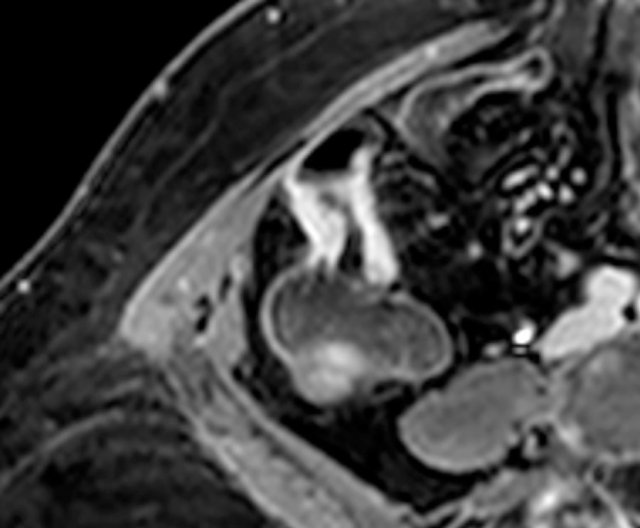
The image is a coronal post-contrast T1 weighted image showing disease activity in the transverse colon with marked wall thickening of more than 7 mm and deep ulceration (arrow).
 Balanced FFE image shows marked bowel wall thickening and luminal narrowing of the terminal ileum. Measurement on the balanced FFE sequence can be less accurate due to the black border artifact (arrows).
Balanced FFE image shows marked bowel wall thickening and luminal narrowing of the terminal ileum. Measurement on the balanced FFE sequence can be less accurate due to the black border artifact (arrows).
Increased bowel wall thickness is one of the most common signs of inflammatory activity, but not specific for Crohn's disease.
For more information on the differential diagnosis of bowel wall thickening click here.
Bowel wall thickness correlates well with the severity of the disease activity.
Measurements are best performed on the sequence with good luminal distension.
Black border artifacts on balanced FFE sequences can distort thickness measurements.
 Thickened terminal ileum segment with marked enhancement on axial post-contrast T1W image with fatsat.
Thickened terminal ileum segment with marked enhancement on axial post-contrast T1W image with fatsat.
Enhancement
Abnormal bowel wall enhancement after administration of gadolinium is the result of increased vascular permeability and angiogenesis.
It is seen both in active disease and fibrosis.
Enhancement can be graded by comparing to the precontrast images, to normal bowel loops and nearby vascular structures.
- No abnormal enhancement
Equivalent to normal bowel wall - Minor increased enhancement
More than normal bowel wall, but significantly less than nearby vascular structures - Moderate enhancement
Somewhat less than nearby vascular structures - Marked enhancement
Equal or more intense than nearby vascular structures
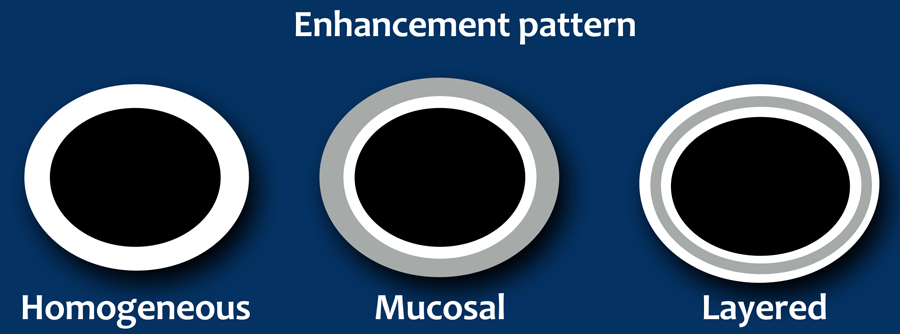
Pattern of enhancement
Enhancement of the bowel wall can be categorized in one of the following patterns:
- Homogeneous
- Mucosal
- Layered
The latter two enhancement patterns can only be appreciated when the wall is thickened.
