Chest X-Ray - Basic Interpretation
Update 2025
Robin Smithuis and Otto van Delden
Radiology Department of the Alrijne Hospital, Leiderdorp and the Academical Medical Centre, Amsterdam, the Netherlands
Publicationdate
The chest X-ray is the most commonly performed radiological investigation. Every radiologist should be an expert in interpreting chest radiographs. Accurate interpretation necessitates a solid understanding of normal anatomy, anatomical variants, and fundamental radiographic principles.
This article focuses on:
- Normal thoracic anatomy and its variants
- A systematic, inside-out approach to chest film interpretation
- Radiographic features of pathology involving the heart, mediastinum, lungs, pleura, chest wall, and upper abdomen
Normal and Variants
PA view
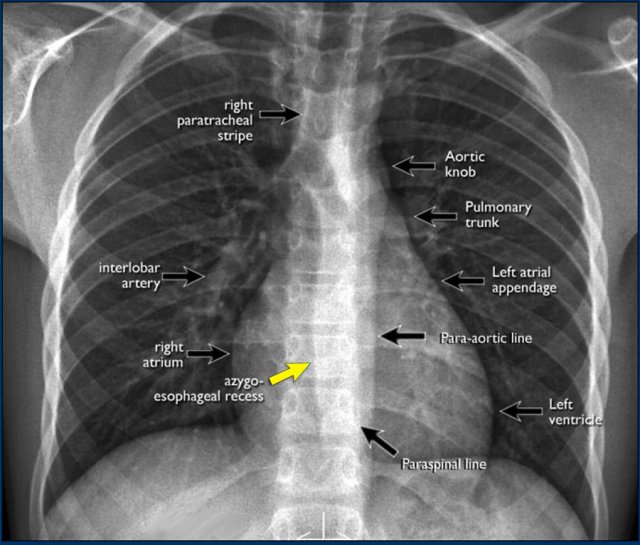
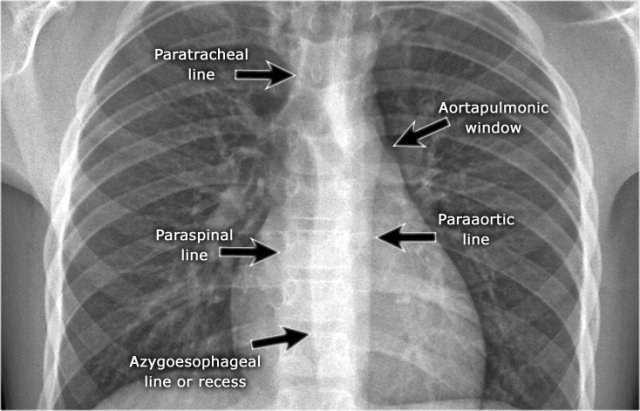
On the PA chest radiograph, careful evaluation of all interfaces between the lungs and adjacent structures—such as the diaphragm, heart, and mediastinum—is essential.
At these interfaces, lung–soft tissue boundaries form visible:
- Lines or stripes (e.g., the right paratracheal stripe)
- Silhouettes (e.g., the aortic knob or left ventricular contour)
These lines and silhouettes serve as anatomical landmarks and help localize pathology. When these contours are displaced or obscured with loss of the normal silhouette, the silhouette sign is present—a key diagnostic feature .
- The paraspinal line may be displaced by a paravertebral abscess, vertebral fracture with hemorrhage, or extravertebral extension of a neoplasm.
- Widening of the right paratracheal stripe (>2–3 mm) may indicate lymphadenopathy, pleural thickening, hemorrhage, fluid overload, or congestive heart failure.
- Displacement of the para-aortic line can be associated with aortic elongation, aneurysm, dissection, or rupture.
The anterior and posterior junction lines, formed where the upper lobes approximate anteriorly and posteriorly, are usually not well visualized and will not be discussed further.
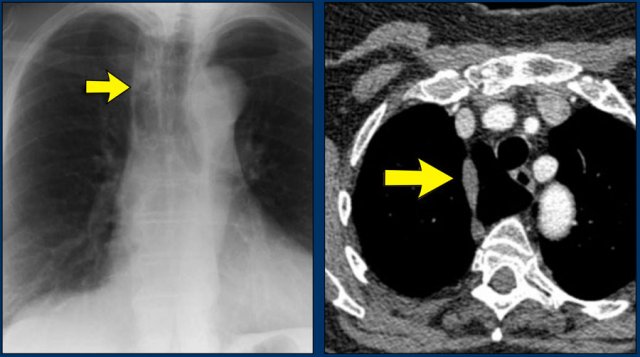
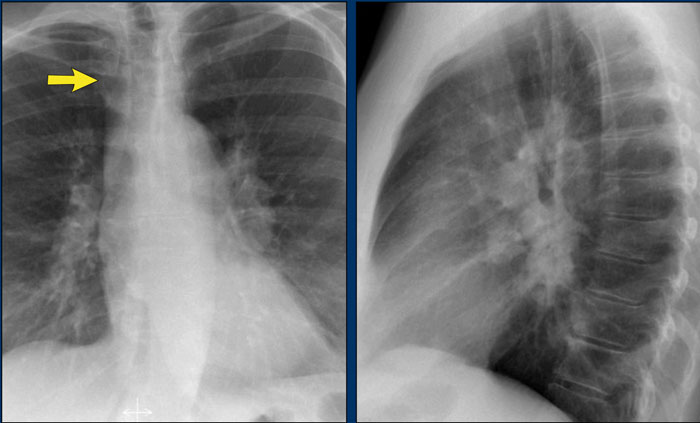
A key mediastinal–pulmonary interface to assess is the azygoesophageal recess (yellow arrow).
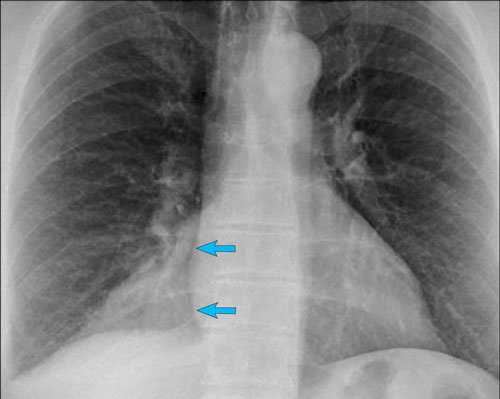
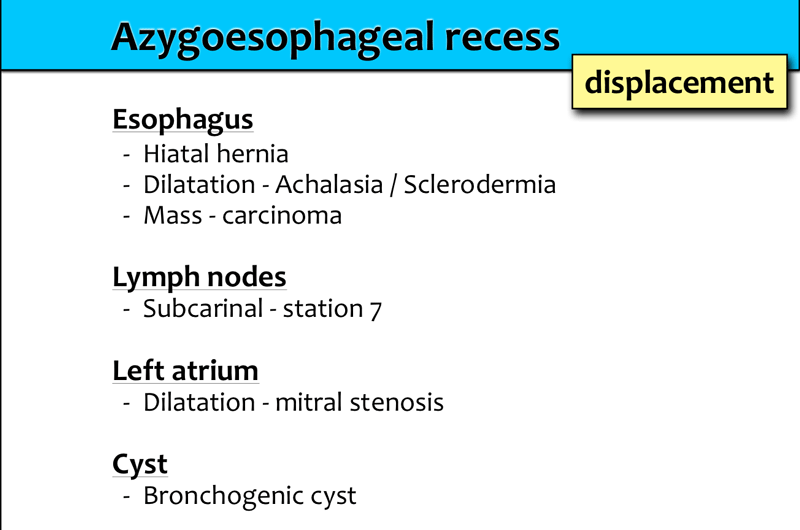
Azygo-esophageal recess
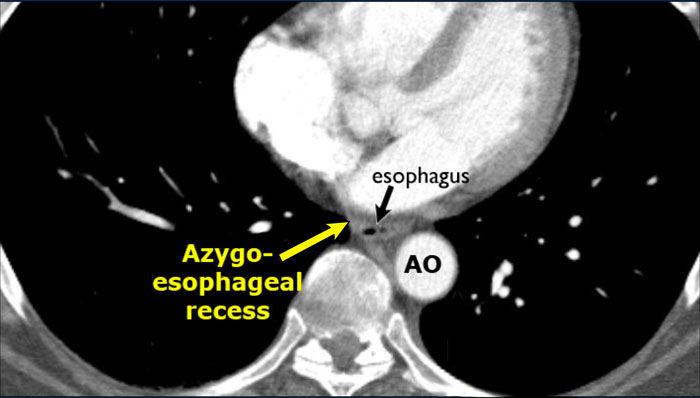
The azygoesophageal recess is located below the level of the azygos vein arch.
In this region, the medial aspect of the right lower lobe abuts the mediastinum between the heart anteriorly and the vertebral column posteriorly.
On its left, it is bordered by the esophagus.
Deviation of the azygoesophageal line may result from:
- Hiatal hernia
- Esophageal pathology
- Left atrial enlargement
- Subcarinal lymphadenopathy
- Bronchogenic cyst
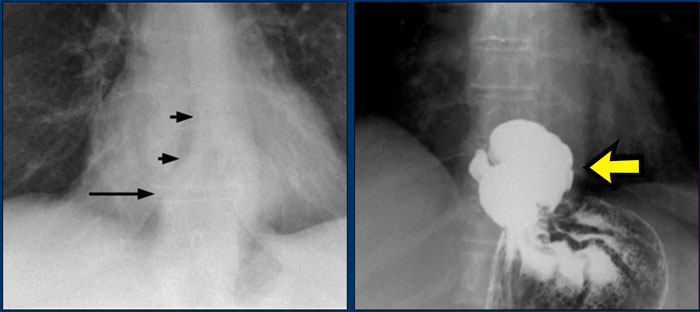
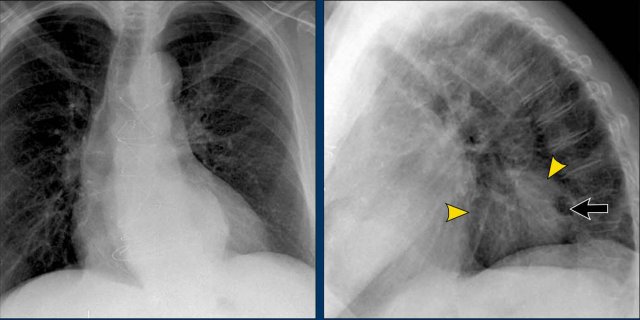
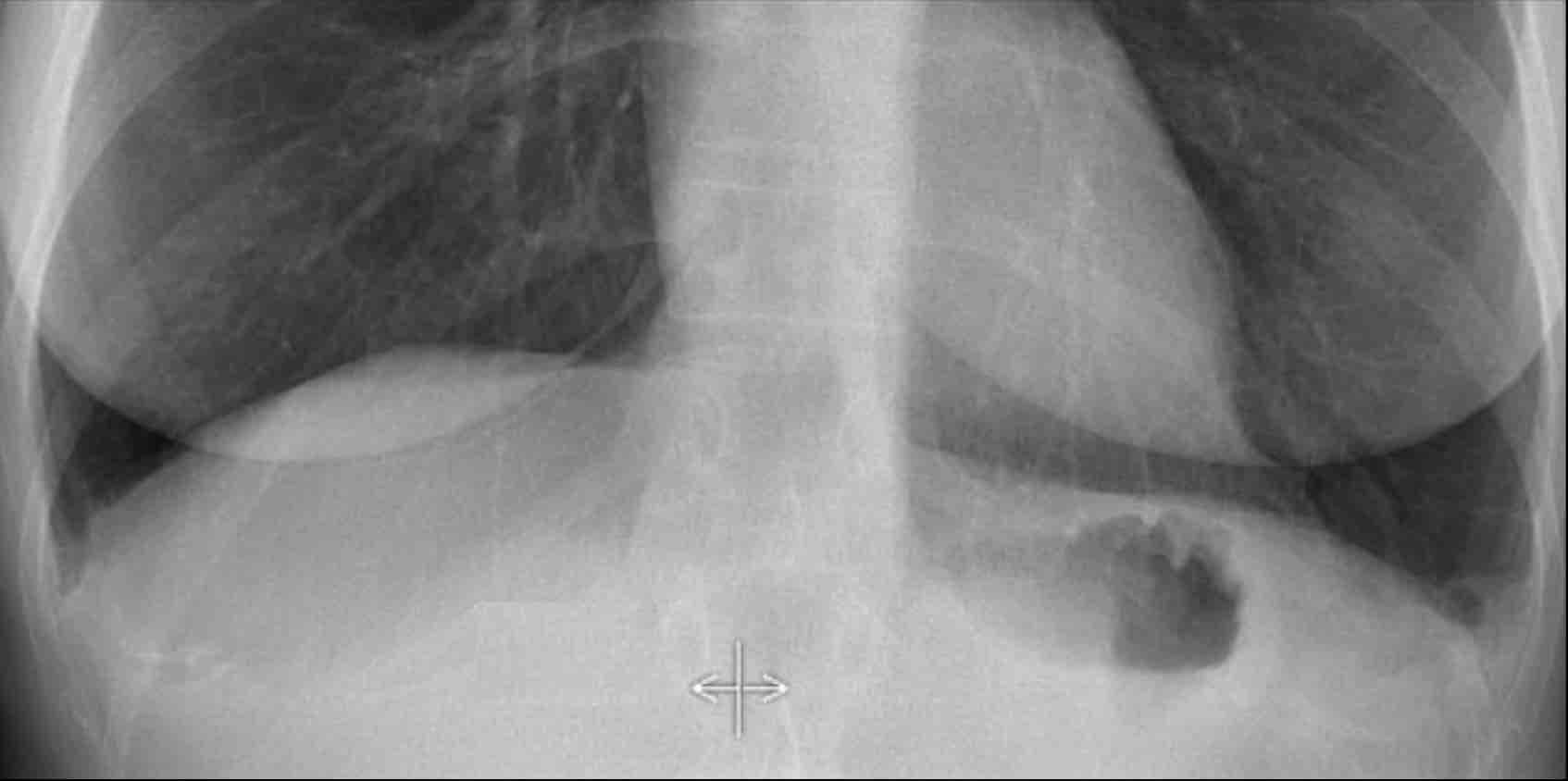
On the PA chest radiograph, a lateral displacement of the azygoesophageal line can be seen.
It is caused by a hiatal hernia.
The arrow points to the barium contrast within the hiatal hernia.
