CT-pattern of Bowel wall thickening
Richard Gore and Robin Smithuis
Professor of Radiology, University of Chicago, Evanston, IL, USA and the Rijnland hospital in Leiderdorp, the Netherlands
Publicationdate
This article is based on a presentation given by Richad Gore and adapted for the Radiology Assistant by Robin Smithuis.
Richard Gore is editor of the Textbook of Gastrointestinal Radiology, 3rd Edition and High Yield Imaging: Gastrointestinal.
We will discuss a pattern approach to patients with bowel wall thickening with special attention to the CT-enhancement patterns.
Introduction
Bowel wall thickening is a common finding in imaging.
CT can be helpful in the differentiation of intestinal disease.
Important features to look for are:
- Enhancement pattern
- Length of involvement
- Degree of mural thickening
- Patency of the mesenteric vessels
- Mesenteric changes
- Lumen contents
All these features will be discussed in detail in the following paragraphs.
Lenght of bowel wall involvement
- < 5 cm involvement
Adenocarcinoma usually presents as a short segment of bowel wall thickening. The borders are shouldering unlike in diverticulitis, where the borders are tapering (figure). - 5-10 cm involvement
Diverticulitis, Crohn's disease and ischemia usually present as a somewhat longer segment of involvement. - 10-30 cm involvement
See the list in the table. The image shows a submucosal hemorrhage. This is mostly seen in the small bowel and duodenum. - Diffuse involvement
When the entire colon is involved think of ulcerative colitis.
Involvement of both the colon and the small bowel is seen in infectious bowel disease (IBD), edema and SLE.
Overview of enhancement pattern
The figure shows an overview of the CT-patterns of mural enhancement in patients with bowel wall thickening.
Click to enlarge.
Type 1 - White Attenuation
There are many pathophysiologic events that can cause a white attenuation pattern:
- Bright enhancement of the bowel wall is seen in vasodilatation in acute inflammatory bowel disease.
- Injury to the intramural vessels with interstitial leakage in shock bowel. Hypoperfusion results in increased permeability and increased enhancement.
- Intramural hematoma is seen in trauma and treatment with anticoagulation.
The normal bowel will enhance bright especially if the scan is in the late arterial phase, i.e. 35-40 seconds post injection.
If the bowel wall is not thickened, this is normal enhancement.
When there is bright enhancement in thickened bowel, it is sometimes difficult to differentiate between the white enhancement pattern and the water-target-sign pattern.
Acute IBD
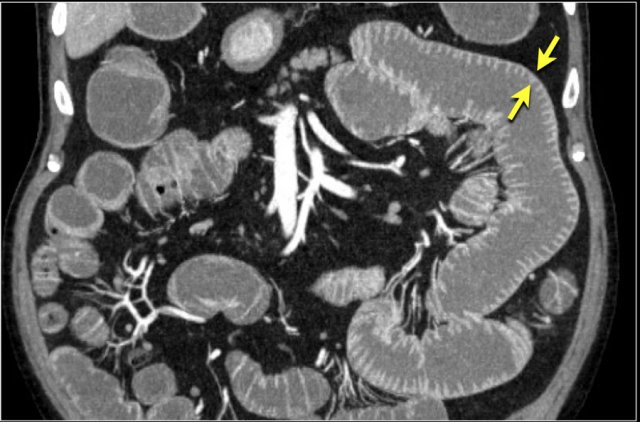
Here a patient with acute inflammatory bowel disease (IBD).
Notice the bright enhancement of a large segment of the small bowel with a thickened wall.
This is the result of hyperemia due to the vasodilatation.
Notice the dilated vessels on the ventral side.
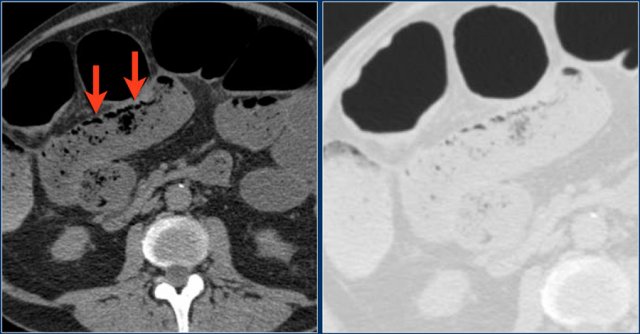
Shock Bowel
In patients with a hypovolemic shock, there is a redistribution of the blood flow.