There is some discussion about the value of the enhancement pattern.
A layered pattern is regarded to depict more severe disease activity compared to the mucosal pattern, which in turn is more severe than a homogeneous pattern (4).
However, different degrees of inflammation and fibrosis can be present at the same time and a layered pattern of enhancement has also been associated with fibrosis (5), although a more recent study did not find this association (6).
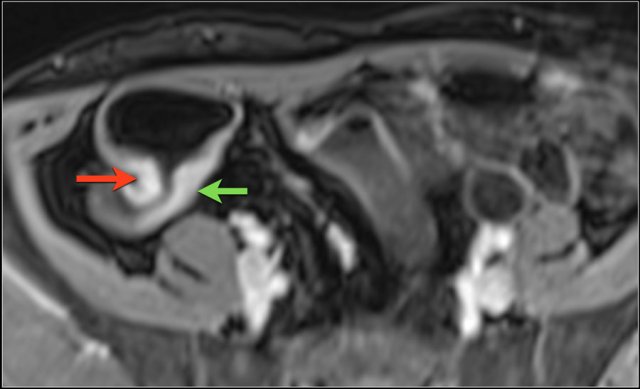
Homogeneous enhancement
Strong homogeneous enhancement is seen in active inflammation.
The image shows a terminal ileum with a homogeneous enhancement pattern with moderate (green arrow) and marked (red arrow) enhancement on an axial post-contrast T1 image.
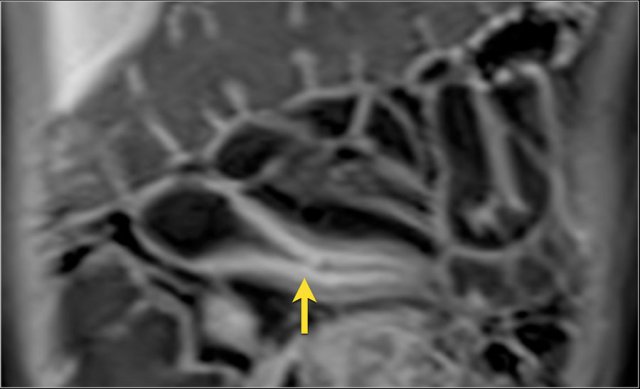
Mucosal enhancement
This is seen as bowel wall thickening with increased enhancement of the mucosal layer relative to the outer layers.
The image is a post-contrast T1 image with a mucosal enhancement pattern in the terminal ileum (arrow).
There is relatively low enhancement of the middle and outer layers
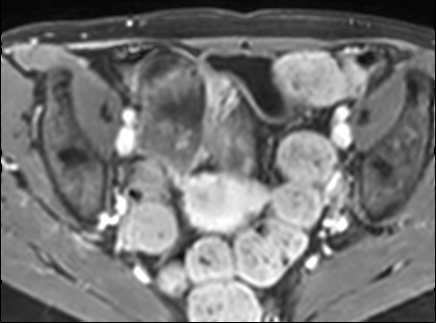
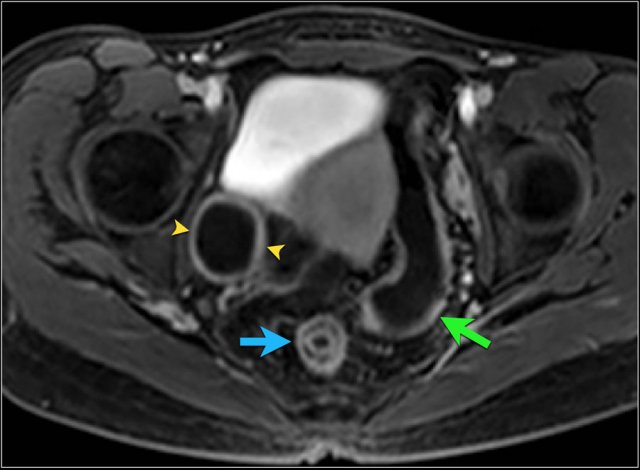 Layered enhancement pattern of the rectum with some surrounding fat stranding on an axial post-contrast T1 image (arrow). Continued inflammation with a homogeneous enhancement pattern can be seen in the sigmoid colon (green arrow). Also, a right-sided adnexal cyst is present with enhancing rim (arrowheads).