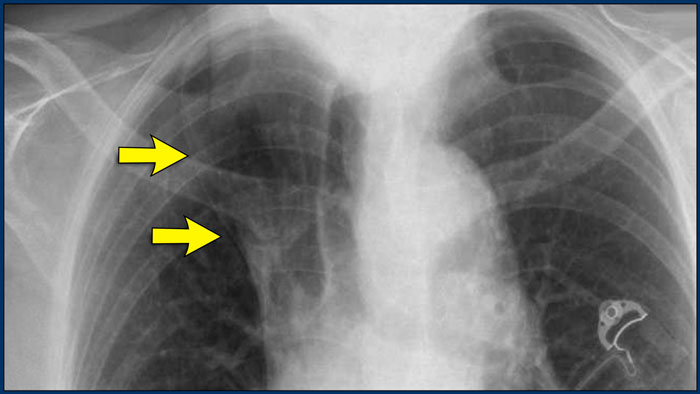
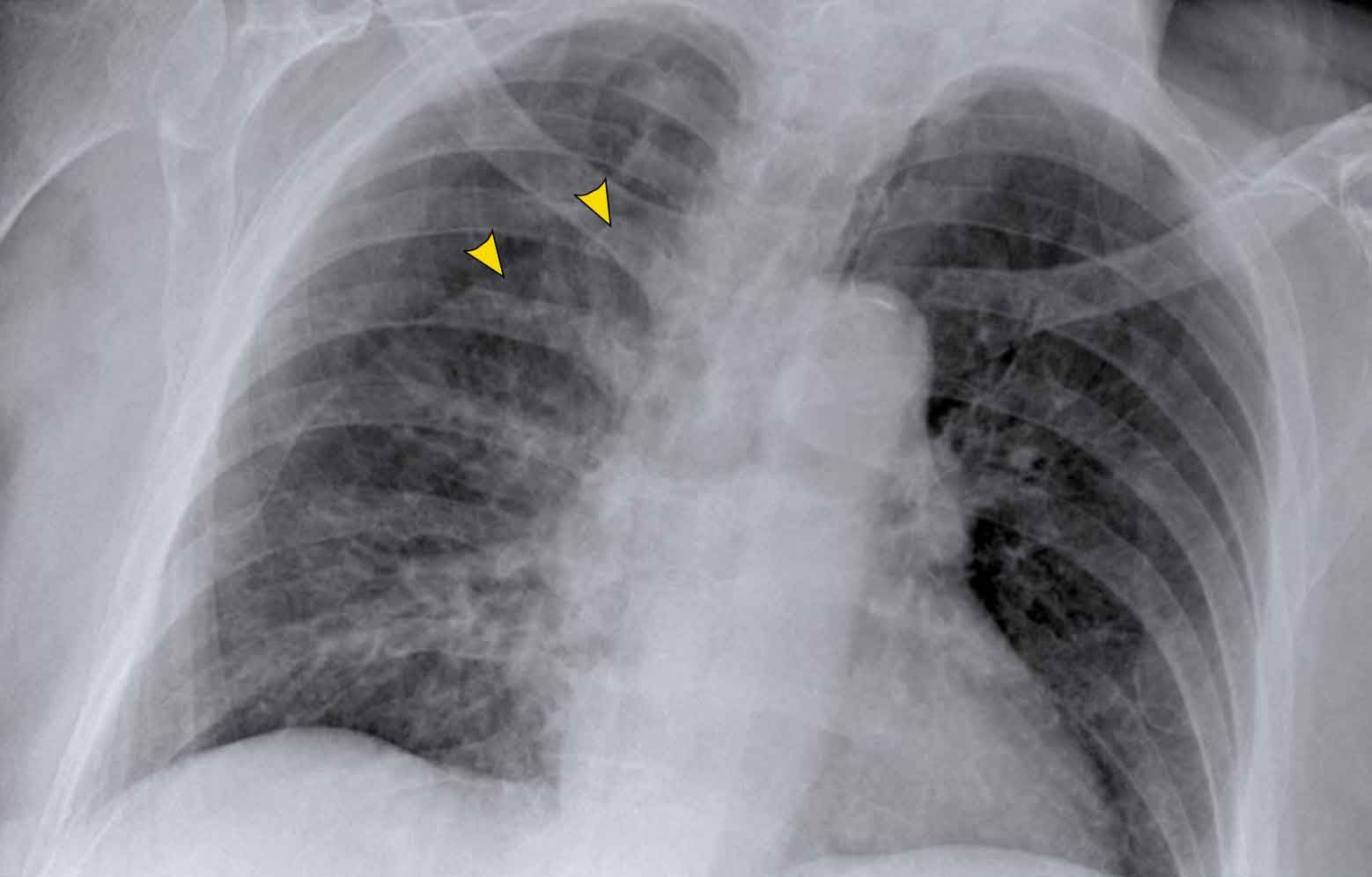
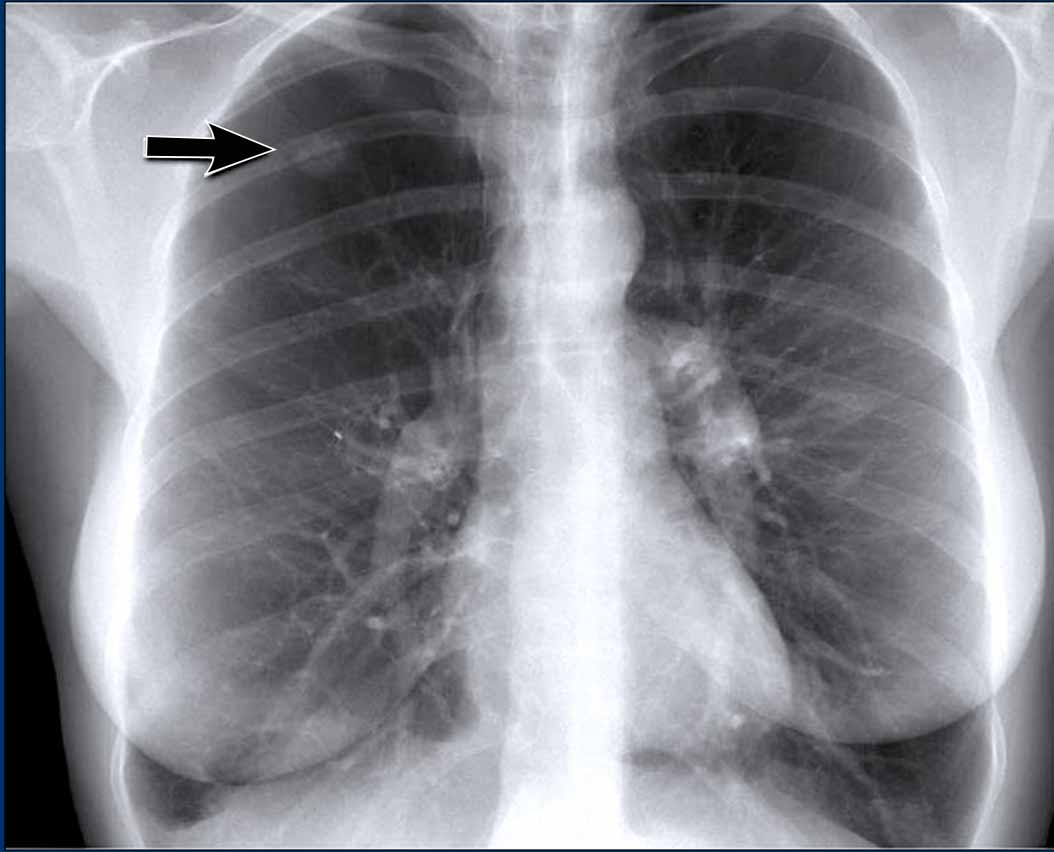
Vena azygos lobe
A common normal variant, the azygos lobe, is formed when the azygos vein takes an anomalous lateral course, creating a deep pleural fissure in the upper lobe of the right lung.
On radiographs, it appears as a thin curvilinear line traversing the right upper lung field, frequently ending in a teardrop-shaped density (the azygos vein) within the azygos fissure.
Here another patient with an azygos lobe.
The azygos vein is seen as a thick structure within the azygos fissure.
Another anatomical variant involves an accessory articulation at the anterior first rib (arrow).
At the junction of the bony and calcified cartilaginous segments, a pseudoarticulation may simulate a pulmonary nodule or mass on frontal imaging.
Pectus excavatum
In patients with pectus excavatum, the right heart border may appear indistinct on frontal chest radiographs.
This appearance can mimic right middle lobe consolidation or atelectasis due to loss of the normal silhouette (silhouette sign).
A lateral chest radiograph is particularly useful in such cases to confirm the diagnosis.
Pectus excavatum is a congenital anterior chest wall deformity characterized by posterior displacement of the sternum and adjacent costal cartilages, resulting in a concave appearance of the anterior thoracic wall.
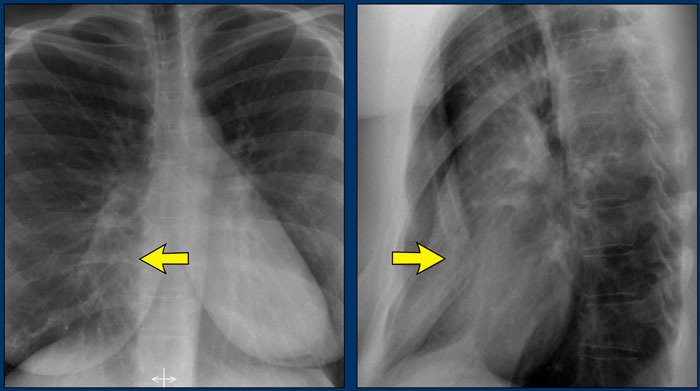
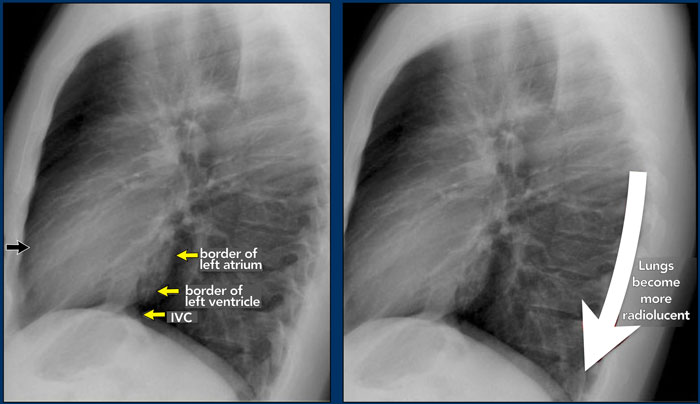
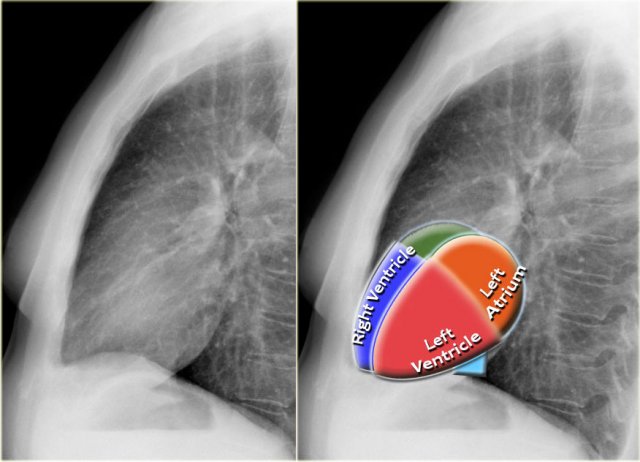
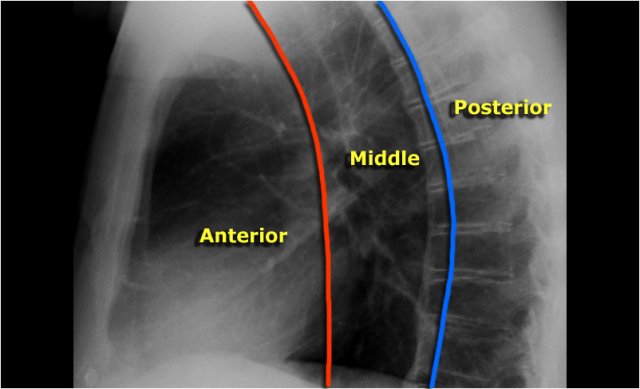
Lateral view
On a lateral chest radiograph, the cardiac borders should be well defined, and the inferior vena cava (IVC) can typically be seen entering the right atrium.
Retrosternal Clear Space
The retrosternal space normally contains aerated lung and should therefore appear radiolucent (dark on the radiograph), extending inferiorly to the level where the right ventricle contacts the sternum (small black arrow).
Any radiopacity within the upper retrosternal space is suspicious for a lesion in the anterior mediastinum or a mass arising from the upper lobes of the lungs.
Spine Sign
When evaluating the vertebral bodies on the lateral view, they should appear progressively more radiolucent (darker) from top to bottom due to the increasing amount of aerated lung overlying them (white arrow).
If the lower thoracic vertebrae appear abnormally dense, it may indicate pathology in the lower lobes, such as consolidation or mass lesions — this is known as the spine sign.
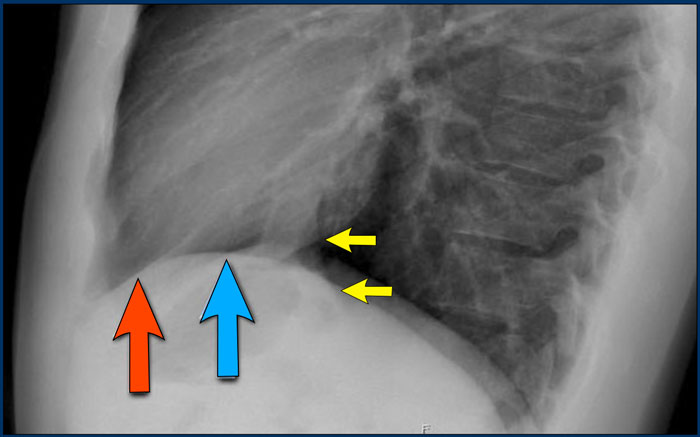
Diaphragm Evaluation
- The right hemidiaphragm should be clearly visible anteriorly up to the chest wall (red arrow), representing the interface between aerated lung and abdominal soft tissues.
- The left hemidiaphragm is usually visible only up to the point where it is adjacent to the cardiac silhouette (blue arrow), beyond which the interface is lost due to the similar radiodensity of the heart and upper abdominal contents.
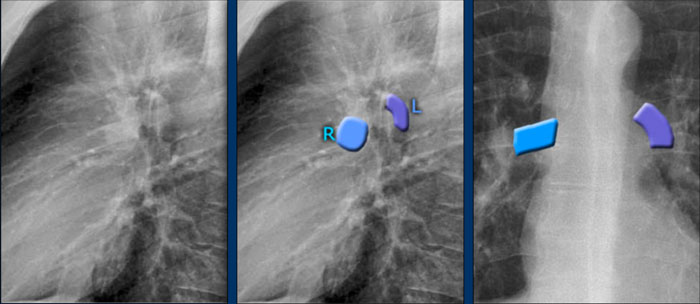
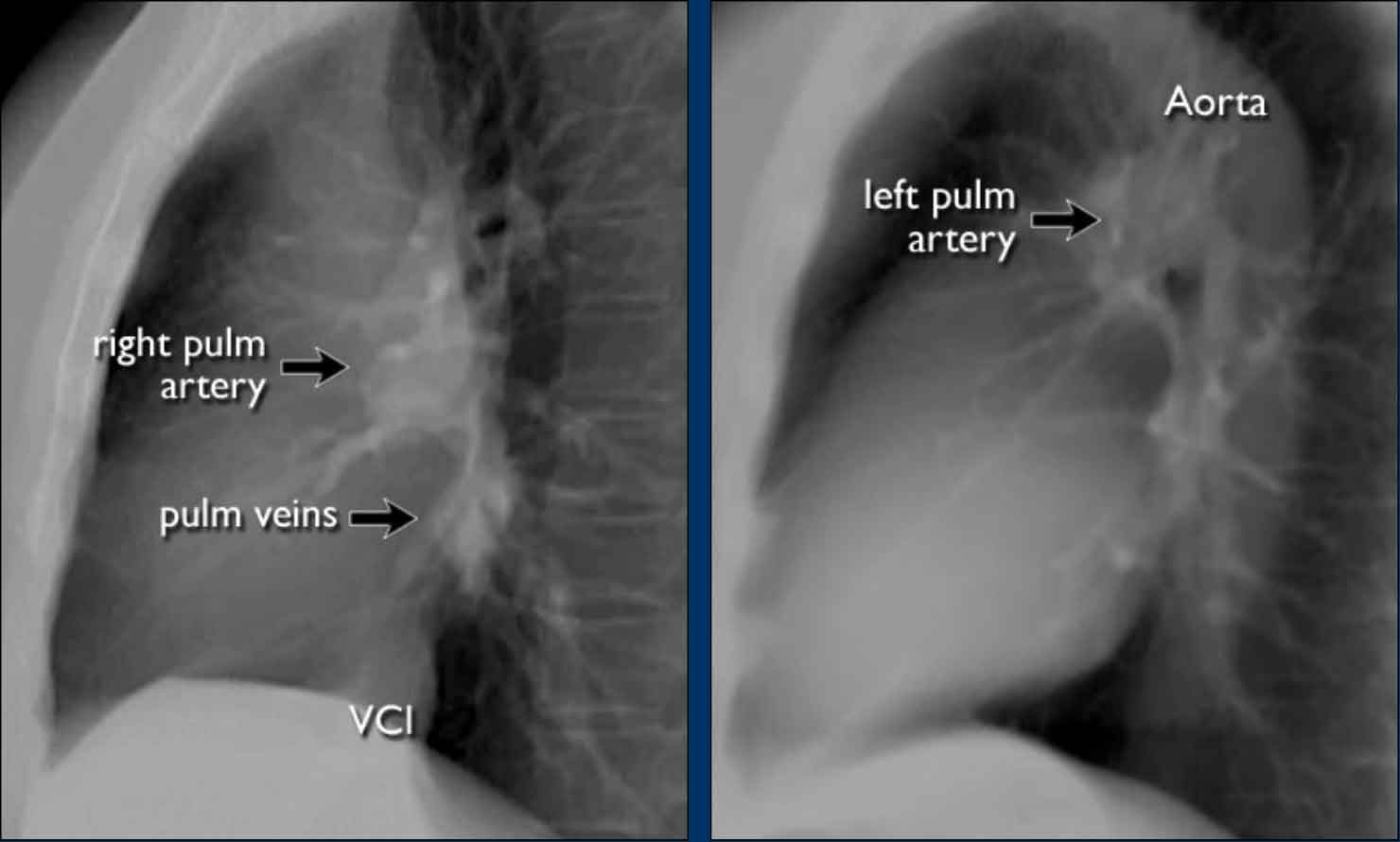
Pulmonary Vasculature and Hilar Structures
The left pulmonary artery (shown in purple) arches above the left main bronchus and is situated higher than the right pulmonary artery (in blue), which courses anterior to the right main bronchus.
Understanding normal hilar anatomy on the lateral view facilitates detection of abnormalities.
For example:
- On the PA view, hilar enlargement may be noted, but it can be difficult to differentiate between vascular dilatation and lymphadenopathy.
- On the lateral view, the presence of rounded opacities in regions where pulmonary vessels are not normally seen strongly suggests enlarged lymph nodes.
In this case, the patient was diagnosed with sarcoidosis.
Additionally, note the widened paratracheal stripe, another indicator of mediastinal lymphadenopathy.
Spondylosis Mimicking Lung Lesions
Degenerative changes of the spine (spondylosis) can occasionally simulate a pulmonary mass on the lateral view.
- Any opacity in the region of the vertebral bodies should prompt correlation with the PA view to assess for spondylotic osteophytes, which are typically located on the right side.
- On the left, osteophyte formation is less pronounced due to aortic pulsations that inhibit calcification.
Mediastinal Masses on Lateral View
When the superior mediastinum appears widened on the PA view, the lateral view is useful to localize the abnormality.
- A soft tissue density in the retrosternal space narrows the differential diagnosis to anterior mediastinal masses, commonly remembered as the "4 Ts":
- Thymoma
- Teratoma (germ cell tumors)
- Thyroid mass
- Terrible lymphoma
In this case, the patient was diagnosed with Hodgkin lymphoma.
Congenital Diaphragmatic Hernias
Bochdalek Hernia
- A Bochdalek hernia is a common incidental finding in adults and results from a posterior diaphragmatic defect(arrows).
- It typically contains retroperitoneal fat, is asymptomatic, and discovered incidentally.
- In rare cases, abdominal organs may herniate into the thorax.
- In neonates, large Bochdalek hernias may lead to pulmonary hypoplasia, which can be life-threatening.
Morgagni Hernia
- A Morgagni hernia is a less common congenital diaphragmatic hernia.
- It is located anteriorly, often presenting as a right-sided retrosternal mass.
- Like Bochdalek hernias, it may be asymptomatic or contain herniated abdominal contents.
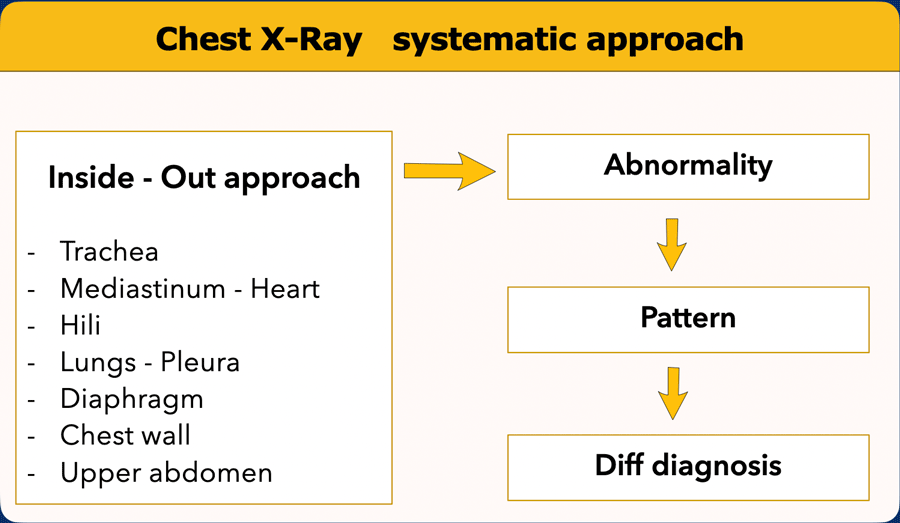
Systematic Approach
A structured, methodical approach is essential for accurate and reproducible interpretation of chest radiographs.