This can result in abnormal bright enhancement of the bowel wall like in this case of a patient who is in a hemorrhagic shock.
Notice that some bowel loops show a white pattern, while others show a water target sign.
The slit-like inferior vena cava is due to the hypovolemia (red arrow).
As a result of redistribution of bloodflow to vital organs, these patients can have hyperenhancing adrenal glands, as these organs are needed to produce adrenaline in order to manage the shock.
Type 2 - Gray Attenuation
In the gray-pattern, the bowel wall is thick and despite a nice bolus of contrast there is poor enhancement and you can not see the different layers of the bowel wall.
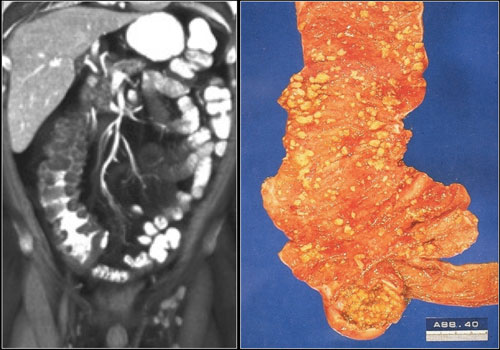
This pattern is seen in chronic fibrotic Crohn's disease, ischemia and neoplasms like adenocarcinoma and lymphoma.
Chronic Crohn's disease
Here a patient with chronic Crohn's disease with cicatrization.
In these patients the bowel wall is like a rock and these patients will not respond to steroids or other medication.
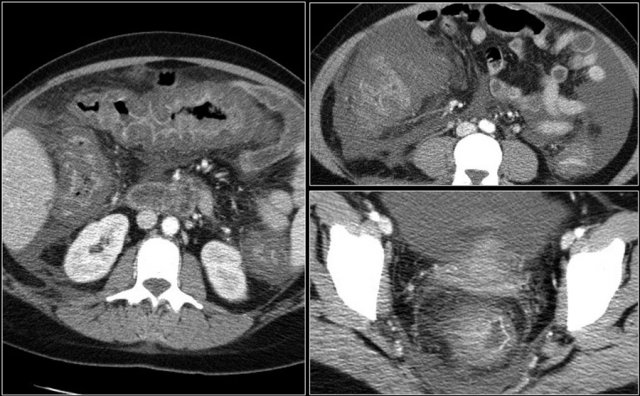
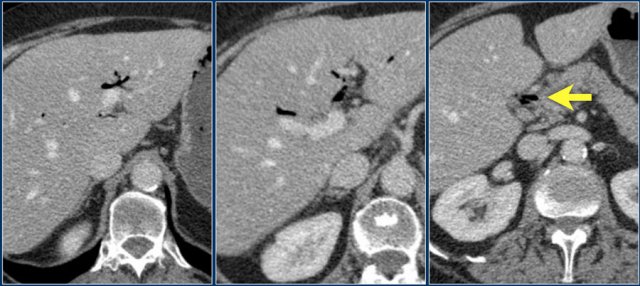
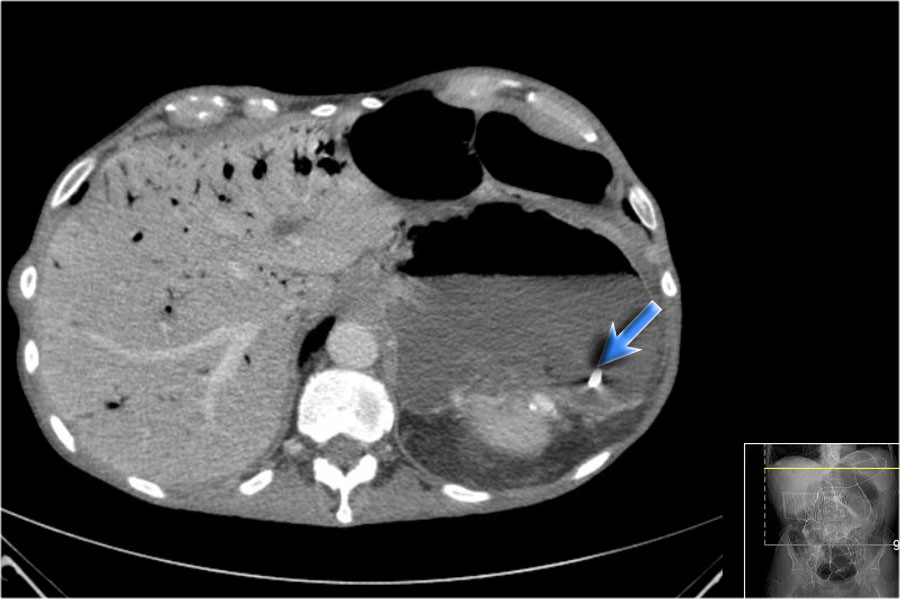
Mesenteric Ischemia
Bowel ischemia frequently affects the colon and is more frequently seen in the splenic flexure, descending colon and sigmoid.