Layered enhancement pattern of the rectum with some surrounding fat stranding on an axial post-contrast T1 image (arrow). Continued inflammation with a homogeneous enhancement pattern can be seen in the sigmoid colon (green arrow). Also, a right-sided adnexal cyst is present with enhancing rim (arrowheads).
Layered enhancement pattern
This pattern suggests severe disease activity or longstanding chronic disease (4,5).
The three-layered appearance is caused by strong enhancement of the mucosa and the serosa with no enhancement of the middle layer, which is the submucosa and the muscular layer.
This middle layer can consist of fat, edema or fibrotic tissue.
This can be distinguished using a fat sat T2 sequence.
 Actively inflamed terminal ileum with marked thickening and moderate mural signal intensity (mural edema) on an axial T2 with fat sat.
Actively inflamed terminal ileum with marked thickening and moderate mural signal intensity (mural edema) on an axial T2 with fat sat.
T2 mural signal intensity
Increased mural signal intensity on fat-saturated T2 images indicates the presence of mural edema, suggesting active disease.
Presence of bowel wall thickening with a low mural T2 signal intensity is more suggestive of fibrotic disease.
The psoas muscle can be used as a reference when assessing mural T2 signal.
Fat suppression is routinely used to differentiate between mural fat depositions and mural edema.
Fat depositions are the result of chronic bowel inflammation and therefore quite common in Crohn's disease.
However, its presence does not indicate active disease.
Perimural edema or fluid can be identified as well and is associated with active disease (7).
 Inflamed small bowel showing wall thickening and mild mural T2 signal (arrow) on an axial T2 with fat sat. Prestenotic dilatation can be seen proximally of the diseased segment.
Inflamed small bowel showing wall thickening and mild mural T2 signal (arrow) on an axial T2 with fat sat. Prestenotic dilatation can be seen proximally of the diseased segment.
T2 mural signal intensity can be graded as follows using a T2 sequence with fat sat:
- No increase
normal bowel wall - Minor increase
bowel wall appears dark gray - Moderate increase
bowel wall appears light gray - Marked increase
bowel wall contains areas of white high signal approaching that of luminal content.
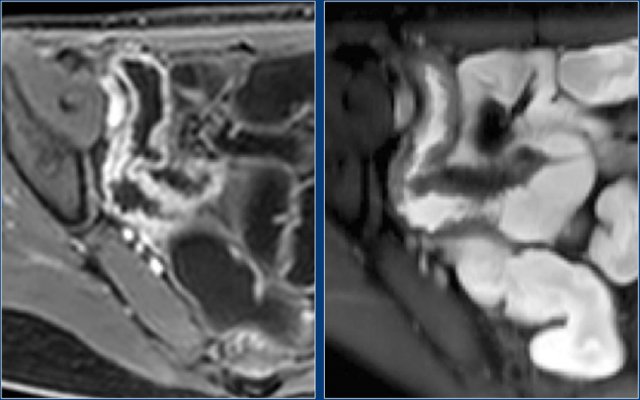
 Wall thickening of the terminal ileum in a 67-year-old male with Crohn's disease since 11 years. Layered enhancement is seen on an axial post-contrast T1 image with fat sat (left). T2 with fat sat (middle) shows the same pattern with a middle layer of low intensity. T2 without fat sat shows an increased signal in the middle layer, suggesting fat depositions. Endoscopy showed only superficial disease.