One commonly used technique is the inside-out approach, which begins with central structures and progresses outward.
Inside-Out Approach: Step-by-Step
- Trachea and Central Airways
- Assess the position and caliber of the trachea.
- Deviation may suggest mass effect, volume loss, or mediastinal shift.
- Evaluate the main bronchi for narrowing, displacement, or obstruction.
- Mediastinum and Heart
- Inspect the mediastinal contours for widening, masses, or abnormal silhouettes.
- Evaluate the heart size and borders. A cardiothoracic ratio >0.5 on a PA film may indicate cardiomegaly.
- Observe the aortic arch and descending thoracic aorta for signs of dilation or dissection.
- Hila
- Check the size, position, and density of the hila.
- Asymmetry may indicate lymphadenopathy, vascular enlargement, or mass lesions.
- Lungs and Pleura
- Examine each lung field for opacities, lucencies, consolidation, nodules, or interstitial patterns.
- Look for pleural effusions, pneumothorax, or pleural thickening.
- Pay close attention to lung zones and the fissures (if visible).
- Diaphragm and Subdiaphragmatic Regions
- Compare the hemidiaphragms for height and contour.
- Free subdiaphragmatic air may indicate perforated viscus.
- Evaluate the costophrenic angles for blunting due to effusion or fibrosis.
- Chest Wall and Soft Tissues
- Inspect the bony thorax for fractures, lytic or sclerotic lesions, and alignment.
- Check for soft tissue abnormalities, subcutaneous emphysema, or masses.
- Upper Abdomen
- Evaluate visible upper abdominal structures, including gas patterns, organomegaly, and calcifications.
Importance of Prior Imaging
Always compare current chest radiographs with prior studies—this is a fundamental principle in radiologic interpretation.
In fact, it has often been said that “the most important radiograph is the old film”, as it provides essential context for evaluating stability or progression of findings.
For example, a lung mass that has remained unchanged over many years is unlikely to represent a primary lung cancer.
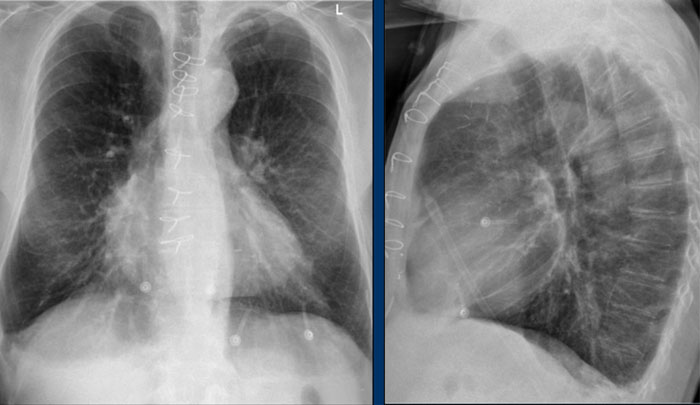
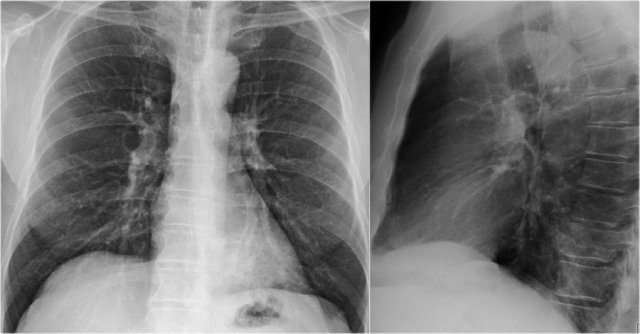
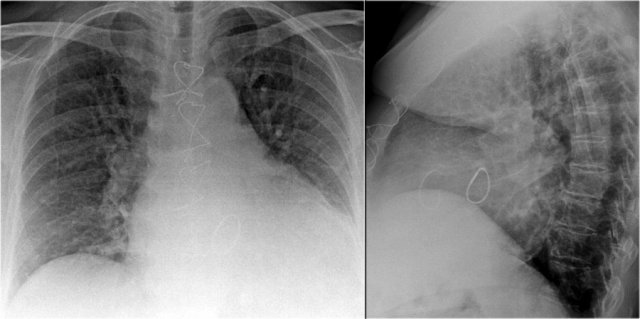
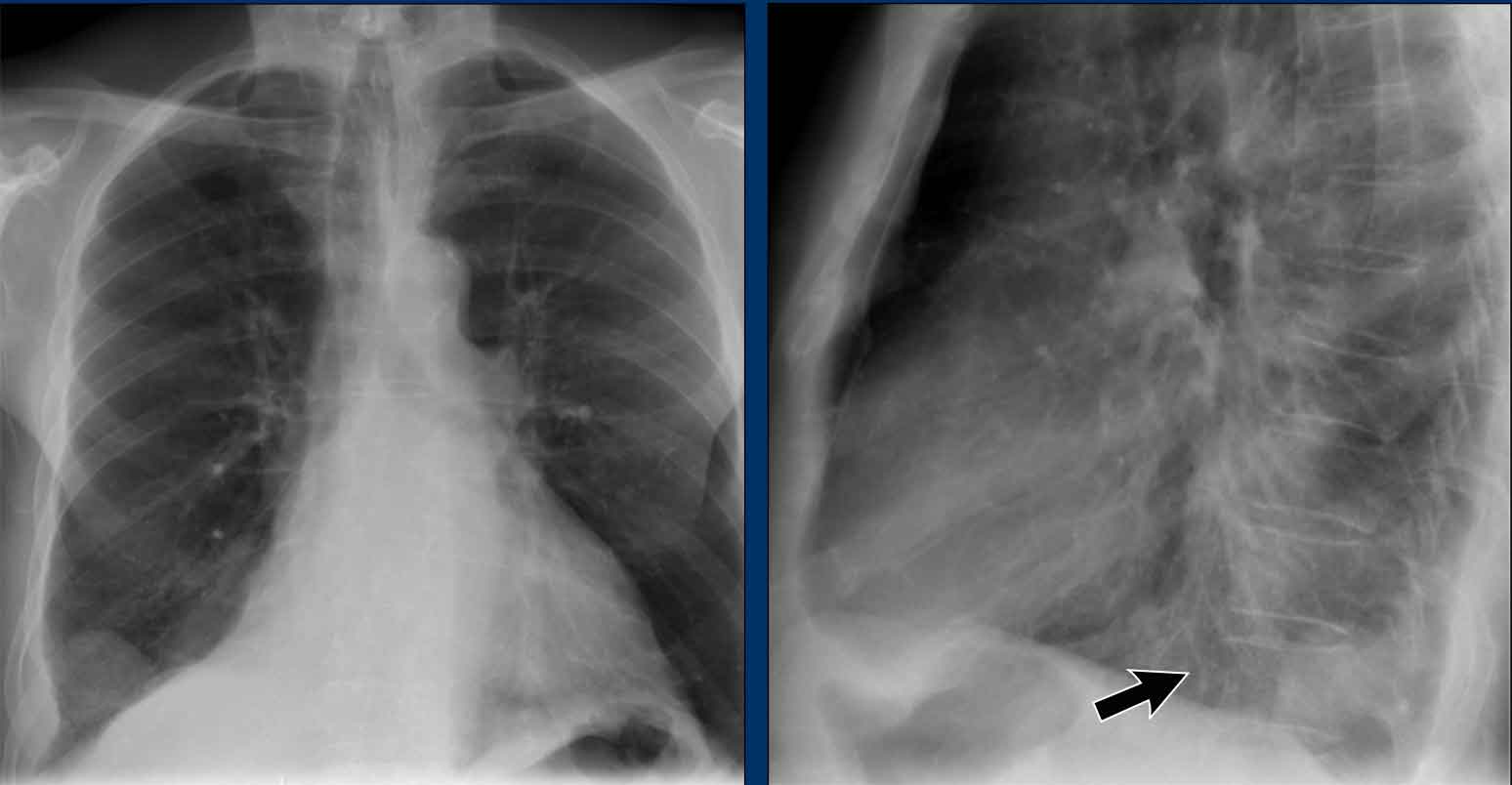
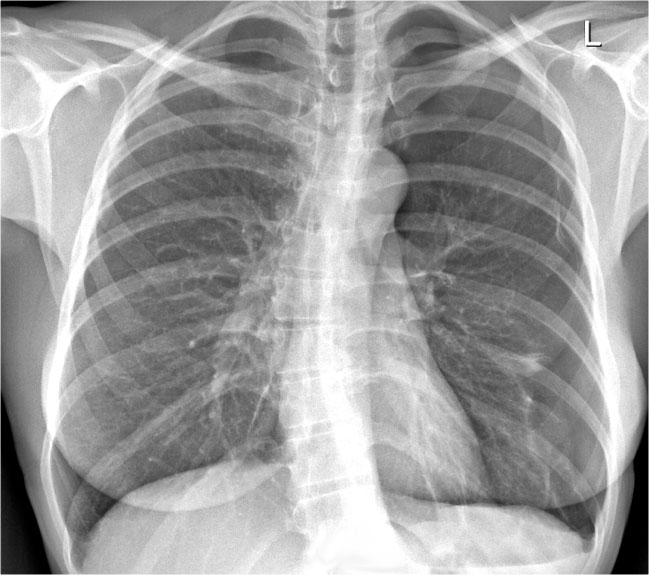
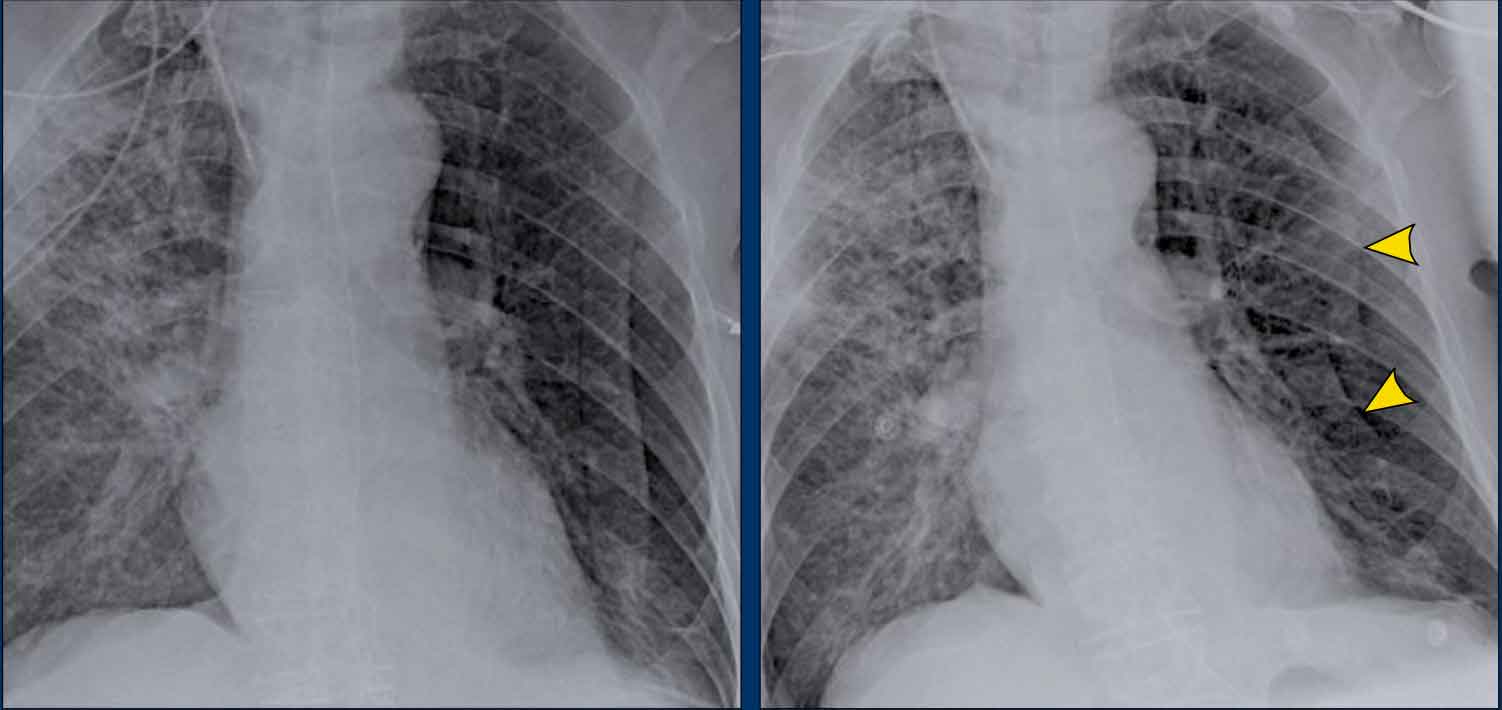
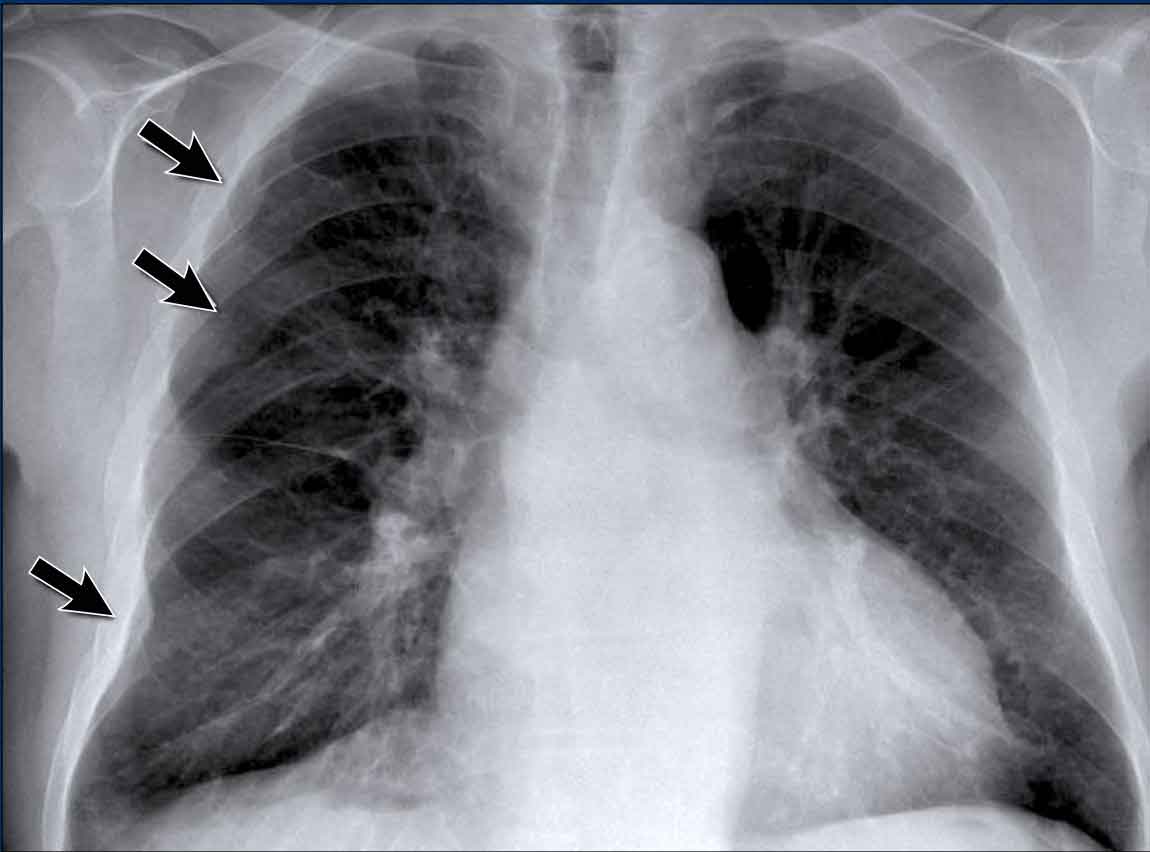
Case Example: Subtle Signs of Congestive Heart Failure
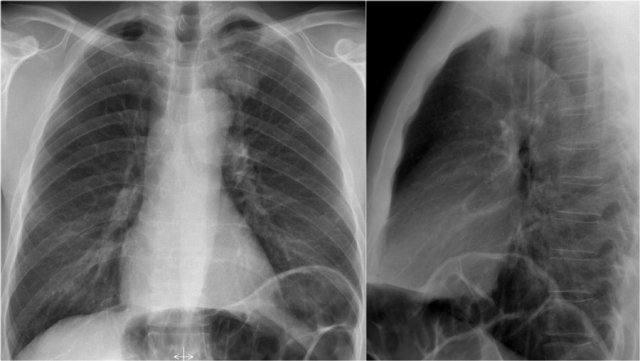
Begin by reviewing these current chest radiographs.
Based solely on these images, one might suspect congestive heart failure (CHF), though the findings are subtle.
Now review the previous study…

Scrolling between the current and prior films significantly increases diagnostic confidence in your diagnosis of congestive heart failure.
Key comparative findings include:
- Cardiac size: Slightly increased compared to the previous study; however, cardiomegaly was already present.
- Pulmonary vasculature: Mild vascular engorgement suggesting elevated pulmonary venous pressure.
- Interstitial markings: Subtle signs of interstitial edema .
- Pleural effusions: Bilateral small effusions, with subtle changes in the inferoposterior borders of the lower lobes, suggesting fluid accumulation.