It is mostly due to a low flow state like hypovolemic shock or congestive heart failure.
Especially in elderly with bowel wall thickening you should always put ischemia in your differential diagnostic list.
A special cause of ischemia in the small bowel is a closed loop obstruction, which we will discuss in a moment.
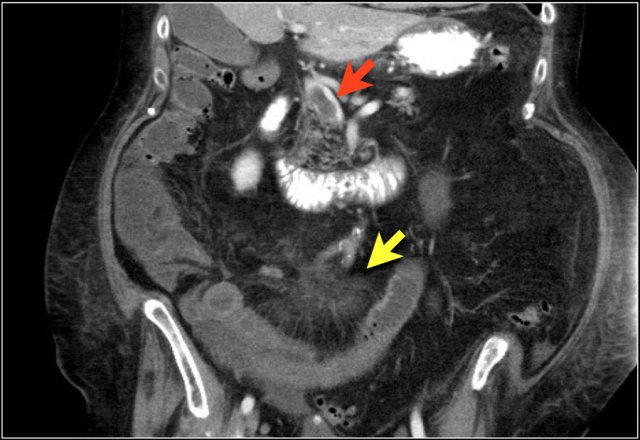
Here a patient with bowel ischemia as a result of thrombosis in the SMV (red arrow).
Notice the venous congestion in the mesentery (yellow arrow).
Here another patient with ischemia of a large segment of the small bowel due to a closed loop obstruction.
An important appearance of a closed loop obstruction is that of a radial array of dilated small bowel loops with the mesenteric vessels converging to a central point.
The findings of ischemia in closed loop obstruction are the same as in patients with other causes of mesenteric ischemia:
- bowel wall thickening
- mesenteric edema
- ascites
- enhancement of the bowel in ischemia can be normal, increased due to reperfusion or there can be lack of enhancement, like in this case.
Click here for more information about closed loop obstruction.
Sometimes it can be helpful to determine the amount of enhancement on thick slab coronal reconstructions.
This is nicely demonstrated in this patient, where there is good enhancement of the jejunum (green area), but lack of enhancement in the ileum (red area) as a result of ischemia.
Here another case of closed loop obstruction.
Notice the difference in enhancement between the normal non-distended loops (green arrow) and the distended strangulated loops (red arrow).
In the center are the twisted mesenteric vessels (yellow arrow).
Tumor
The gray enhancement pattern with loss of identification of the various layers of the bowel wall can be seen in various tumors like adenocarcinoma, metastases and GIST.
Lymphoma and neuroendocrine tumors like carcinoid usually show somewhat more enhancement.
Here a patient with an adenocarcinoma of the sigmoid.
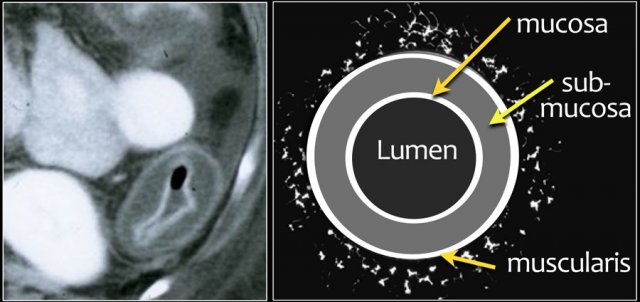
Type 3 - Water target sign
The most common type of enhancement is the target sign with water density.