Wall thickening of the terminal ileum in a 67-year-old male with Crohn's disease since 11 years. Layered enhancement is seen on an axial post-contrast T1 image with fat sat (left). T2 with fat sat (middle) shows the same pattern with a middle layer of low intensity. T2 without fat sat shows an increased signal in the middle layer, suggesting fat depositions. Endoscopy showed only superficial disease.
Fat suppression is routinely used to differentiate between mural fat depositions and mural edema.
Fat depositions are a result of chronic bowel inflammation, but not typical of active disease.
These fat depositions can be diffuse but can also present as a layered pattern.
The CT equivalent for this pattern is the 'fat-halo sign'.
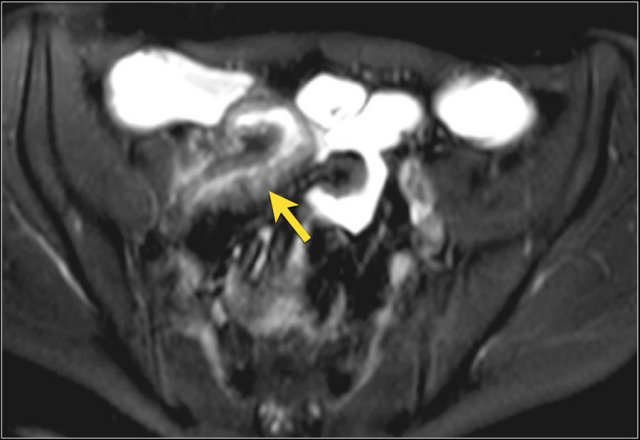
 Coronal post-contrast T1 and T2 fat sat images show multiple small ulcerations in the terminal ileum.
Coronal post-contrast T1 and T2 fat sat images show multiple small ulcerations in the terminal ileum.
Ulceration
Moderate to deep ulceration can be seen on T1 and T2 images, but small ulcerations can be difficult to distinguish from mucosal folds depending on the degree of luminal distension.
Ulcerations are active spots of inflammation and usually there is increased enhancement on the post-contrast T1 images.
Loss of haustration
When the colon is involved in Crohn's disease a decrease of haustral folds can be seen.
A complete loss of haustration results in a smooth surface.
This is also a common finding in ulcerative colitis and known as 'lead pipe' colon.
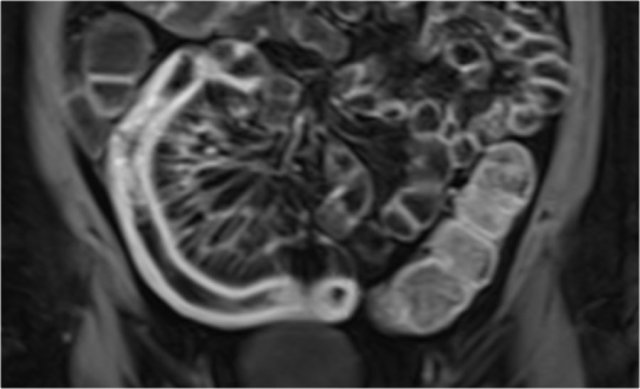
The coronal post-contrast T1 image shows loss of haustral folds throughout the colon in a patient with chronic Crohn's disease.
 Coronal post-contrast T1 image shows marked enhancement of the terminal ileum with a prominent comb sign.
Coronal post-contrast T1 image shows marked enhancement of the terminal ileum with a prominent comb sign.
Comb sign
Increased vascularity of the mesentery is seen in active inflammation.
The engorged vessels have a linear appearance, resembling the teeth of a hair comb (comb sign).
Creeping fat
Creeping fat, also called fibrofatty proliferation or fat wrapping, are different names for hypertrophy of the subserosal fat.
It is a common finding in longstanding Crohn's disease.
The image shows creeping fat surrounding the descending colon.
It isolates the colon from surrounding bowel loops.