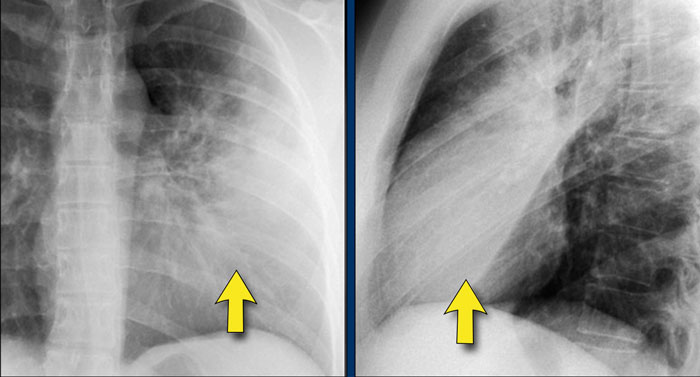
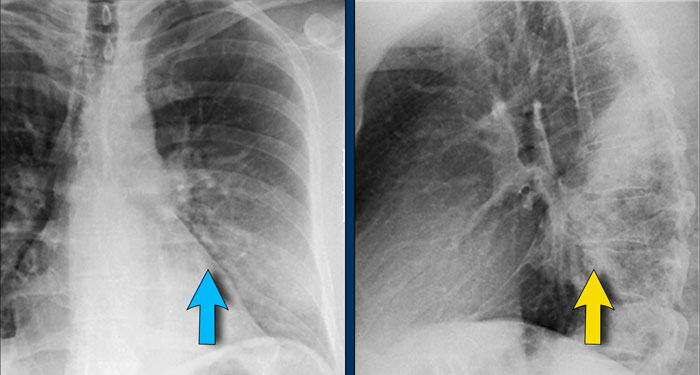
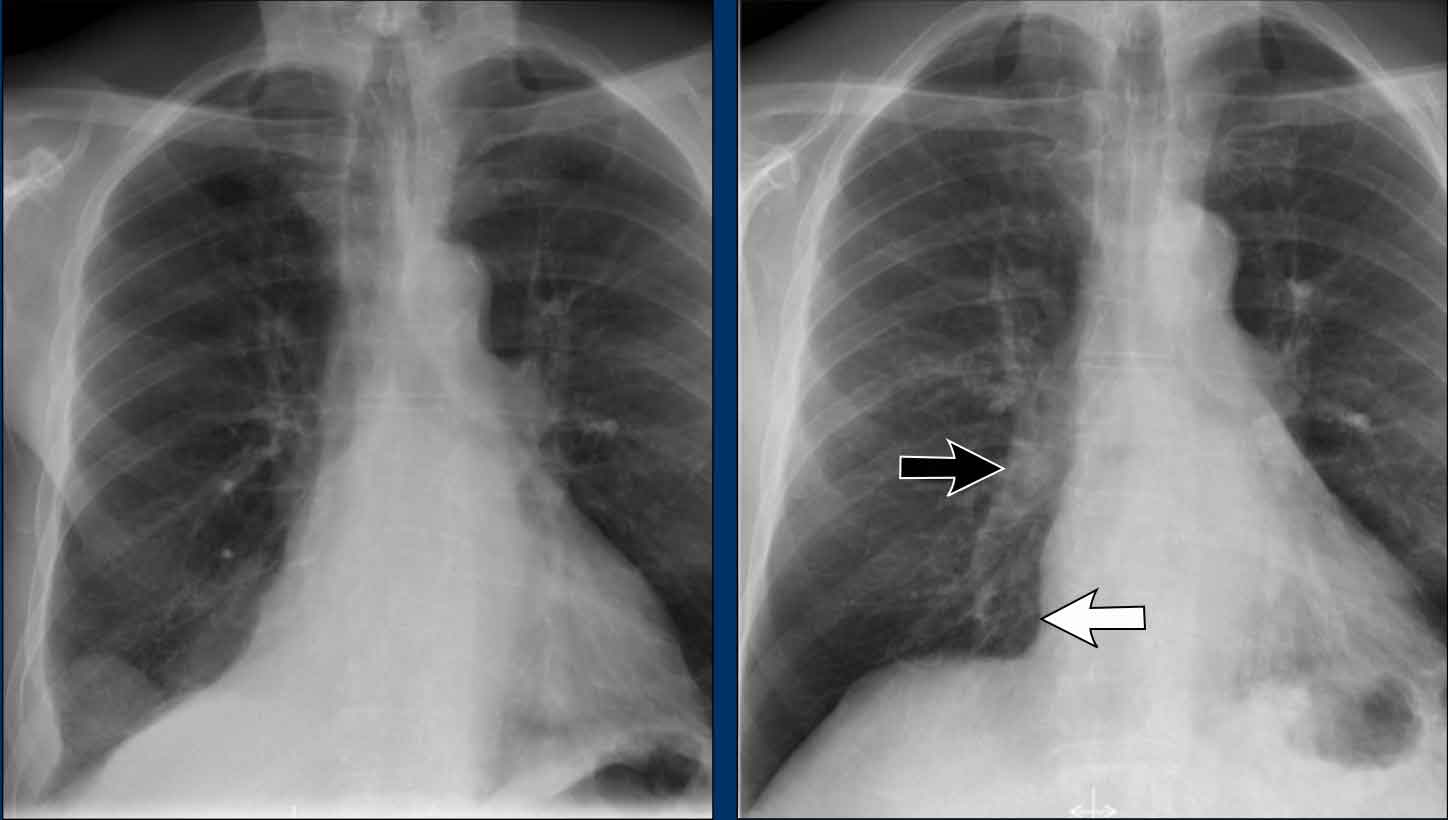
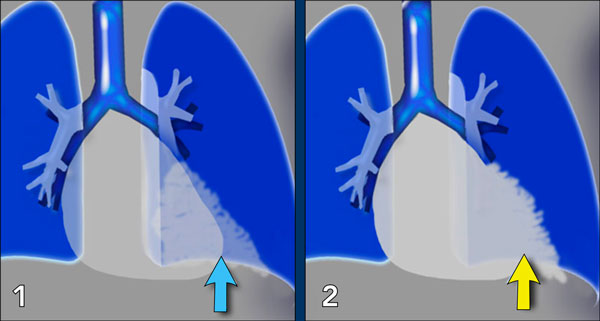 1. No silhouette sign in a consolidation located in the left lower lobe (blue arrow). 2. Silhouette sign in a consolidation in the lingula lobe (yellow arrow).
1. No silhouette sign in a consolidation located in the left lower lobe (blue arrow). 2. Silhouette sign in a consolidation in the lingula lobe (yellow arrow).
Silhouette sign
The silhouette sign refers to the loss of the normal border between structures of different radiographic densities, most commonly air-filled lung adjacent to soft tissue structures like the heart or diaphragm.
This sign is crucial for detecting subtle pathology and localizing lesions within the thorax.
Illustration of the Silhouette Sign
- No Silhouette Sign (Blue Arrow)
- The left ventricle, located anteriorly, is normally bordered by air-filled lingula of the left upper lobe.
- If a consolidation occurs in the left lower lobe (posterior), the interface between the lingula and the heart remains intact, and the left heart border is preserved.
- Positive Silhouette Sign (Yellow Arrow)
- When consolidation is present in the lingula, which directly abuts the left heart border, the silhouette of the left ventricle becomes obscured.
- This indicates the pathology is located anteriorly in the chest.
Silhouette Sign – Examples
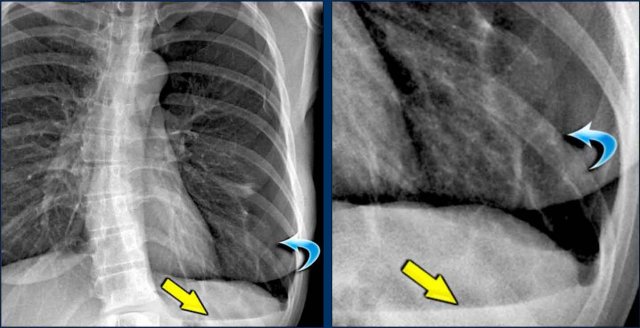
Case 1: PA View
- The left heart border is obscured on the PA radiograph.
- Without even reviewing the lateral view, this finding localizes the pathology to the anterior segment of the left lung, likely the lingula.
- Diagnosis: Lobar pneumonia due to Streptococcus pneumoniae.
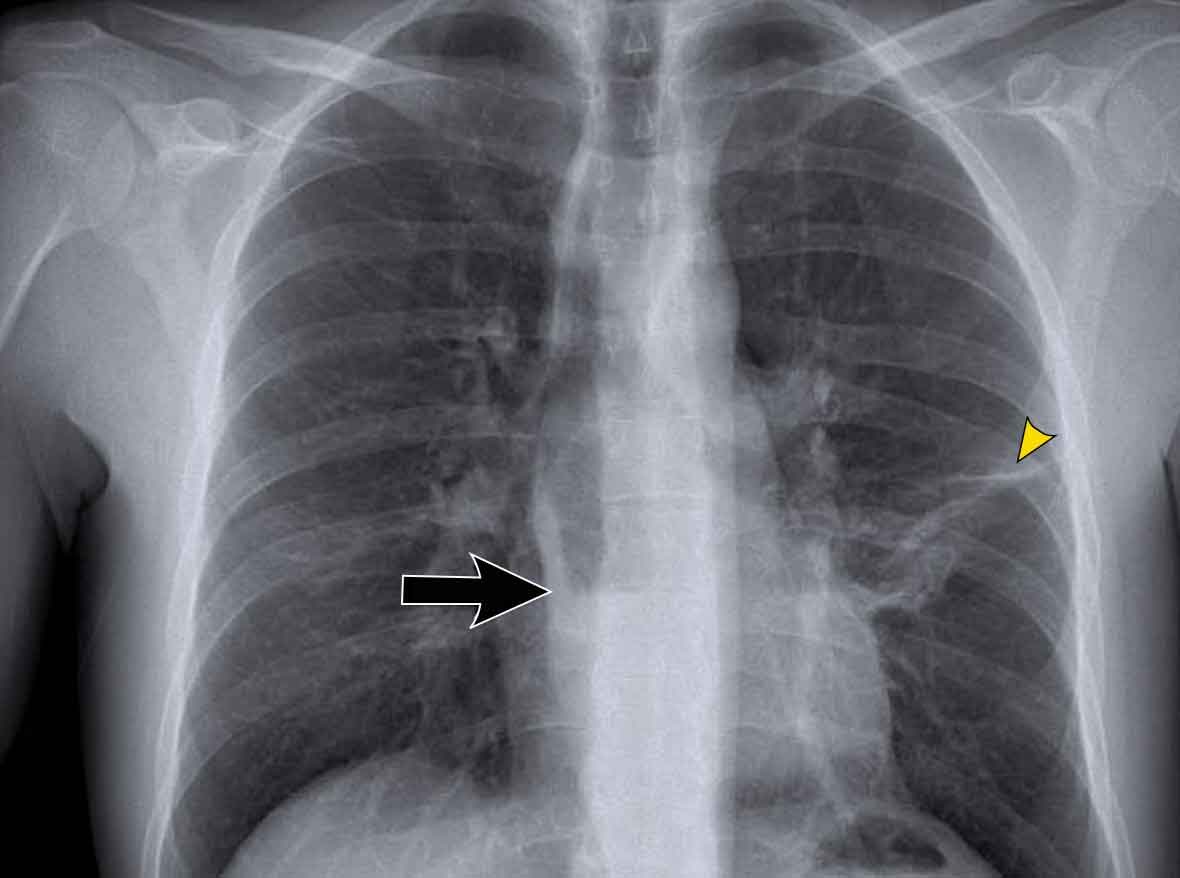
Case 2: PA View
- A consolidation is visible in the left lower lobe (yellow arrow).
- The left heart border remains well-defined with a normal silhouette (blue arrow), indicating the lesion is posterior, not involving the lingula.

Silhouette Sign – Lateral View Analysis
Case 3: Lateral View
- There is increased opacity over the lower thoracic spine.
- Careful analysis of the diaphragmatic contours on the lateral view helps localize the lesion:
- The right hemidiaphragm contour is not visible posteriorly, suggesting the presence of a water-density lesion in the right lower lobe.
- Proceed to the PA view…
PA View of the Same Patient
- The right heart border is intact, confirming the lesion is not anterior—in agreement with the lateral film.
- Question: Why is the silhouette of the right diaphragm still visible on the PA-view?
- Answer: The visible portion of the diaphragm on the PA view represents the highest anterior point, which is not in contact with the posterior pneumonia in the right lower lobe. Therefore, there is a normal silhouette and the silhouette sign is absent.
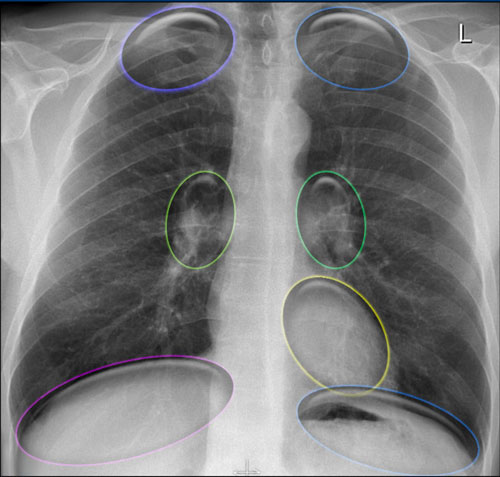
Hidden Areas on Chest Radiography
Certain regions of the chest are prone to being overlooked on standard chest radiographs due to overlapping anatomical structures. These are referred to as the "hidden areas", and they warrant particular attention during image interpretation to avoid missing subtle or significant pathology.
Key Hidden Areas:
- Apical zones
- Hilar regions
- Retrocardiac region
- Subdiaphragmatic zone (below the diaphragmatic domes)
Hidden Areas (1)
It’s important to recognize that a substantial volume of lung parenchyma extends below the dome of the diaphragm, particularly in the posterior lower lobes.
This area (illustrated in blue) must be carefully evaluated.
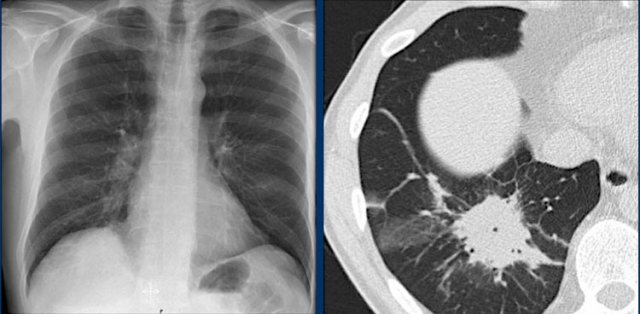
Hidden Areas (2): Right Lower Lobe Lesion
This example demonstrates a large mass in the right lower lobe that is challenging to identify on the PA view unless close attention is paid to the hidden areas.
- On initial inspection, the lesion is inconspicuous.
- However, with focused review of the subdiaphragmatic and retrocardiac regions, the abnormality becomes evident.
- Enlarge the image for better visualization.