The target sign is caused by the enhancing mucosa and muscularis propria with the edematous submucosa in between (figure).
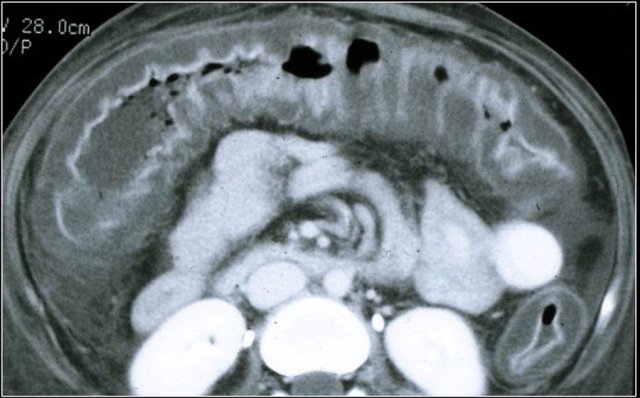
Pseudomembranous Colitis
Pseudomembranous colitis (PMC or sometimes called colitis difficile) is a colitis, that is mostly caused by the bacterium Clostridium difficile due to bacterial overgrowth of the colon in patients who are treated with broad-spectrum antibiotics.
Here a patient with PMC.
There is ascites and hyper enhancement of the bowel wall with submucosal edema and edema in the mesocolon.
The dilated bowel in the right lower abdomen is actually the redundant sigmoid.
The diagnosis is made by testing for the presence of C. difficile toxins in the stool or the presence of C. difficile itself.
The endoscopic detection of pseudomembranes on the mucosa of the colon or rectum used to be diagnostic of PMC before the above tests and CT were available.
Risk factors for developing PMC are:
- broad spectrum antibiotics
- s/p surgery, shock, burns
- cardiac arrest
- proximal to an obstruction in the colon
- HUS, ischemic colitis, uremia
- leukemia, lymphoma, AIDS
Patients present with diarrhea, abdominal pain, and fever caused by the toxins that are produced by the bacteria.
The disease can be complicated by a toxic megacolon.
The CT findings are:
- Circumferential and diffuse mural thickening with submucosal edema.
- Prominent haustrae.
- Eccentric polypoid wall thickening.
- Shaggy luminal contour.
- Oral contrast can be trapped between thick folds simulating sinus tracts.
Portal hypertension
Portal hypertension is another cause of the water target sign.
When a patient has portal hypertension, the increased pressure is transmitted to the right colon.
This leads to the generation of inflammatory mediators and increased production of nitrous oxide, which induces tissue injury.
This produces an isolated right sided colitis.
Study the images and then continue reading.
The findings are:
- Cirrhosis - irregular contour of the liver
- Varices and splenomegaly
- Ascites
- Right-sided colitis
- Aneurysm of the hepatic artery
The differential diagnosis is:
- Portal hypertension
- Infectious colitis
- Ischemic colitis
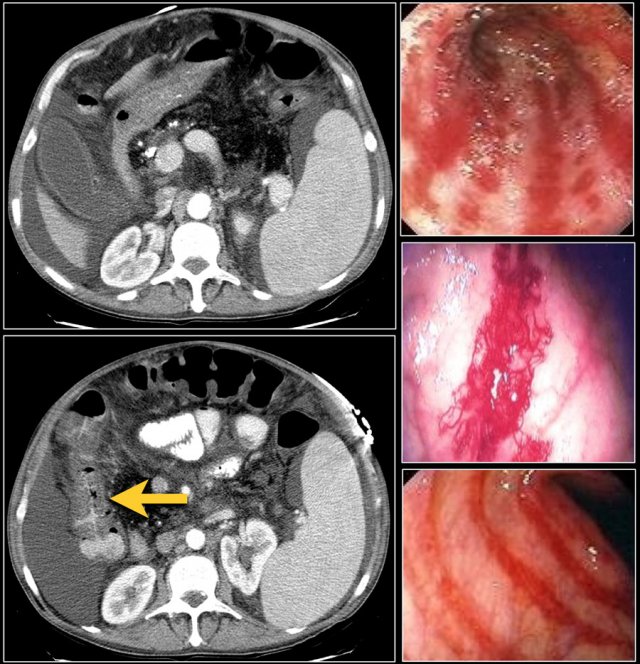 Right -sided colitis in a patient with cirrhosis and portal hypertension. The endoscopic images are of different patient with right-sided colitis.