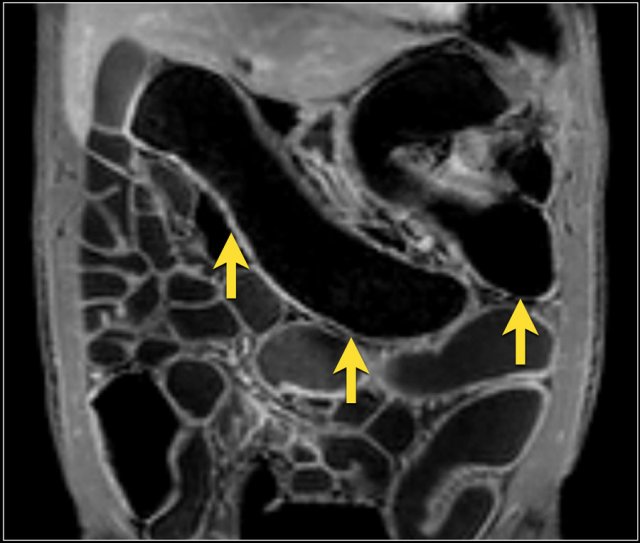
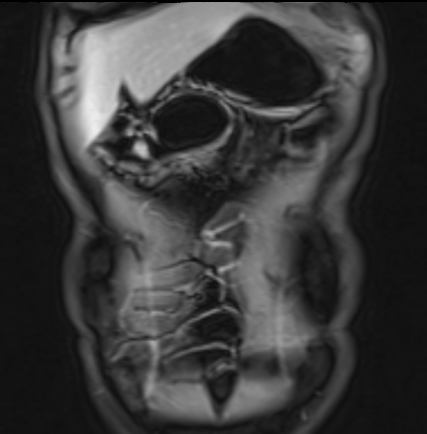
Skip lesions
Skip lesions and patchy inflammation are a typical finding in Crohn's disease, in contrast to the continuous inflammation, which is seen in ulcerative colitis.
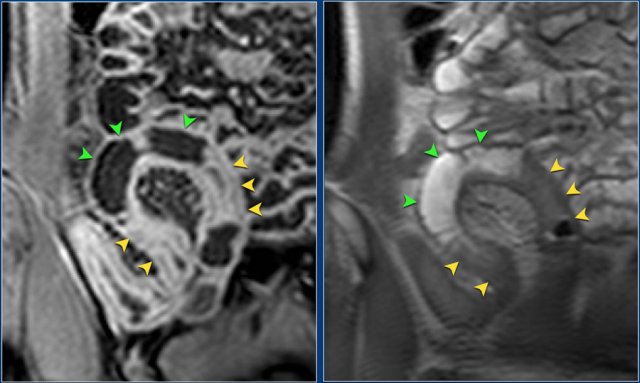
Skip lesions refers to the interspersed inflammation "skipping" parts of the bowel, which are left unaffected (green arrows).
The coronal T1 post-contrast image (left) and the T2 image (right) show skip lesions in the terminal ileum.
The affected lesions show increased enhancement with a layered pattern (yellow arrows), while another part is unaffected or skipped (green arrows).
Complications
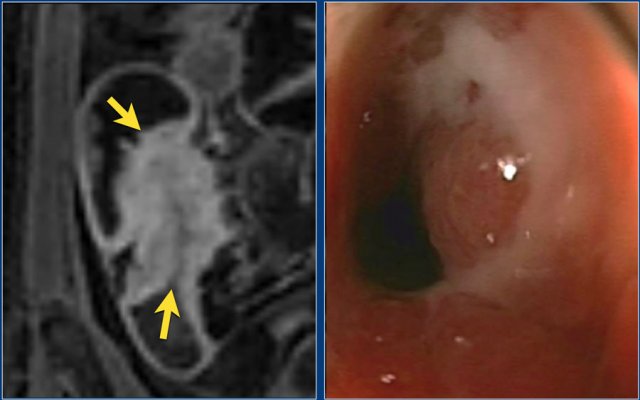 Coronal post-contrast T1 image with a stenosis at the ileocecal junction (left). No obvious pre-stenotic dilatation is seen. The stenosis was non-passable using endoscopy (right).