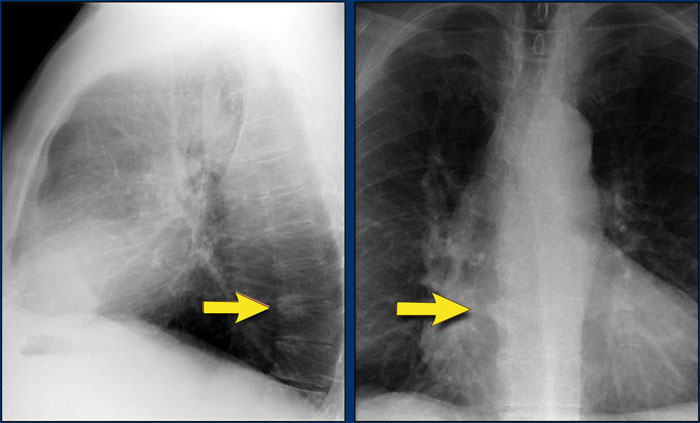
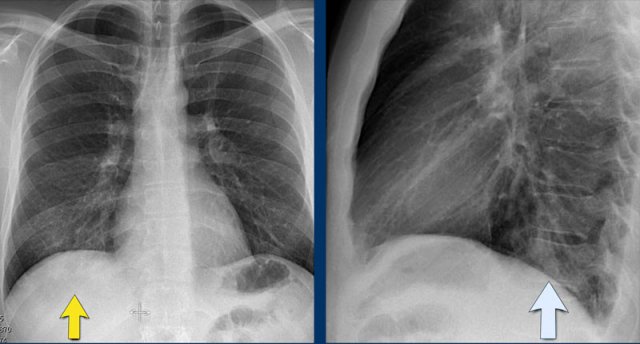
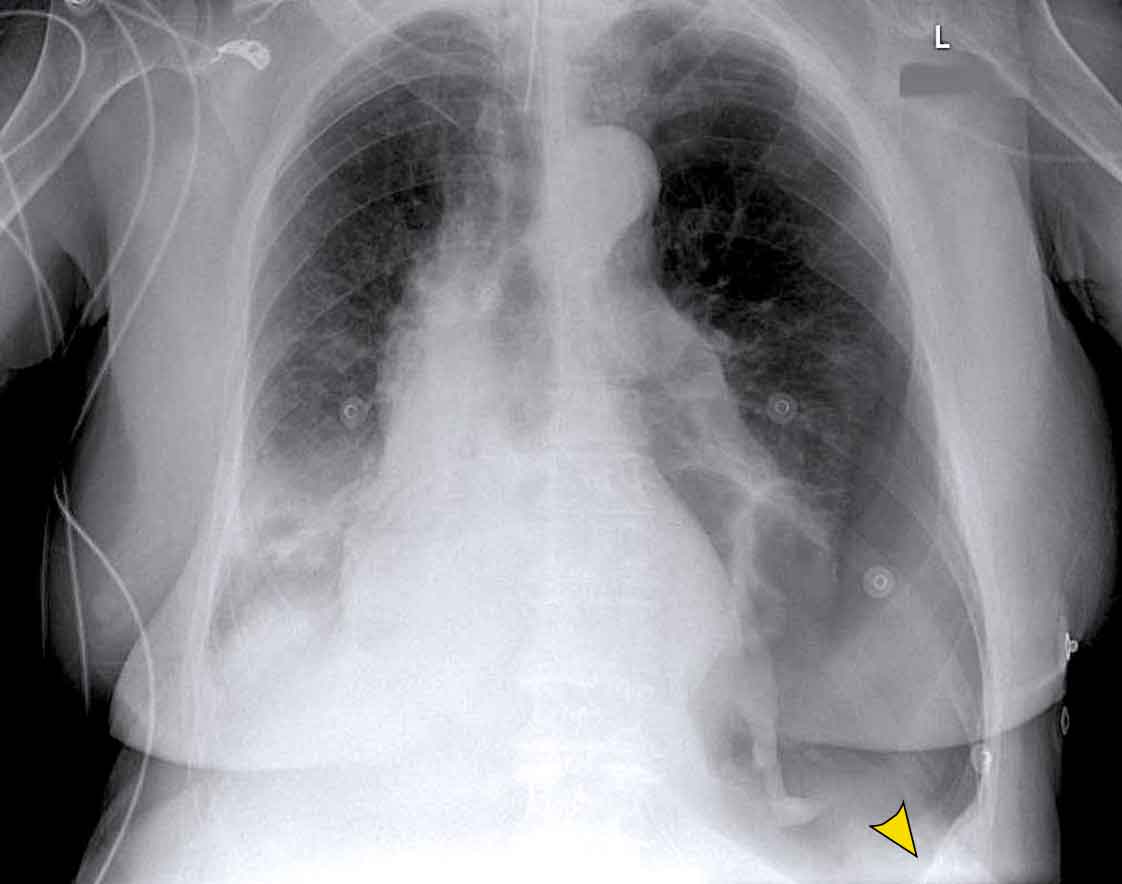
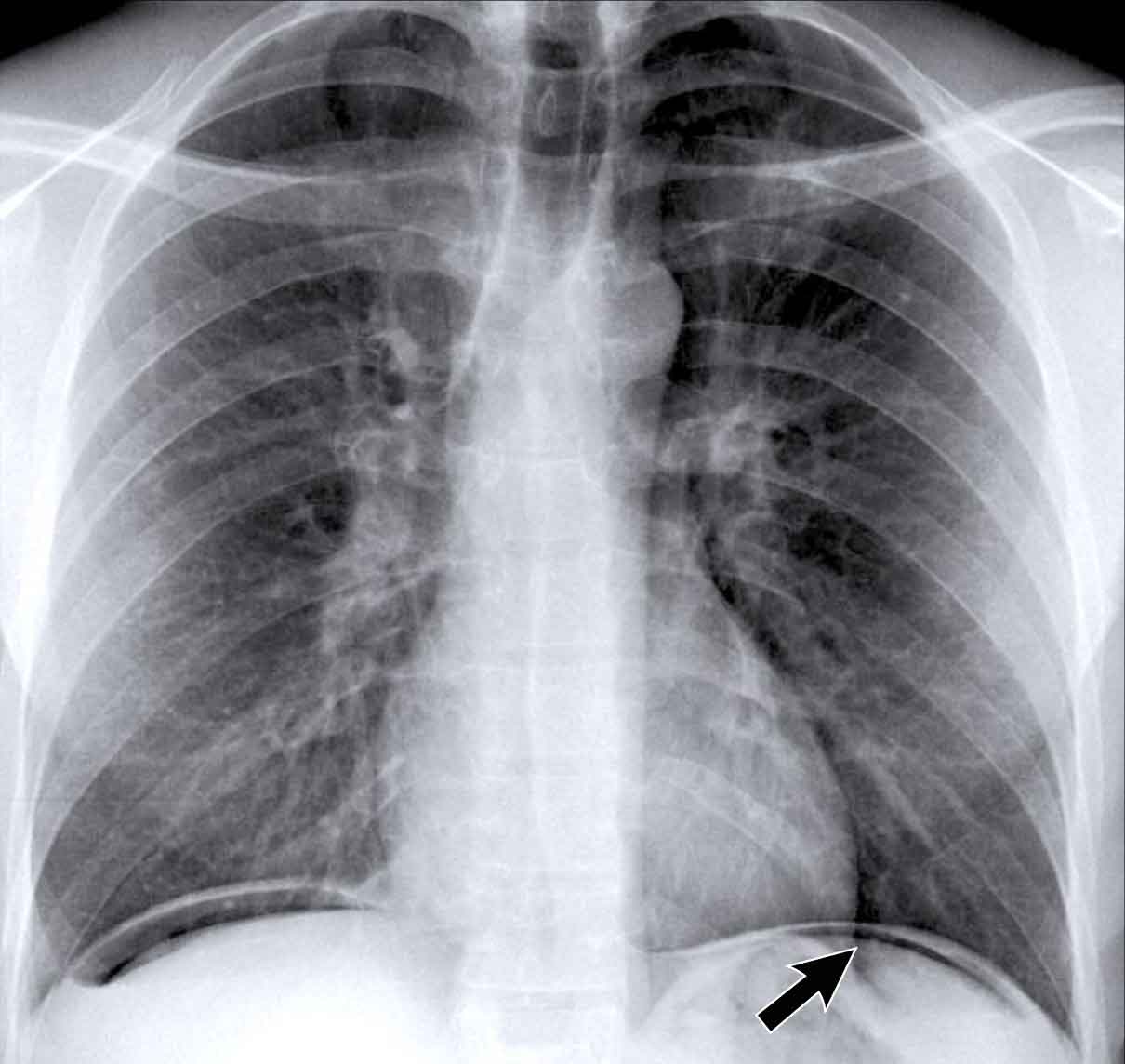
Hidden Areas (3): Pneumonia Below the Diaphragm
In this case, a pneumonia was primarily located below the right diaphragmatic dome (yellow arrow), within the posterior basal segment of the right lower lobe.
- On the lateral view, there is an increase in opacity over the lower thoracic vertebrae, indicating lower lobe consolidation (arrow).
- Again, image magnification may be necessary for adequate assessment.

Hidden Areas (4): Retrocardiac Opacity
Initial review of the CXR reveals a subtle increase in density in the retrocardiac region (blue area), which requires careful attention.
- This was confirmed to be a left lower lobe pneumonia.
- Always correlate with the lateral view, where consolidation in the lower thoracic spine region is a key clue.
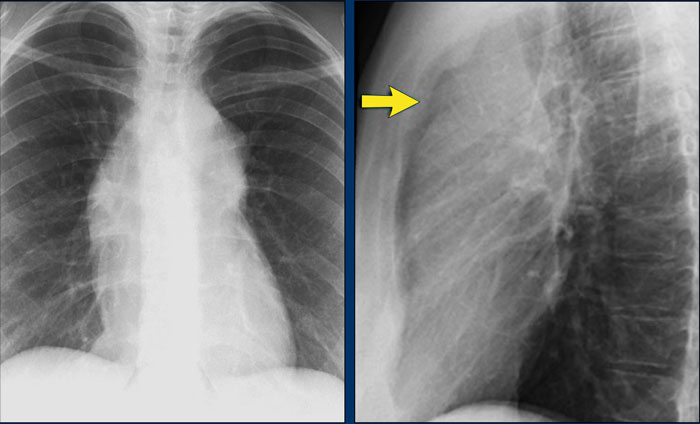
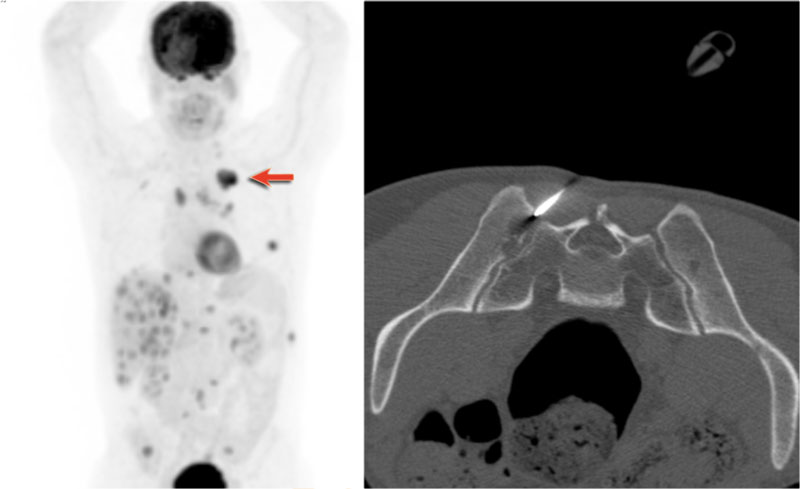
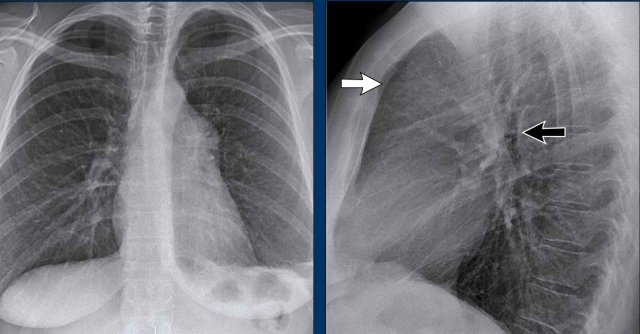
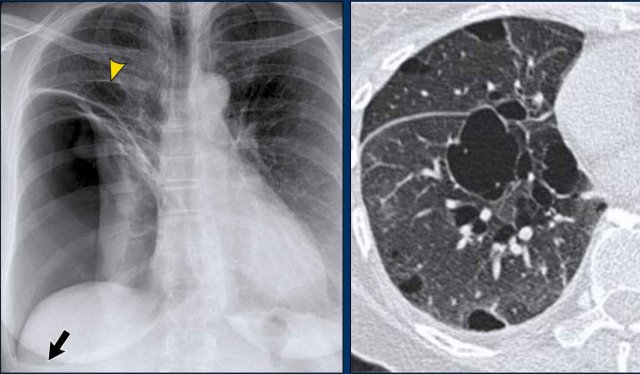
Hidden area (5): Mass Behind the First Rib
In some patients, an accessory joint at the anterior aspect of the first rib may simulate a mass, as we learned earlier.
However this area is also a "hidden zone", where true lesions can be masked.
- In this case, a small lung carcinoma was obscured by the left first rib on the PA view.
- On the lateral film, the lesion is visible in the retrosternal space.
Continue with the PET-CT...
Subsequent PET-CT imaging confirmed a hypermetabolic tumor (arrow), with metastases to the bone and liver.
- Diagnosis was confirmed via biopsy of an osteolytic metastasis in the iliac bone.
Hidden Areas (6): Subtle Consolidation Behind the Heart
In another example, there is a subtle left lower lobe consolidation localized to the retrocardiac area—again, a commonly overlooked region.
- On the lateral view, the pathology manifests as increased density over the lower thoracic vertebrae.
- Consistent with posterior lower lobe pneumonia.
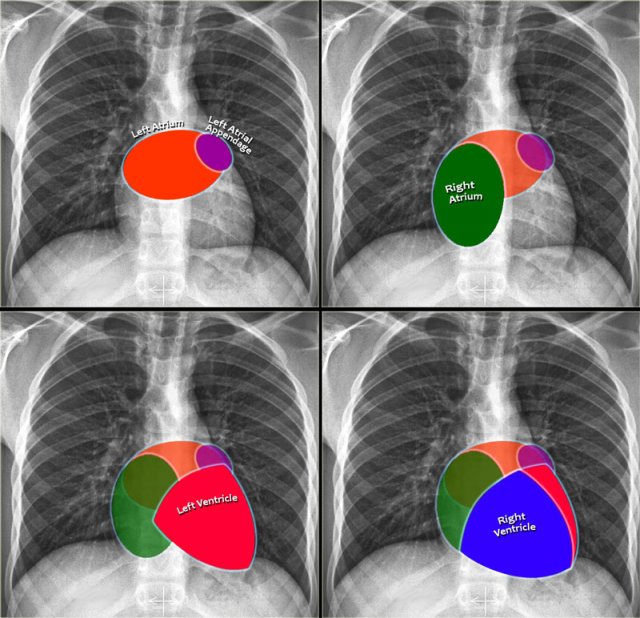
Heart and Pericardium
Cardiac Contours on Chest Radiography
On a standard chest radiograph, only the external contours of the heart are visible. In most cases, we can assess overall heart size and cardiac silhouette, but it is difficult to evaluate individual chambers. Nonetheless, understanding the anatomical positions of the cardiac compartments aids in interpreting shape and contour changes associated with chamber enlargement.
Left Atrium (LA)
It is the most posterior cardiac chamber and it receives oxygenated blood from the pulmonary veins, which enter the left atrium almost horizontally. The left atrial appendage is occasionally visible as a small outpouching just below the pulmonary trunk (best seen on lateral view).
Radiographic signs of left atrial enlargement:
- PA view: Bulging of the upper right heart border and widening of the carinal angle due to splaying of the main bronchi.
- Lateral view: Bulging of the posterior-superior cardiac contour.
Right Atrium (RA)
Receives deoxygenated blood from the superior and inferior vena cava.
Radiographic sign of right atrial enlargement:
- PA view: Outward displacement of the right heart border.
Left Ventricle (LV)
Is situated posterior and leftward to the right ventricle.
Radiographic signs of left ventricular enlargement:
- PA view: Leftward enlargement of the cardiac silhouette
- Lateral view: Bulging of the inferior-posterior contour of the heart.
Right Ventricle (RV)
Location: The most anterior chamber, directly posterior to the sternum.
Radiographic signs of right ventricular enlargement:
- PA view: Enlargement may push the heart silhouette leftward and in severe cases, the left heart border may be formed by the RV.
- Lateral view: Progressive filling of the retrosternal space, starting inferiorly and moving upward with increasing RV size.
Chamber-Specific Contours on Lateral View
- Left Atrium: Forms the upper posterior heart border; enlargement causes posterior bulging.
- Left Ventricle: Forms the lower posterior heart border; enlargement causes posteroinferior displacement.
- Right Ventricle: Occupies the lower retrosternal space; enlargement fills the retrosternal clear space superiorly.
Case Examples
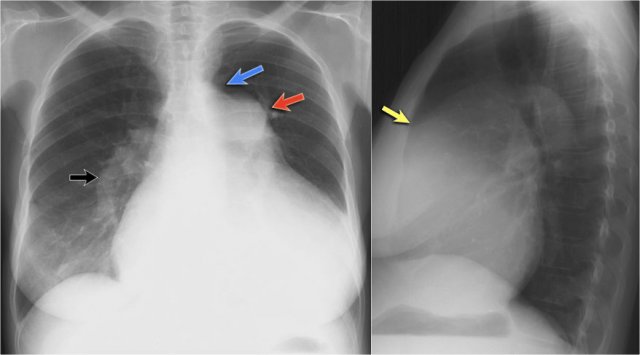
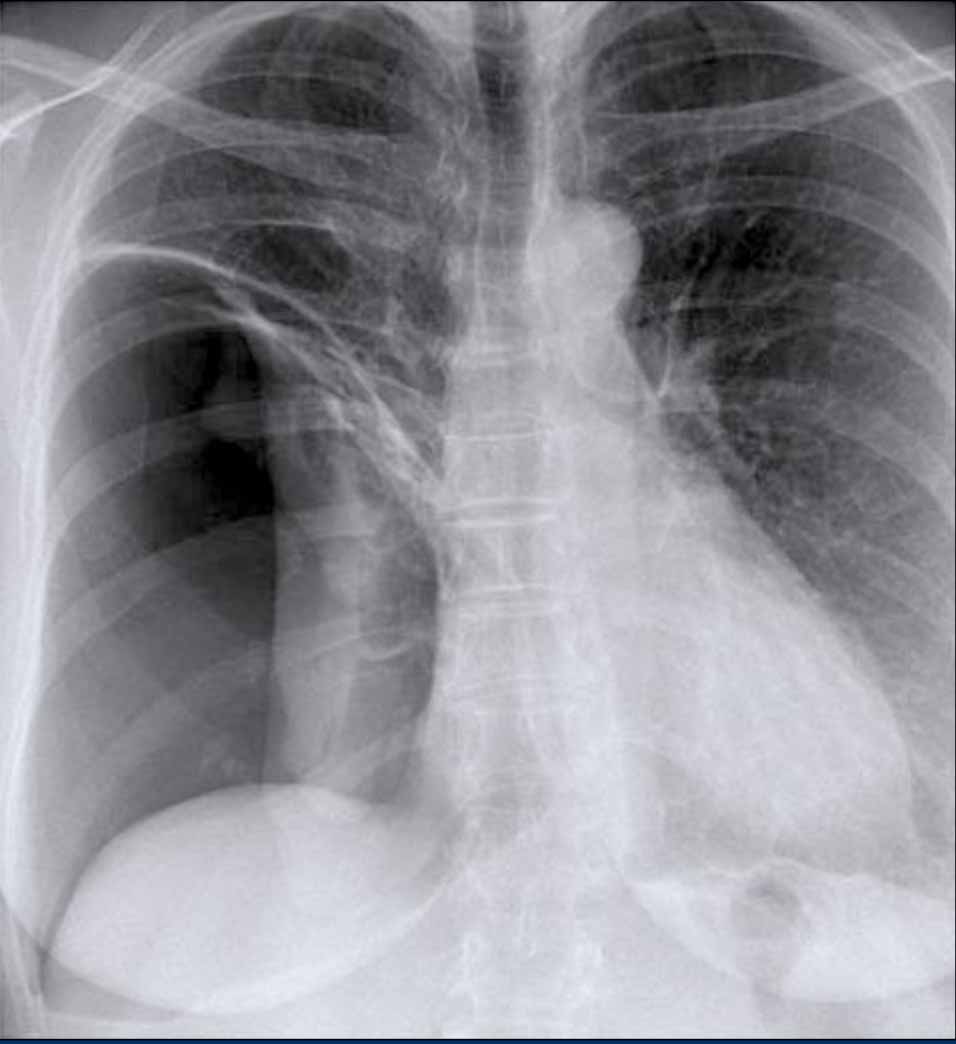
Left Atrial Enlargement
- Patient with a history of chronic mitral valve disease and valve replacement.
- Extreme dilation of the LA leads to bulging of both the right upper cardiac contour (black arrows) and posterior heart border on lateral view (blue arrow).
Right Ventricular Enlargement
First study the PA and lateral chest film and then continue reading.
Findings
- Chest radiographs show massive cardiomegaly, predominantly due to right ventricular dilation (yellow arrow on lateral view).
- Small aortic knob (blue arrow), with dilation of the pulmonary trunk and right lower pulmonary artery.
- Findings suggest a left-to-right shunt with secondary pulmonary hypertension.