Right -sided colitis in a patient with cirrhosis and portal hypertension. The endoscopic images are of different patient with right-sided colitis.
Spontaneous bacterial peritonitis
Patients with portal hypertension and right-sided colitis are at risk for developing spontaneous bacterial peritonitis.
In these patients there is vascular ectasia in the right colon.
A diffuse colitis can be seen with granular, erythematous and mucosal friability, which just looks like ulcerating colitis.
The following items make these patients at risk for developing spontaneous bacterial peritonitis:
- Fecal material in the lumen
- High pressure in the portal vein
- Abnormal permeable wall, resulting in bacterial translocation through the colonic wall into the ascites.
Typhlitis
Typhlitis is another disease that presents with the water target sign.
Typhlitis is a necrotizing inflammation of the cecum, which is usually seen in patients with neutropenia due to acute leukemia, AIDS or aplastic anemia.
There is transmural edema and ulceration, which can cause perforation.
The micro-organisms that are involved are: Pseudomonas, Candida, CMV and E. Coli.
These patients are very sick and have fever, watery-bloody diarrhea and neutropenia.
Neutropenia is an abnormally low count of neutrophils, a type of white blood cell that helps fight off infections, particularly those caused by bacteria and fungi.
When the neutropenia is severe - fewer than about 500 cells per microliter of blood - bacteria, that normally present in the mouth and digestive tract can cause infections.
Infectious Colitis
Right colon:
- Salmonella
- Shigella
- Campylobacter
- Yersinia enterocolitica
Diffuse colitis
- E.Coli
- CMV
- Cryptococcus
Left colon and Rectosigmoid:
- Schistosomiasis
Rectosigmoid:
- HSV
- Gonorrhea
Ischemia
In young patients ischemia is usually due to trauma or vasculitis.
Here are images of a young patient with SLE.
There is a gray-pattern of enhancement of the whole left-sided colon.
Type 4 - Fat target sign
Submucosal fat was first reported in patients with chronic ulcerative colitis and Crohn's disease.
Soon it turned out that submucosal fat was frequently seen in obese patients, especially in the transverse and descending colon.
Now the most common cause of the fat target sign is obesity.
Rapid submucosal fat accumulation can be seen in patients that are treated with chemotherapy.
Here a patient with Crohn's disease and a fat-target sign.
17% of patients with Crohn's disease have submucosal fat in the terminal ileum and ascending colon.
It is dependent on the duration of the disease.
Submucosal fat is frequently seen in patients with celiac disease.
Especially if there is isolated fat in the duodenum or in the proximal jejunum, that is very suspicious of celiac disease.
These patients also have more pronounced folds in the ileum compared to the jejunum, which is the opposite of the normal finding (figure).
The faeces in these patients may contain more fat (blue arrow).
How to deal with submucosal fat?
- In a patient without a history of IBD the fat-target sign likely relates to the patient's body habitus.
- In a patient with belly discomfort with duodenal and proximal jejunal fat or fatty feces: suggest celiac disease.
- In patients with acute symptoms suggest acute and chronic IBD
- If there is only involvement terminal ileum query Crohn's disease.
Type 5 - Gas - Pneumatosis
The most concerning pattern is gas within the bowel wall.
Gas within the bowel wall is called pneumatosis intestinalis.
Pneumatosis intestinalis is seen in life-treatening situations in patients with ischemia and impending bowel perforation, who need immediate therapy.
However pneumatosis can also be found as an incidental finding in patients without abdominal complaints.
Finally gas adjacent to the bowel wall can mimick pneumatosis.
This is called pseudopneumatosis.
So the first question is....are we really dealing with pneumatosis intestinalis and what is the clinical setting of the patient.
The clinical course is generally benign when pneumatosis is an incidental finding, such as when it occurs in association with obstructive pulmonary disease.