Coronal post-contrast T1 image with a stenosis at the ileocecal junction (left). No obvious pre-stenotic dilatation is seen. The stenosis was non-passable using endoscopy (right).
Stenosis
Stenosis can present as bowel wall thickening combined with lumen narrowing.
The presence of a prestenotic dilatation increases the likelihood of a stenosis.
Abnormal contrast enhancement of the affected bowel segment is usually present.
In the grading system, only severe stenosis is included as a complication, which is defined as a stenosis with prestenotic dilatation and a moderate-to-marked increase in mural T2 signal.
Narrowing can be due to contraction and therefore check other sequences before making the diagnosis of a stenosis.
There may be a role for motility sequences to demonstrate the presence or absence of motility to differentiate a contraction from a stenosis.
The video shows a motility sequence (BTFE dynamic) showing wall thickening in the cecum and terminal ileum.
There is some decreased motility in the terminal ileum, but there is no stenosis.
A 48-year-old female, who was under anti-TNF treatment, underwent a colonoscopy.
In the sigmoid colon, a stenosis was seen, which could not be passed.
MR-enterography was performed to examine the extension of the stenosis.
Scroll through the images.
The small bowel is normal, but stenotic segments are seen in the descending and transverse colon.
Both stenotic segments display wall thickening up to 8 mm and marked enhancement with a mucosal pattern in the descending colon and a layered pattern in the transverse colon.
A prestenotic dilatation is seen before both segments.
Since these stenoses were not present at a colonoscopy before anti-TNF treatment, they had most likely developed during the treatment.
Therefore it was decided to perform a subtotal colectomy with an ileosigmoïdal anastomosis.
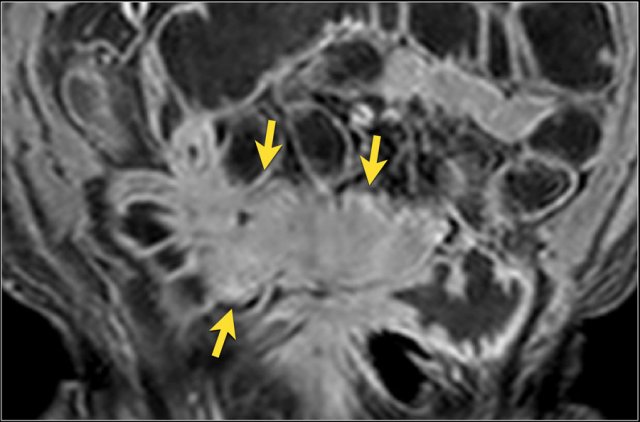
Infiltrate
Infiltrate can be seen as creeping fat between bowel loops with replacement of the fat signal intensity and tethering and kinking of bowel loops.
Obstructive symptoms due to adhesions, inflammatory narrowing or fibrosis are common.
Fistulas and abscesses are often present.
Due to the complex structure, the exact path of a fistula can be difficult to define.
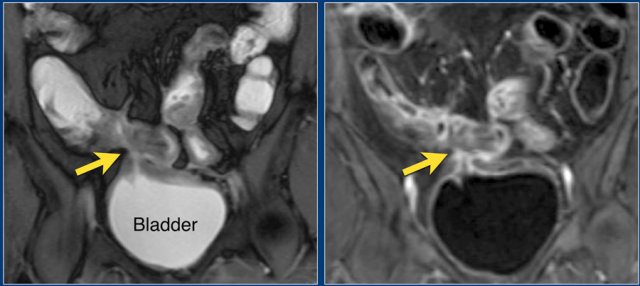 Coronal Balanced FFE image shows an enterovesical fistula (arrow) originating from the small bowel. Post-contrast T1 image shows marked enhancement of the small bowel and the 'tram track' at the site of the fistula.