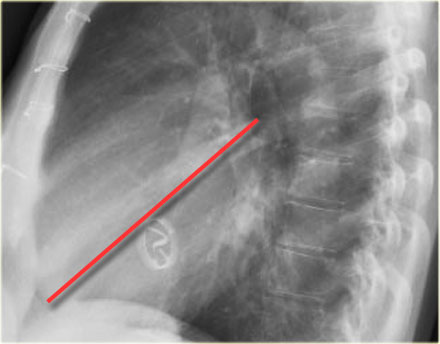
Valvular Anatomy on Lateral Radiograph
- To localize cardiac valves on lateral view, draw a line from the carina to the cardiac apex:
- Above the line: Aortic and pulmonic valves
- Below the line: Tricuspid and mitral valves (4)
This line helps to approximate valve locations and assess for chamber-specific enlargement.
Notice the extreme dilatation of the left ventricle as seen on this lateral view.
Cardiac incisura
On the right side, the lung usually lies directly against the anterior chest wall.
On the left side, the inferior part of the lung may not reach the anterior chest wall due to interposition of the heart, pericardial fat, or pericardial effusion.
This creates a soft tissue density on the anteroinferior aspect of the lateral view, called the cardiac incisura.
Note:
- The cardiac incisura is a normal finding and should not be mistaken for pathology in the lingula or right middle lobe.
Click image to enlarge...
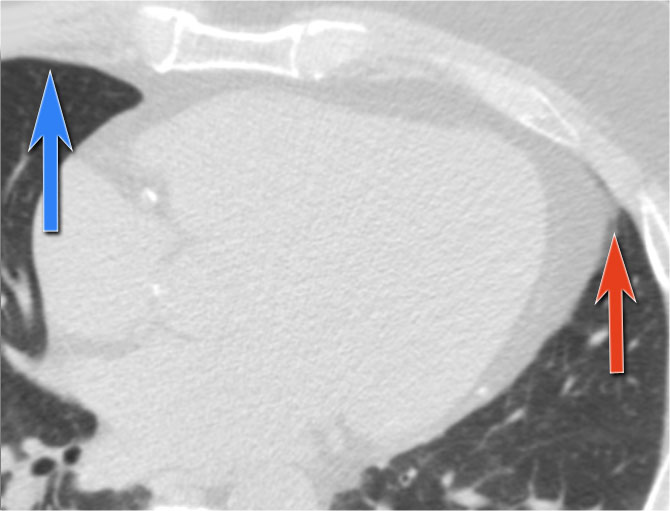
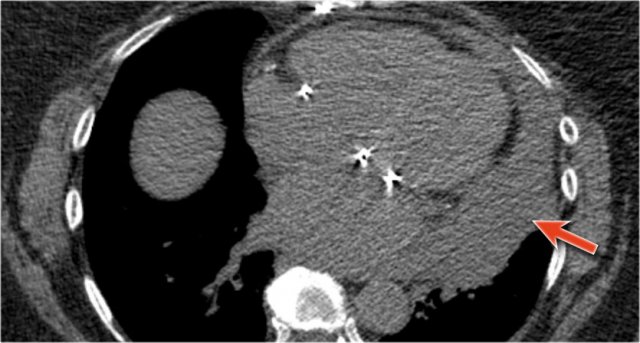
CT correlation
The explanation for the cardiac incisura is seen on this CT-image.
At the level of the inferior heart, the right lower lobe (blue arrow) is often seen extending more anteriorly than the left lower lobe (red arrow) , explaining the asymmetry of the cardiac incisura.
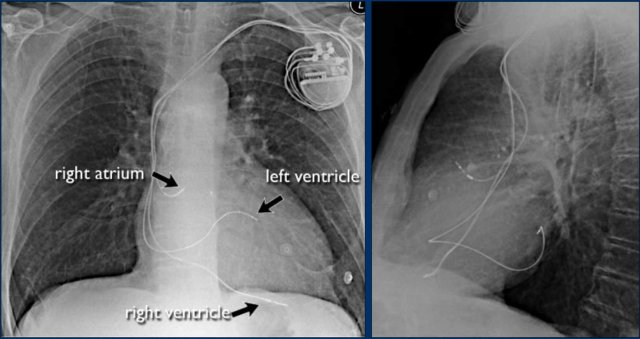
Cardiac Pacemakers
There are various types of cardiac pacing devices, each with specific lead configurations.
In this example:
- Right atrial lead
- Right ventricular lead
- Left ventricular lead via the coronary sinus (used in cardiac resynchronization therapy)
Indication for cardiac resynchronization therapy:
- Patients with ventricular dyssynchrony benefit from biventricular pacing, which improves ventricular coordination and enhances cardiac output.
Pericardial effusion
When encountering an enlarged cardiac silhouette on chest radiography, it is essential to consider pericardial effusion as a potential mimic of cardiomegaly.
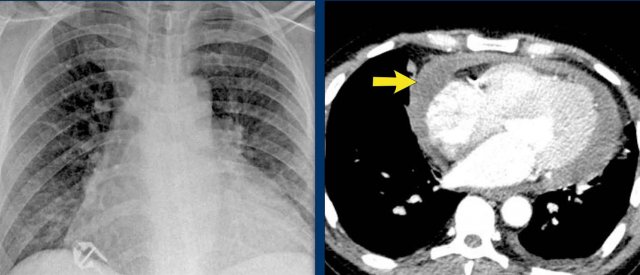
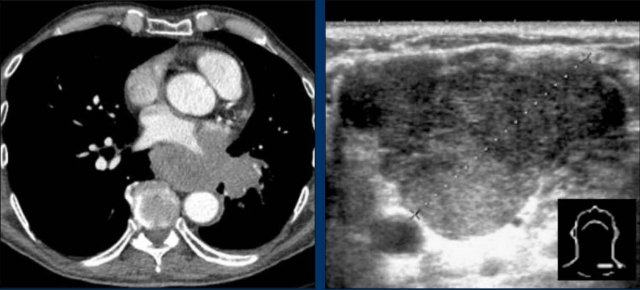
Case Example 1: Pericardial Effusion Mimicking Cardiomegaly
- On the chest radiograph, the patient appears to have a dilated heart.
- However, CT imaging clearly demonstrates that the apparent enlargement is due to significant pericardial fluid accumulation, not true myocardial chamber enlargement.
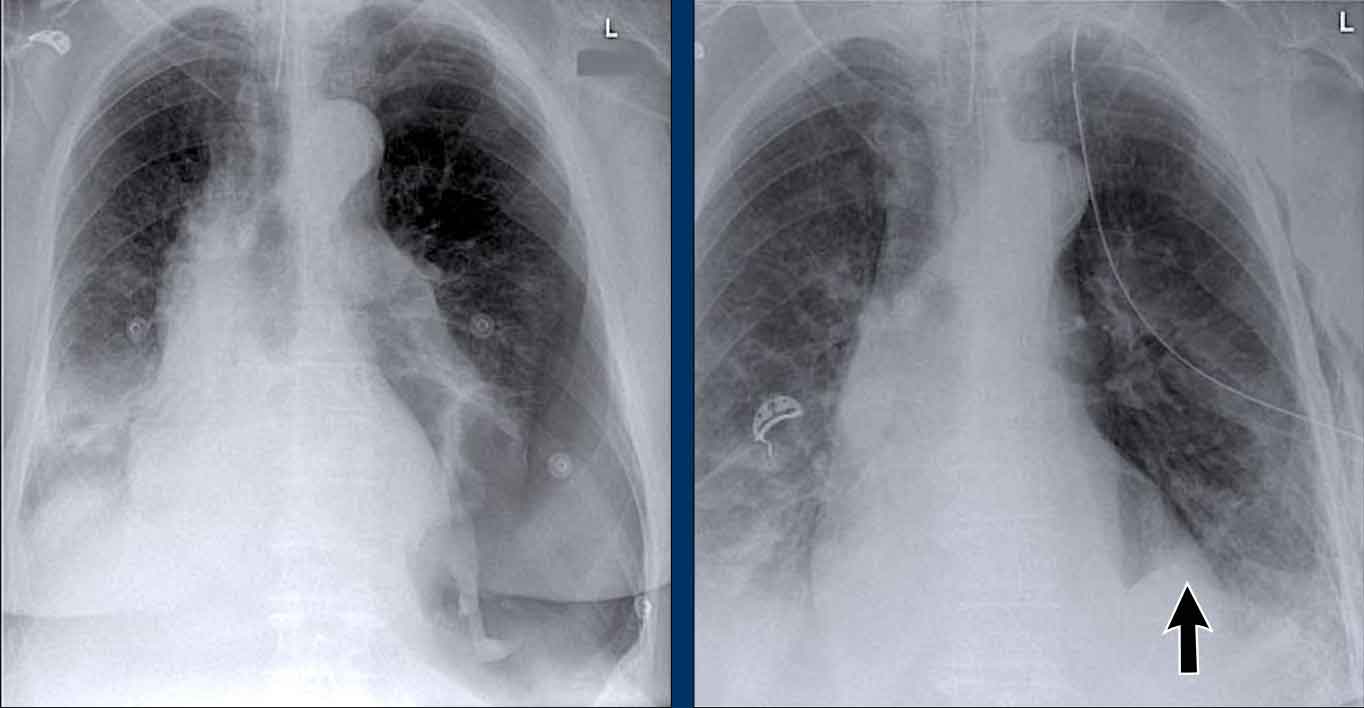
Postoperative Pericardial Hemorrhage
In patients with recent cardiac surgery, a sudden change in heart size on chest X-ray should raise suspicion for pericardial bleeding, which may be life-threatening.
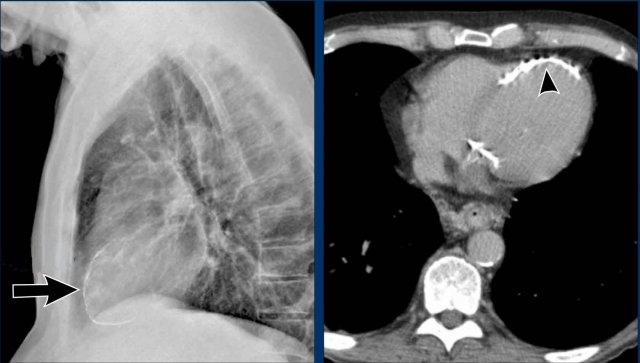
Case Example 2:
- A postoperative patient showed a change in the cardiac silhouette.
- Echocardiography detected only a minimal pericardial effusion.
Case Example 2 - CT imaging
- CT imaging revealed a large posterior pericardial effusion compressing the left ventricle (blue arrow: effusion; red arrow: compressed, contrast-filled left ventricle).
- Surgical exploration confirmed a large posterior pericardial hematoma.
Note: Minimal anterior fluid on ultrasound may underestimate the true volume if the effusion is loculated posteriorly, highlighting the value of CT in postoperative cases.
Especially in patients who had recent cardiac surgery an enlargement of the heart figure can indicate pericardial bleeding.
This patient had a change in the heart configuration (importance of prior imaging) and pericardial bleeding was suspected.
Ultrasound demonstrated only a minimal pericardial effusion.
Case Example 3: Valve Replacement & Heart Failure
Post-valve replacement, a patient presents with a markedly enlarged cardiac silhouette on chest X-ray.
Findings
- A large cardiac silhouette
- There is evidence of pulmonary vascular redistribution, suggesting congestive heart failure.
Case Example 3: CT imaging
CT demonstrates a large pericardial effusion.
Tip
Always compare postoperative chest films with preoperative imaging to detect interval changes such as effusions or evolving heart failure.
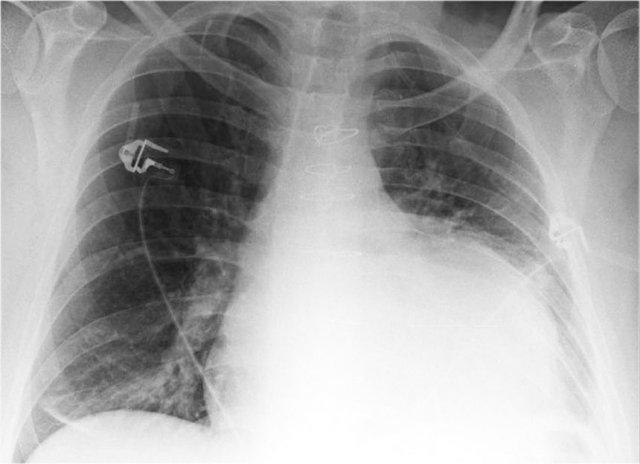
Cardiac and Pericardial Calcifications
- Coronary artery calcifications (indicative of atherosclerosis).
- Valvular calcifications (commonly involving the aortic and mitral valves).
- Pericardial Calcification are less common and may indicate chronic pericardial disease, particularly constrictive pericarditis. Appears as linear or curvilinear calcifications along the pericardial contour.
Here we see pericardial calcifications which can be associated with constrictive pericarditis.
Myocardial Calcification vs. Pericardial Calcification:
- Myocardial infarction-related calcification can resemble pericardial calcification.
- Distinction: Myocardial calcifications follow the contour of the left ventricle and are located within the myocardium, not along the pericardium.
In this case there are calcifications that look like pericardial calcifications on the chest X-ray, but these are myocardial calcifications in an infarcted area of the left ventricle.
Notice that they follow the contour of the left ventricle.
Pericardial fatpad
Pericardial fat deposition is common.
Occasionally, a prominent fat pad is visualized on chest radiography or CT.
In rare cases, fat pad necrosis may occur, mimicking conditions like epiploic appendagitis.
It presents with acute pleuritic chest pain in otherwise healthy individuals, but is self-limiting and benign.
Pericardial cyst
Pericardial cysts are benign lesions that are anatomically connected to the pericardium and typically contain clear, serous fluid.
The majority of pericardial cysts are located in the anterior cardiophrenic angle, more frequently on the right side.
However, they may also be identified more superiorly, within the pericardial recesses at the level of the proximal ascending aorta and main pulmonary arteries.
Most patients remain asymptomatic.
On chest radiography, a pericardial cyst may mimic an elevated left hemidiaphragm (black arrow).
However, CT more clearly demonstrates a fluid-filled cystic lesion contiguous with the pericardium (yellow arrow).
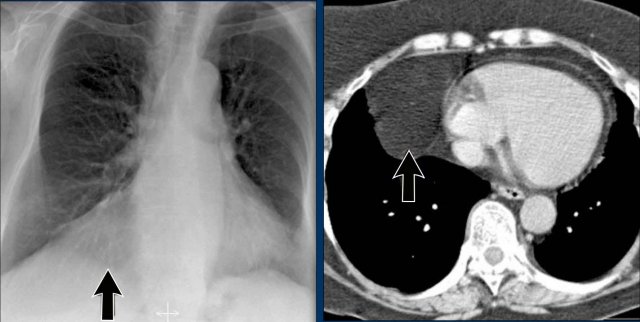
Hili
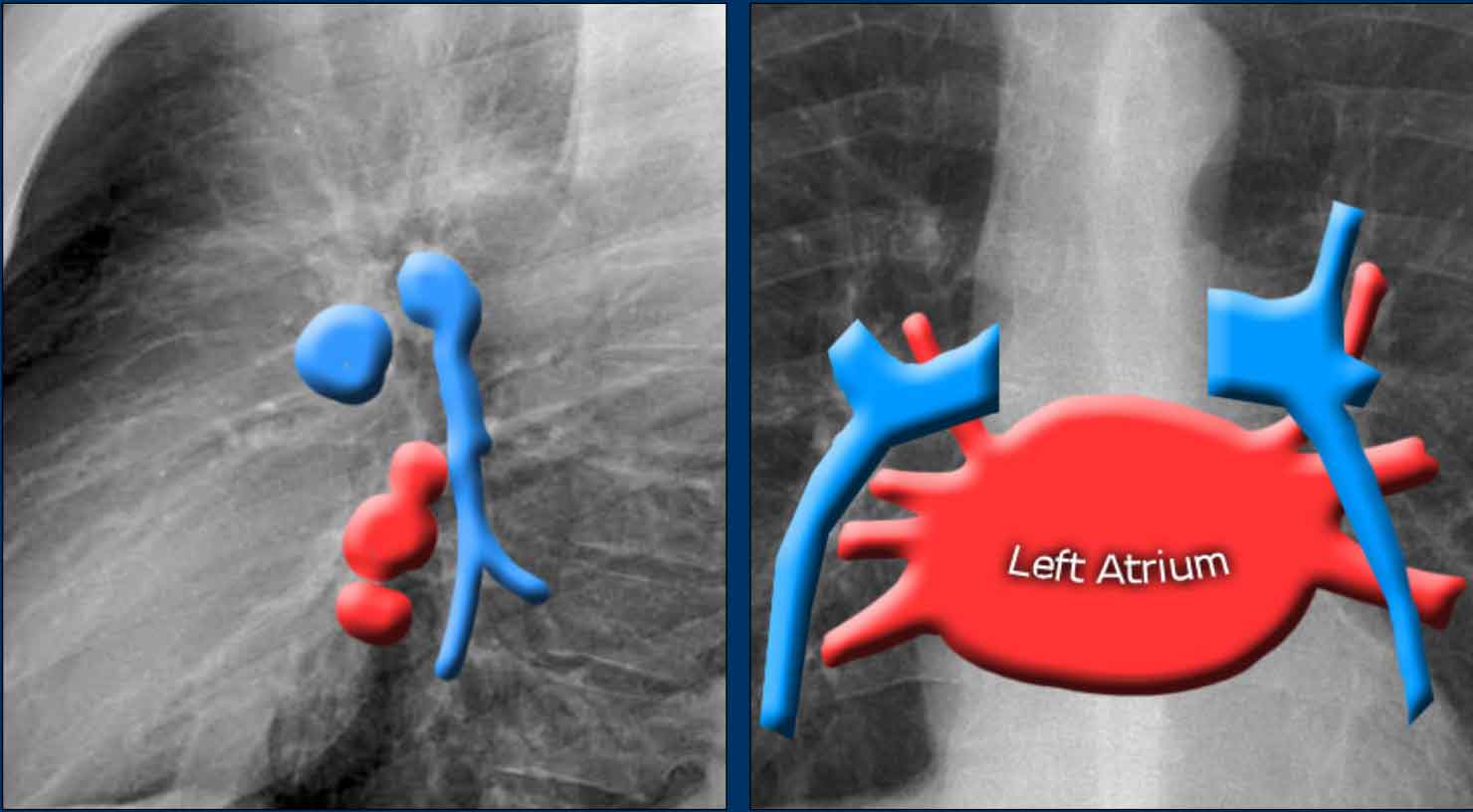
The normal hilar shadow on chest radiography is predominantly vascular in nature—comprising approximately 99% of pulmonary arteries and, to a lesser extent, pulmonary veins (1).