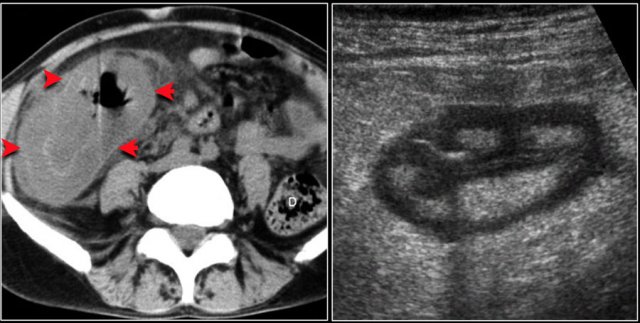
Pseudopneumatosis
Let's first start with pseudopneumatosis, because we don't want to alarm anybody by mistaking normal intraluminal gas for pneumatosis.
Especially in the cecum and ascending colonic gas bubbles can be trapped between fecal debris and the mucosa.
In this case we are quite sure that the gas is intraluminal and not within the wall.
In this case it is more difficult.
The linear arrangement of the gas bubbles makes it suspective of pneumatosis.
However these gas bubbles are trapped between the fecal debris and the bowel wall.
In these cases you have to carefully study all the images and use different window settings.
Give special attention to the non-dependent bowel wall, where there is no feces in contact with the mucosa and gas bubbles will not be seen.
String of pearls sign
This is a patient with a small bowel obstruction (SBO).
Study the images.
Then continue reading.
The CT-images show dilatation of the small bowel.
In these patients the folds of the small bowel or valvulae conniventes will widen and air bubbles will become trapped in a stepladder configuration on the ventral side.
On a horizontal beam radiograph of the abdomen this is known as the string of pearls sign.
Here another case of SBO with a string of pearls sign.
Scroll through the images and then continue reading.
At first glance this really looks like pneumatosis in a patient with a very dilated ascending colon due to an obstructing tumor.
Notice how gas bubbles can be seen in a circular arrangement and are also seen on the non-dependent portion of the bowel wall (blue arrow).
However when we scroll through the images, it becomes clear that these gas bubbles are only seen in between the bowel wall and the bowel content.
When we get to the point, where there is a air-fluid level, there are no air bubbles on the non-dependent portion of the bowel wall.
So this is another case of pseudopneumatosis.
However this still is a very sick bowel and decompression is needed.
Such an accumulation of gas bubbles between the mucosa and the bowel content is only possible in a bowel, that has lost its normal peristaltic movements due to longstanding and severe obstruction.
Portal venous gas
Now let's continue with some patients, who do have pneumatosis.
Here a patient in whom there is no doubt about the diagnosis of pneumatosis intestinalis.
Identifying gas within the mesenteric or portal veins is diagnostic of pneumatosis.
These patients are not only at risk for bowel ischemia and perforation, but also for sepsis.
Portal venous gas is an ominous radiologic sign and is associated with a high mortality rate.
The increased use of CT has resulted in the recognition of an increasing number of non-life threatenig causes of portal venous gas of which diverticulitis is the most common.
Here a patient with extensive pneumatosis and gas within the portal veins.
Bowel ischemia was found at surgery.
Gas in the portal veins has to be differentiated from gas within the bile ducts, which is called pneumobilia.
Sometimes an air-fluid level can be seen in the portal vein.
Portal venous gas is located peripherally in the liver as opposed to pneumobilia which is usually more centrally located.
In this case it is obvious that the air is located within the bile ducts.
There is air centrally in the liver and we also see air in the common bile duct (arrow).
Obstruction is a common cause of pneumatosis.
Here a patient with pneumatosis of the cecum and ascending colon as a result of obstruction due to a sigmoid cancer (arrow).
The gas in the bowel wall indicates an impending perforation.
Here another patient with pneumatosis as result of an obstruction.
Post decompression the wall of the cecum returned to normal.
Pneumatosis due to trauma
Trauma is a well-known cause of pneumatosis.
Laceration of the mucosa due to anastomotic surgery or catheter manupilation may result in entrance of gas into the submucosal layer.
In this patient the insertion of a feeding catheter resulted in pneumatosis of the small bowel.