Coronal Balanced FFE image shows an enterovesical fistula (arrow) originating from the small bowel. Post-contrast T1 image shows marked enhancement of the small bowel and the 'tram track' at the site of the fistula.
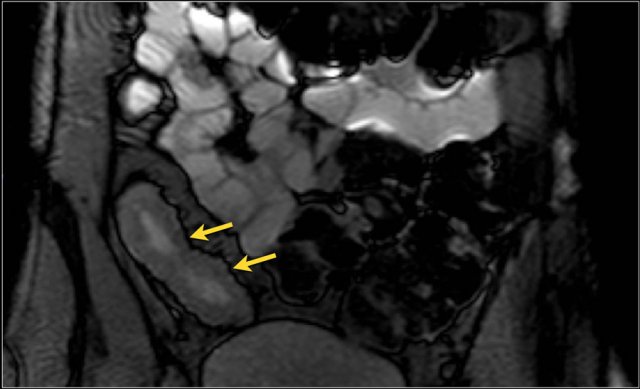
Fistula
Sinus tracts and fistulas are common complications in patients with Crohn's disease.
Both show marked enhancement on T1 images after administration of gadolinium.
A fistulous track can present with a layered 'tram track' configuration or as a linear enhancing structure.
It can be seen going from one bowel loop to another bowel loop, to another hollow organ or to the skin.
A 50 year-old female with Crohn's disease since 10 years presented with bloody diarrhea and underwent a MR-enterography and a colonoscopy.
At colonoscopy, a normal colon was seen, but the ileocecal valve was stenotic.
Scroll through the images.
Severe disease activity can be seen at the terminal ileum with presence of multiple fistulas.
This examination prompted the gastro-enterologist to start anti-TNF treatment.
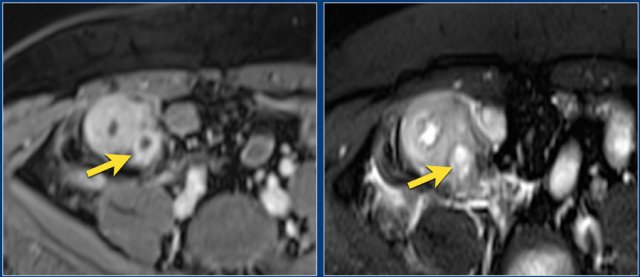 Small abscess medioposterior from thickened and inflamed terminal ileum. Note the rim enhancement on the post-contrast T1 image (upper) and marked mural signal on the fat sat T2 image (lower)
Small abscess medioposterior from thickened and inflamed terminal ileum. Note the rim enhancement on the post-contrast T1 image (upper) and marked mural signal on the fat sat T2 image (lower)
Abscess
Abscesses are often seen in patients with severe active Crohn's disease.
Abscesses are characterized by rim enhancement on post-contrast T1 images and central high signal intensity on T2 images.
The abscess is frequently surrounded by fat stranding.
Diffusion Imaging
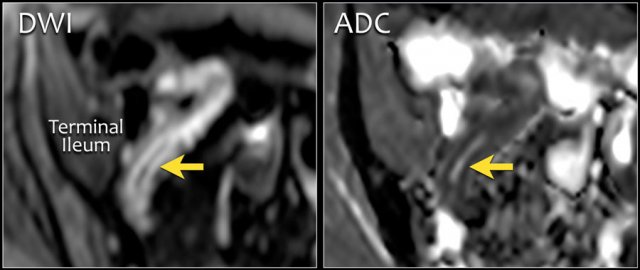 Crohn's disease of the terminal ileum with high signal on axial DWI and low signal on ADC map indicating diffusion restriction (b=600).
Crohn's disease of the terminal ileum with high signal on axial DWI and low signal on ADC map indicating diffusion restriction (b=600).
Diffusion Imaging
Bowel inflammation, fistulas and abscesses show restricted diffusion -high on DWI, low on ADC.
B values of 600 - 1000 are most commonly used.
Maybe DWI can replace contrast-enhanced series, but its role is not defined yet.