These vascular structures have well-defined, smooth margins and demonstrate normal branching patterns.
Image
Thick coronal slab MIP at the level of the hili.
An important anatomical consideration is that the left hilum is normally situated higher than the right.
This relationship arises from the course of the pulmonary arteries: the left pulmonary artery arches over the left main bronchus, while the right pulmonary artery courses anterior to the right main bronchus, which is typically positioned lower than its left counterpart.
In a minority of cases, the hila may be at the same level, but the right hilum should never be higher than the left.
In this illustration, lower lobe pulmonary arteries are colored blue to indicate deoxygenated blood.
These arteries have a more vertical orientation compared to the pulmonary veins, which run more horizontally toward the left atrium, located inferior to the level of the main pulmonary arteries.
On lateral chest radiographs, both pulmonary arteries and veins are identifiable and should not be misinterpreted as lymphadenopathy. Occasionally, pulmonary veins may appear prominent.
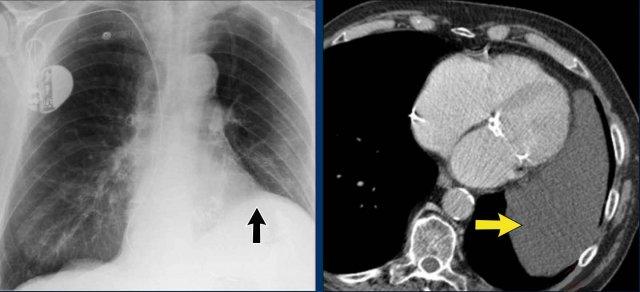
The left main pulmonary artery passes superior to the left main bronchus and lies higher than the right pulmonary artery, which courses anterior to the right main bronchus.
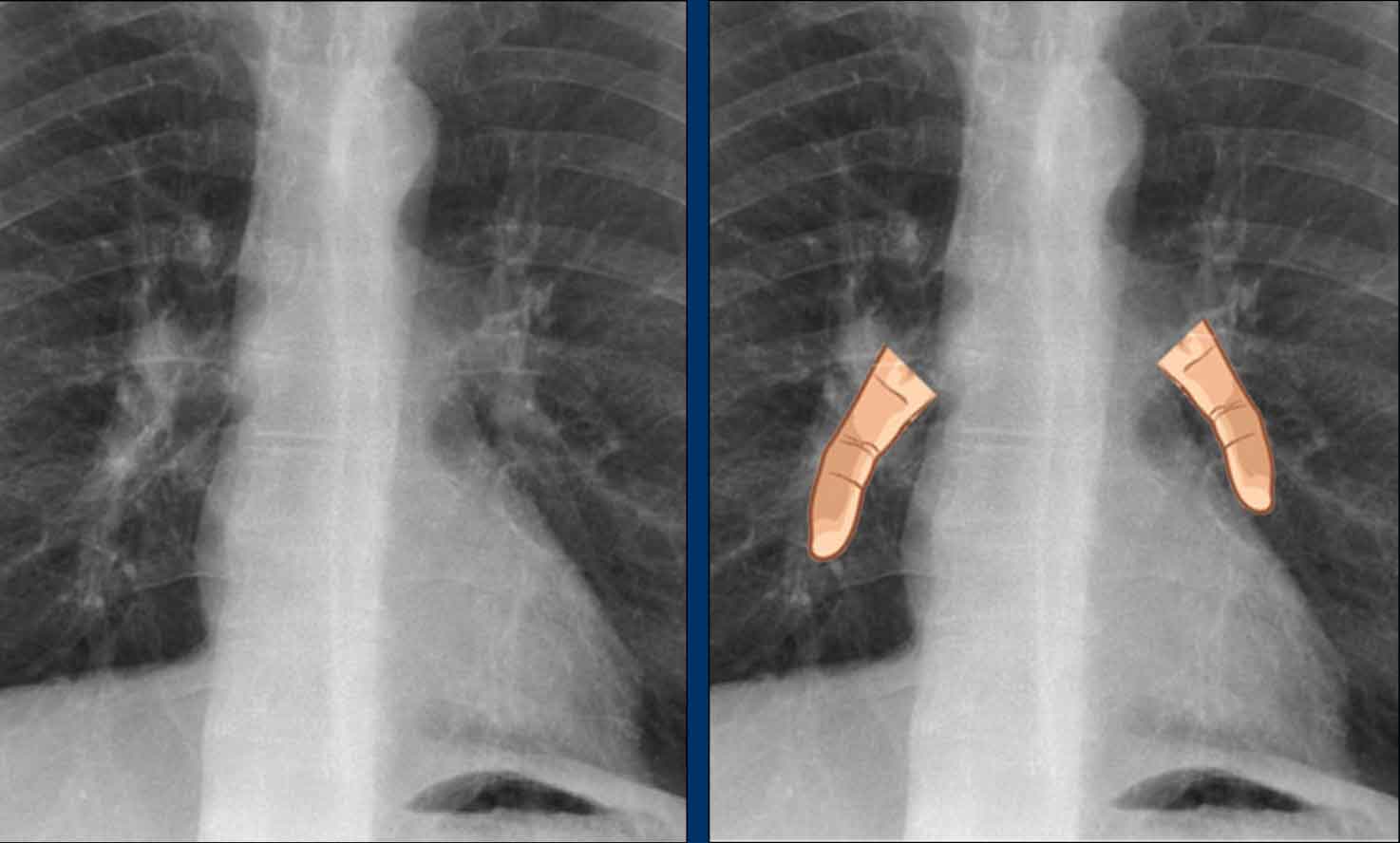
The included images are thick-slab sagittal CT reconstructions of the thorax, which enhance visualization of hilar structures.
The lower lobe pulmonary arteries descend from the hilum in a vertically oriented fashion.
Radiographically, these vessels are colloquially referred to as the “little finger” due to their size and shape, approximating that of a little finger (1).
On PA chest radiographs, the "little finger" of the right lower lobe pulmonary artery is visible in approximately 94% of normal individuals, while on the left side it is visible in about 62% (1).
Clinical Case
A 70-year-old male patient presents following a fall down the stairs, complaining of severe right flank pain.
Imaging Findings
- On the PA chest radiograph, there is an absence of the right fifth digit.
- On the lateral view, there is increased density projected over the lower thoracic spine.
What is your diagnosis?
The findings are consistent with right lower lobe atelectasis.
On the PA view, note the abnormal contour of the right heart border. The right interlobar pulmonary artery is not visualized—this is because it is not surrounded by aerated lung, but rather by the collapsed right lower lobe, which lies adjacent to the right atrium.
On follow-up imaging, the right lower lobe has re-expanded, and the atelectasis has resolved.
This suggests that the atelectasis was likely due to post-traumatic hypoventilation with mucus plugging.
Also noted on the follow-up radiograph is the reappearance of the right fifth finger (black arrow), and restoration of a normal right heart border (white arrow), confirming re-expansion of the lower lobe.
Hilar enlargement
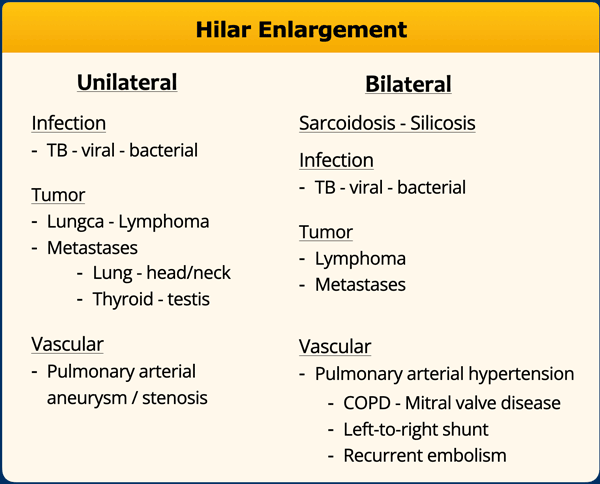
The table summarizes the causes of hilar enlargement.
Normal hili are:
- Normal in position - left higher than right
- Equal density
- Normal branching vessels
Enlargement of the hili is usually due to lymphadenopathy or enlarged vessels.
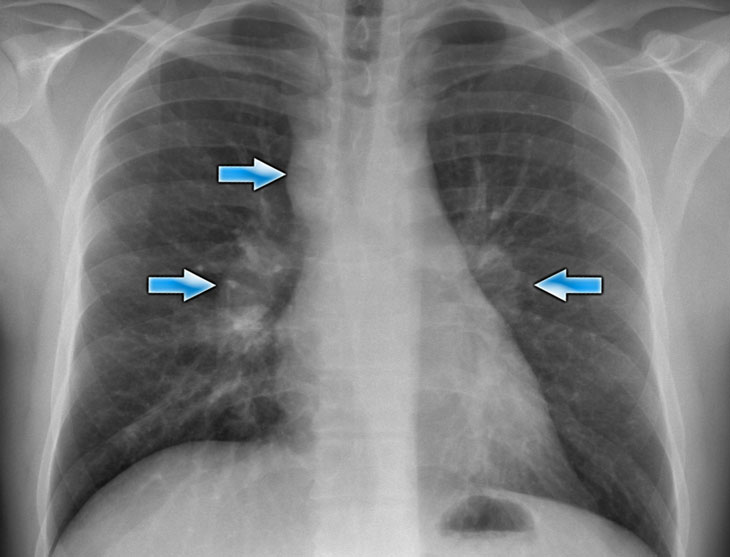
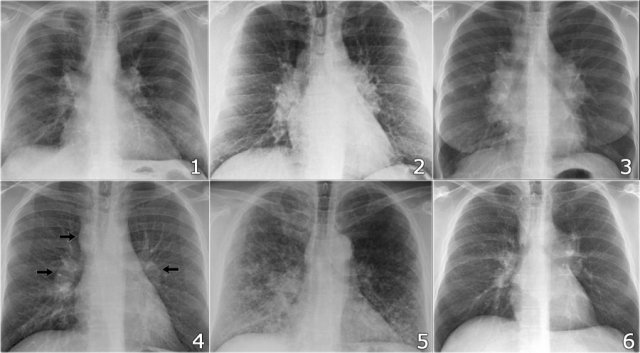
Hilar enlargement - case 1
In this case there is an enlarged hilar shadow on both sides. This could be the result of enlarged vessels or enlarged lymph nodes. A very helpful finding in this case is the mass on the right of the trachea.
This is known as the 1-2-3 sign in sarcoidosis, i.e. enlargement of left hilum, right hilum and paratracheal.
Here some more examples of sarcoidosis.
Click image to enlarge.
- Lymphadenopathy and groundglass appearance of the lungs
- Lymphadenopathy, 1-2-3 sign
- Bulky lymphadenopathy
- 1-2-3 sign
- Nodular lung pattern, no lymphadenopathy
- Hilar and paratracheal lymphadenopathy
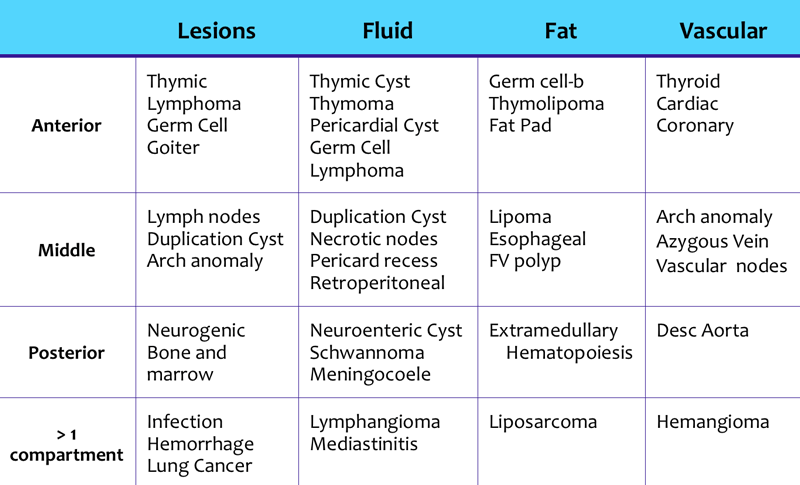
Mediastinum
Mediastinal masses are discussed in more detail in Mediastinal masses.
Here is just a brief overview.
The mediastinum can be divided into an anterior, middle and posterior compartment, each with it's own pathology.
Mediastinal lines
Mediastinal lines or stripes are interfaces between the soft tissue of mediastinal structures and the lung.
Displacement of these lines is helpful in finding mediastinal pathology, as we have discussed above.
Azygoesophageal line
The most important mediastinal line to look for is the azygoesophageal line, which borders the azygoesophageal recess.
This line is visible on most frontal CXRs.
The causes of displacement of this line are summarized in the table.
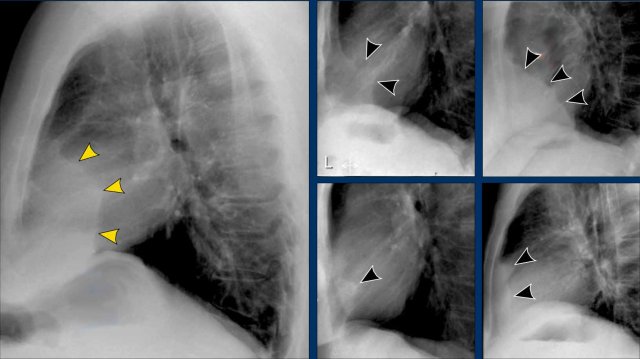
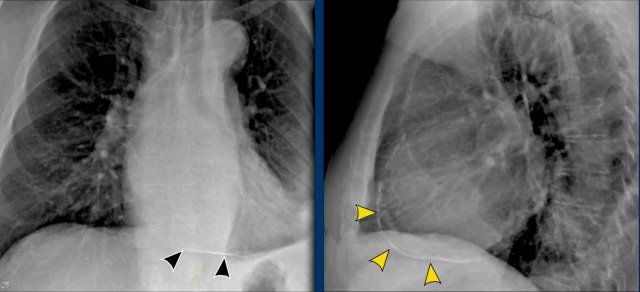
Displacement of the Azygoesophageal Line (1) – Hiatal hernia
A hiatal hernia (arrowheads) is the most common cause of displacement of the azygoesophageal line as seen on the PA-view.
Notice the air within the hernia on the lateral view (black arrow).
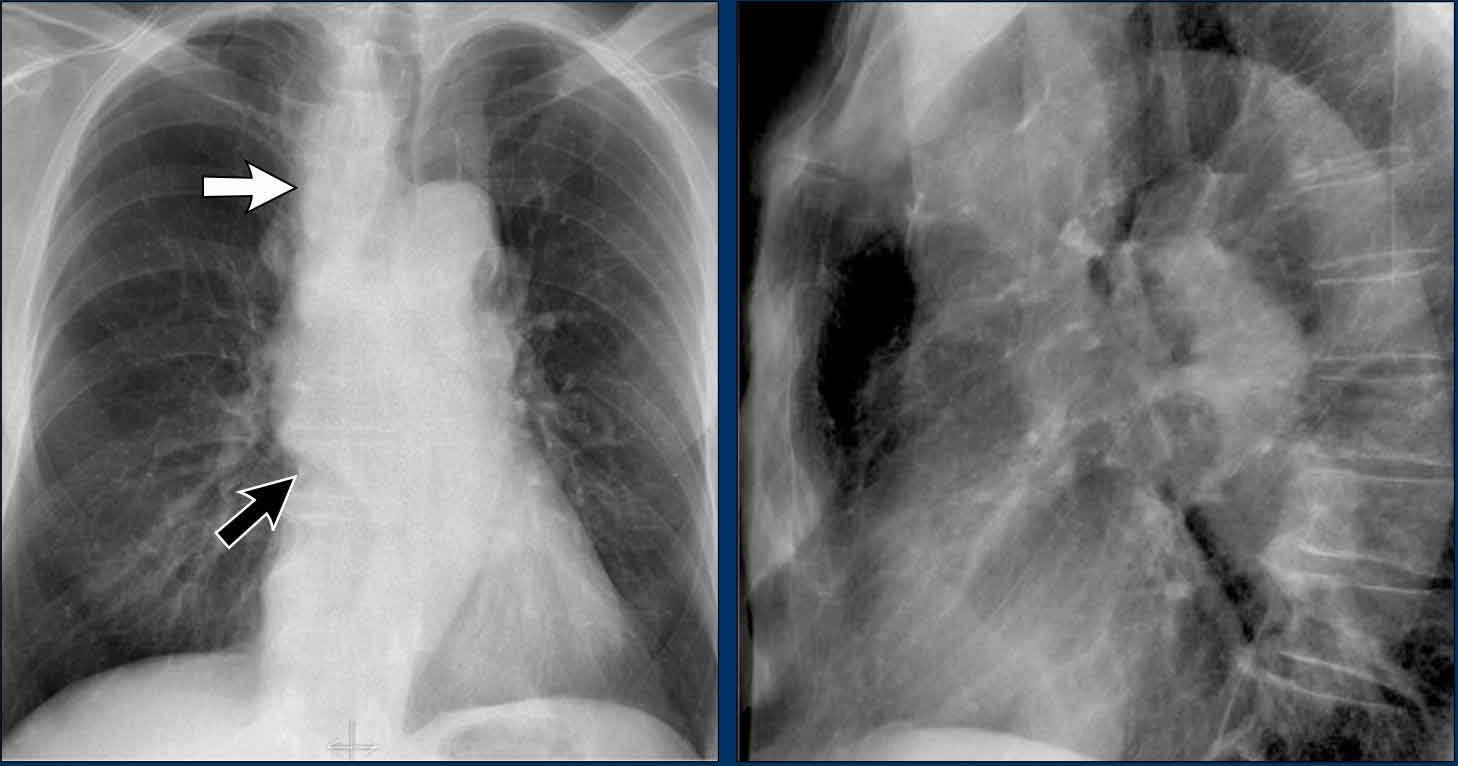
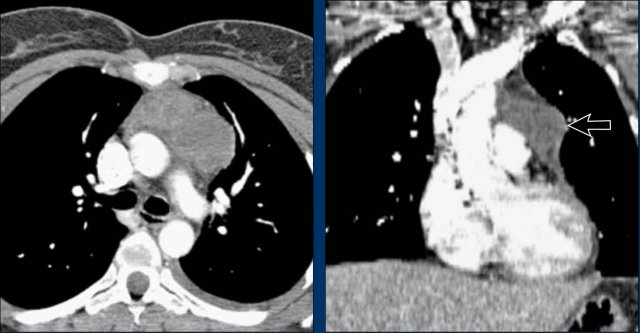
Displacement of the Azygoesophageal Line (2) – Subcarinal Lymphadenopathy
A common cause of displacement of the azygoesophageal line is subcarinal lymphadenopathy (station 7).