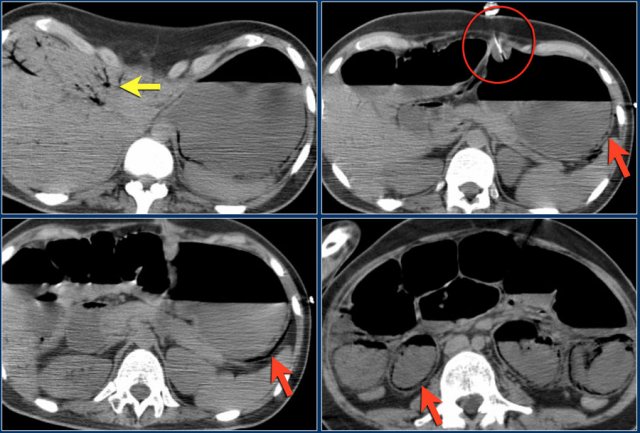
Here a patient with pneumatosis intestinalis after a percutaneous endoscopic gastrostomy (PEG).
This is a procedure in which a PEG tube is passed into the stomach through the abdominal wall to provide a means of feeding when oral intake is not adequate.
Notice the following:
- Portal venous gas (yellow arrow)
- PEG-tube (red circle)
- Pneumatosis in the wall of the stomach and small bowel (red arrows)
Here a very strange case to show how difficult things can be and that findings are not always what they appear to be.
This patient was septic and based on the ultrasound findings the diagnosis of an abscess post-cholecystectomy was made.
A CT was performed to prepare for a CT-guided percutaneous drainage of the abscess (red circle).
Scroll through the images.
Then continue reading.
On the first image there is gas in the portal veins.
There is a feeding catheter which is placed in the duodenum.
There is extensive pneumatosis (red arrows).
The curved arrow indicates the markers that were placed in preparation of the CT-guided drainage.
Based on these findings the patient was transferred for emergency laparotomy, because bowel ischemia was suspected.
At surgery the bowel was distended, but there were no signs of ischemia.
The abscess was drained surgically and the patient did well.
Finally it was concluded that the pneumatosis was probably the result of mucosal damage by the feeding catheter.
This strange case should not mislead you.
These CT-findings will always be suspective of bowel ischemia and necessitate emergency surgery in the proper clinical setting as was in this case.
Incidental pneumatosis
Here images of a patient without any abdominal symptoms.
There is pneumatosis, which was regarded as an incidental finding.
Asymptomatic pneumatosis can be seen in patients with asthma and COPD.
Pneumatosis in mesenteric ischemia
Pneumatosis is sometimes seen in mesenteric ischemia and is a sign of pending perforation and necrosis.
In this patient there is an occlusion of the superior mesenteric artery (red arrow).
This has resulted in ischemia of the right colon with pneumatosis.
Notice the subtle portal venous gas in the left lobe of the liver (yellow arrow).
Degree of mural thickening
The diseases that cause the largest bowel wall thickening are Crohn's disease and Pseudomembranous colitis (PMC).
Mesenteric abnormalities
Patency of the mesenteric vessels
The causes of bowel ischemia are arterial occlusion, venous thrombosis, strangulation and a low flow state.
The image shows a large segment of ileum with poor enhancement.
In the mesentery there is edema and venous engorgement.
These findings indicate ischemia.
Notice the thrombus within the superior mesenteric vein.
Mesenteric changes
In the mesentery we look for:
- enlarged lymphnodes
- edema and engorgement of vessels
- fistula formation
Here we see a fistula between the small bowel and the colon in a patient with Crohn's disease.
Mesenteric edema
Mesenteric edema in association with bowel wall thickening is seen in:
- Ischemia
- Inflammatory bowel disease, especially Crohn's disease
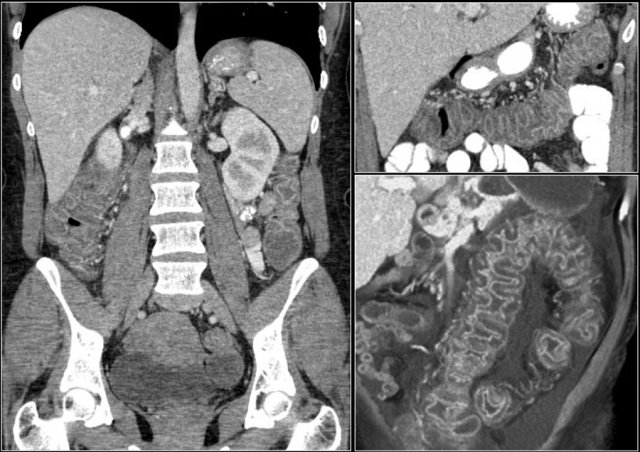
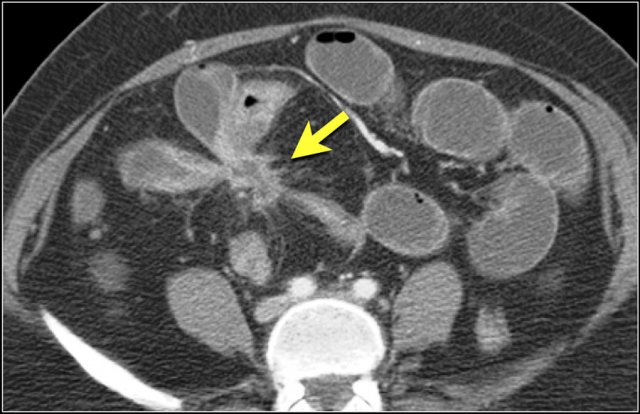
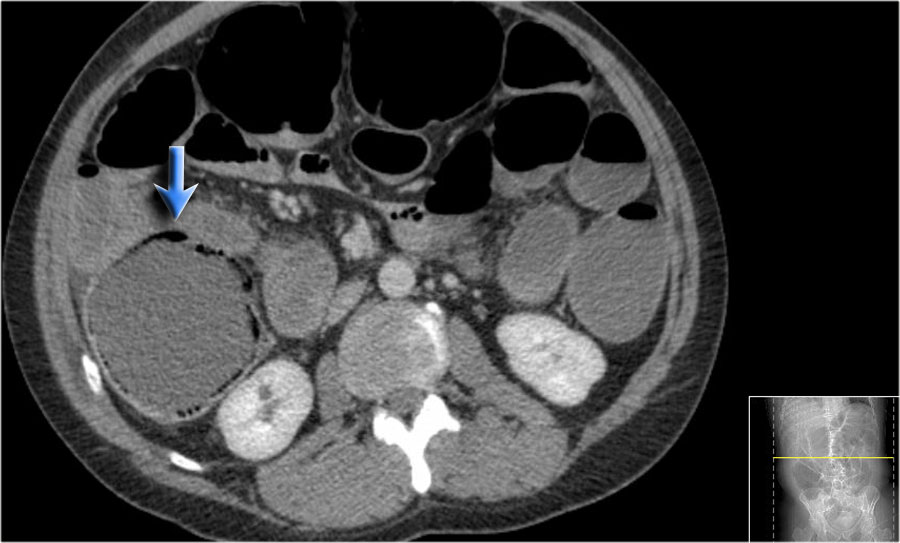
These images are of a patient with a closed loop small bowel obstruction.
Notice the group of small bowel loops with a thickened wall in the right upper abdomen (yellow arrow).
The mesenteric edema (red arrow) indicates increased venous pressure due to strangulation.
Engorgement of vessels
Increased venous pressure in strangulation also leads to engorgement of veins (yellow arrow).
This patient also has a closed loop obstruction with gray enhancement pattern of the strangulated bowel loops (red arrows).
Notice the normal enhancement of small bowel proximal to the obstruction (green arrow).
Another patient with ischemic bowel and extensive mesenteric edema.
At surgery this was all necrotic small bowel.
Lumen contents
Look at the content of the bowel lumen for:
- Fecal material in the small bowel indicating a long standing obstruction
- Blood in the lumen indicating gastrointestinal hemorrhage
- Fat in the colonic lumensometimes seen in celiac disease.
Small bowel feces sign
The yellow arrow indicates a small bowel feces sign in a patient with a small bowel obstruction.
Gastro-intestinal hemorrhage
Here a patient high density bowel content indicating gastro-intestinal hemorrhage.
Fatty bowel content in a patient with celiac disease.