On the chest X-ray, note superior displacement of the azygoesophageal line just below the carina, consistent with enlarged subcarinal lymph nodes (black arrow).
Additional right paratracheal lymphadenopathy is seen, displacing the right paratracheal stripe (white arrow) and deviating the trachea to the left.
Continue with PET-CT...
PET Imaging
- PET-CT demonstrates extensive hypermetabolic lymphadenopathy in the mediastinum and neck, which is more conspicuous than on chest radiography.
- Cervical lymph nodes are involved—an important finding as they are accessible for biopsy.
Continue with images of CT and ultrasound...
CT Imaging
- Contrast-enhanced CT shows bulky subcarinal lymphadenopathy displacing the azygoesophageal recess and compressing the left atrium.
- Biopsy of a cervical node confirmed small cell lung carcinoma.
Displacement of the Azygoesophageal Line (3)
First study the chest x-ray.
Then continue reading.
Imaging findings
- Displacement of the azygoesophageal line both superiorly and inferiorly
- Presence of an air-fluid level, consistent with dilated fluid-filled esophagus
- Left perihilar opacity in the region of the lingula, attributed to prior aspiration pneumonia
What is your diagnosis?
Continue with prior Chest X-ray and CT...
Prior Chest X-ray:
- AP view shows a right paratracheal mass
- Azygoesophageal recess not visualized; displaced and paralleling the right atrial border
- Large round opacity in the left lung consistent with aspiration pneumonia
CT Imaging:
- Marked esophageal dilation
- No evidence of mass obstructing the gastroesophageal junction
- Diagnosis: Achalasia
Aortopulmonary window
The aortopulmonary window (AP window) lies between the aortic arch and pulmonary trunk; its lateral contour should appear concave or straight.
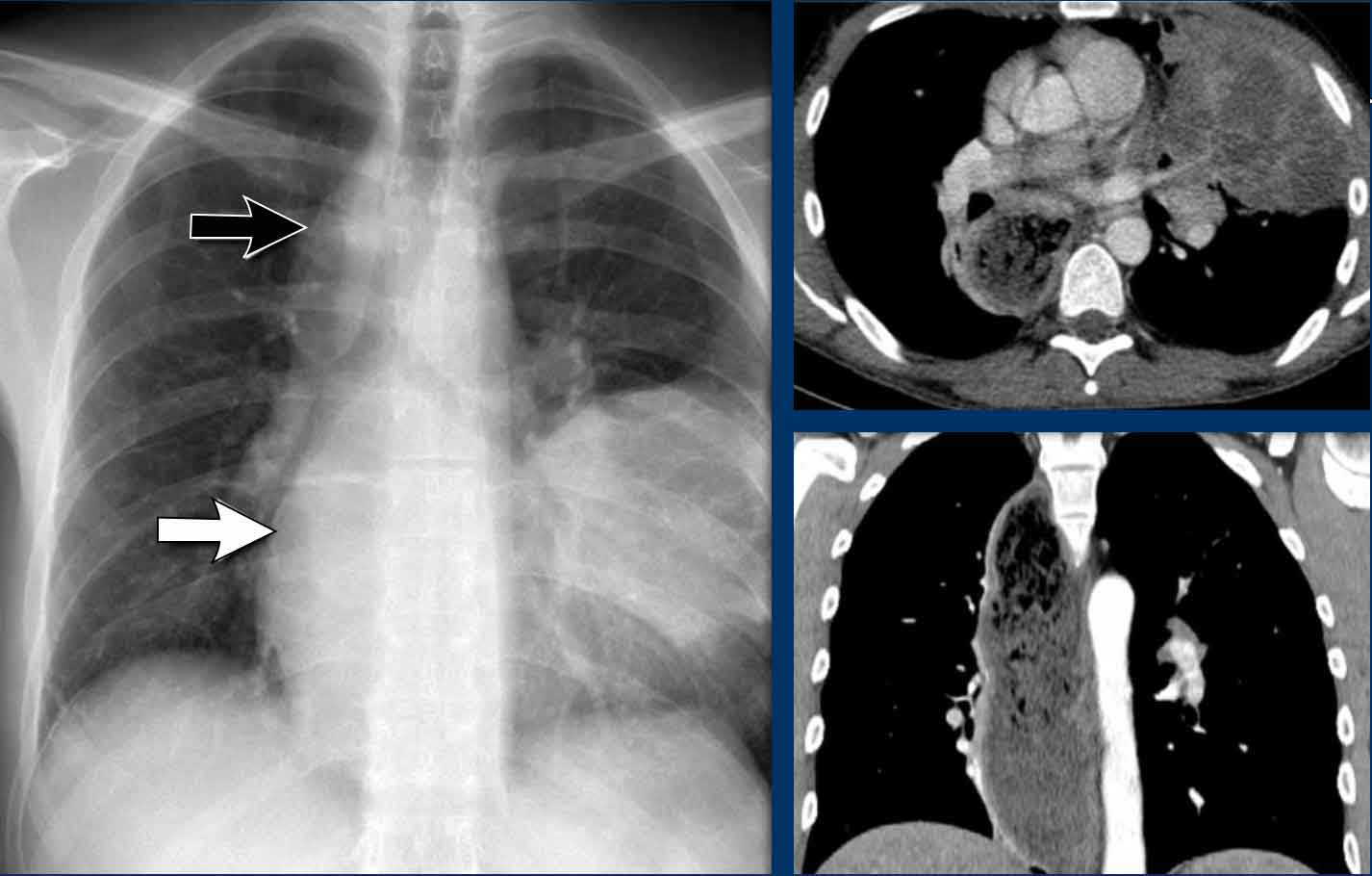
AP window pathology - case 1
Imaging
- PA film shows a mass filling the aortopulmonary window
- Lateral view shows no enlarged pulmonary vessels (black arrow), but a mass projecting into the retrosternal space (white arrow)
Continue with the CT...
CT Imaging
- Mass in the anterior mediastinum is seen.
- Final diagnosis: Hodgkins lymphoma.
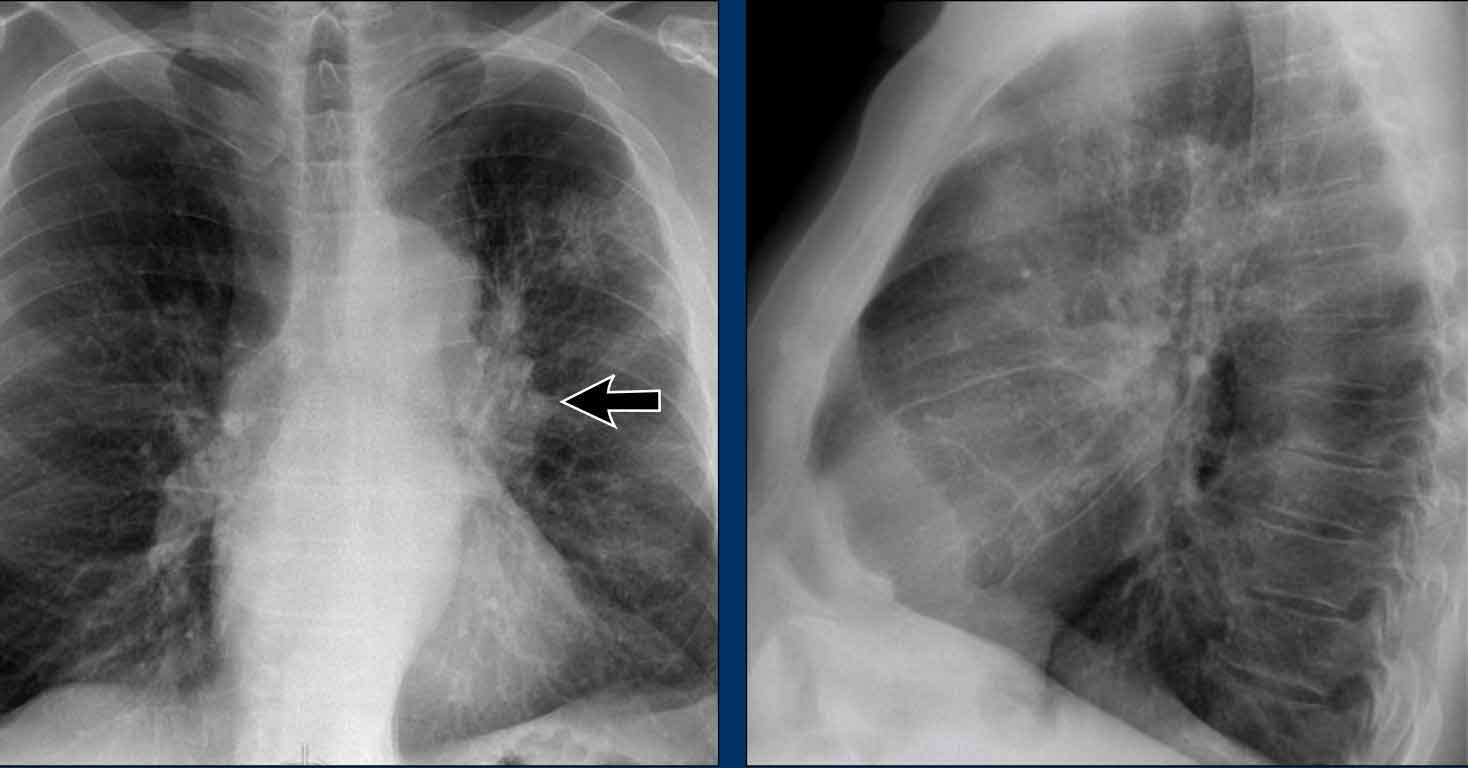
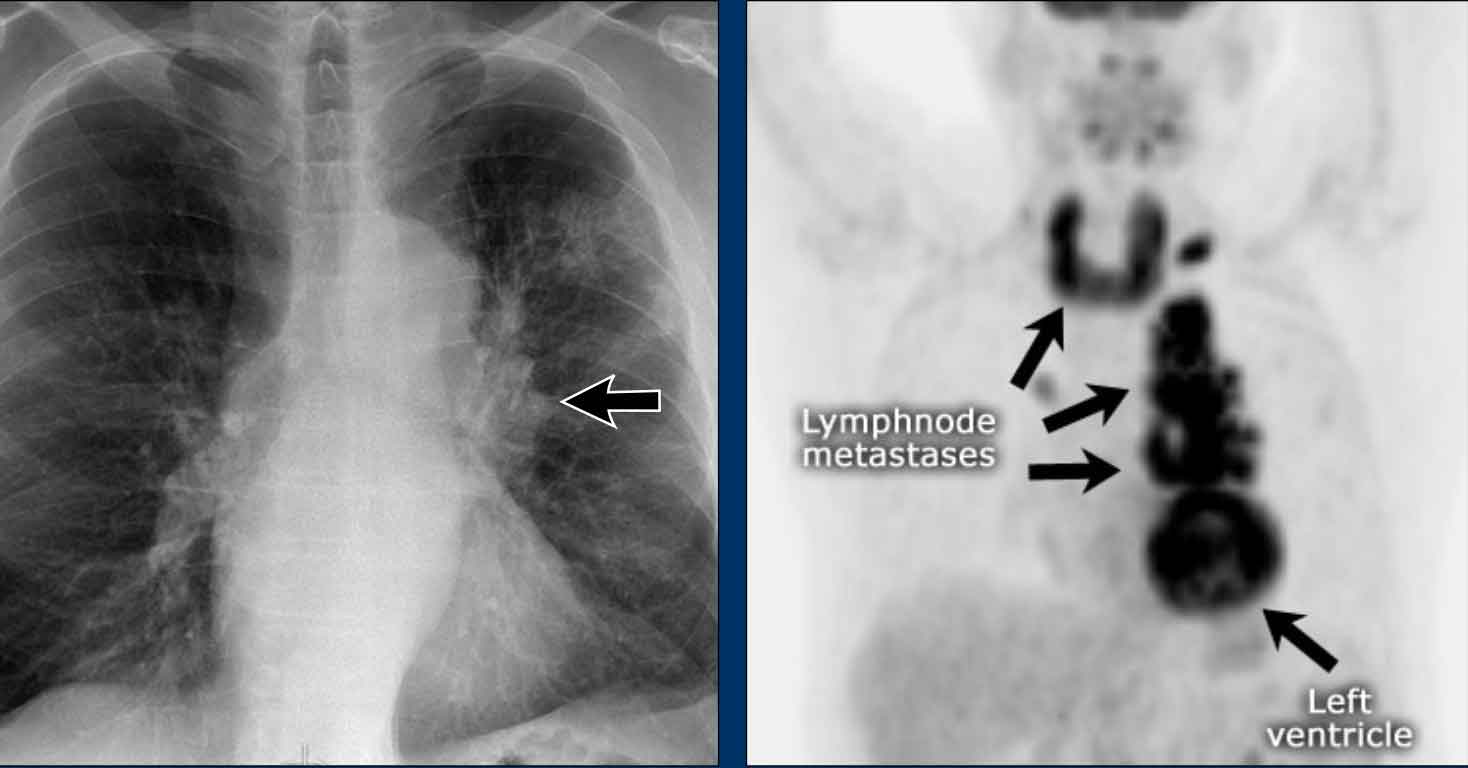
AP window mass - case 2
Imaging
- PA chest X-ray shows a mass occupying the AP window
Continue with the PET-CT...
PET-CT
Lungs
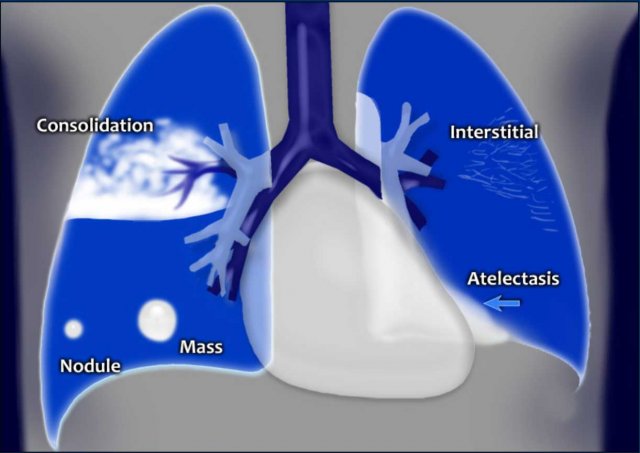
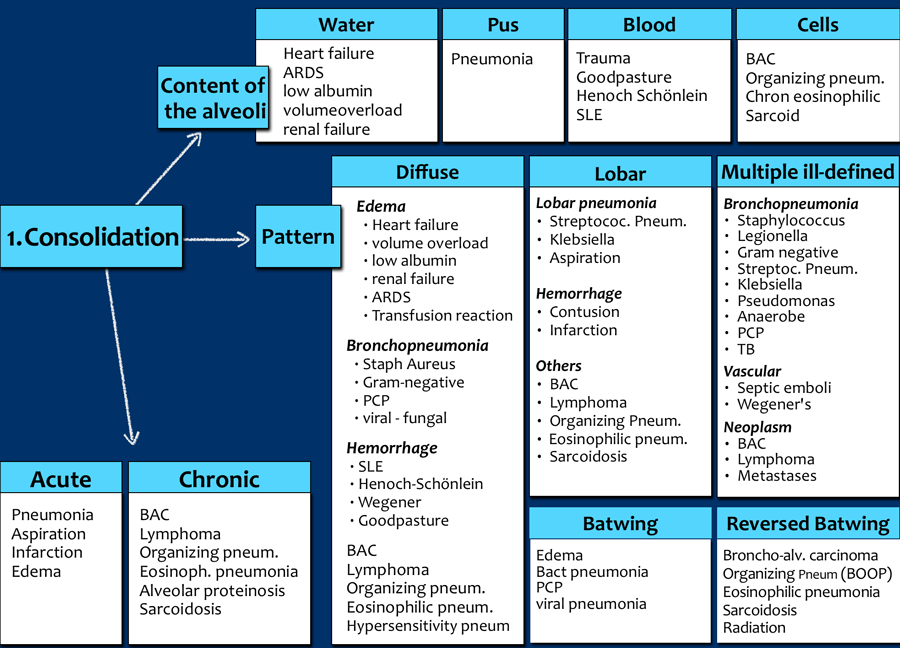
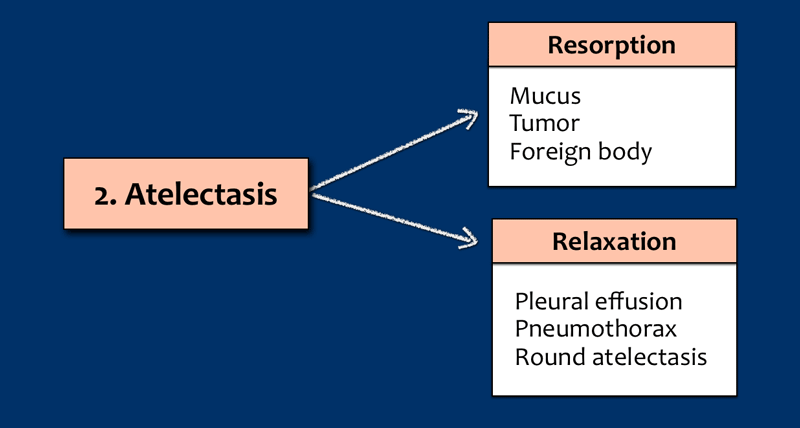
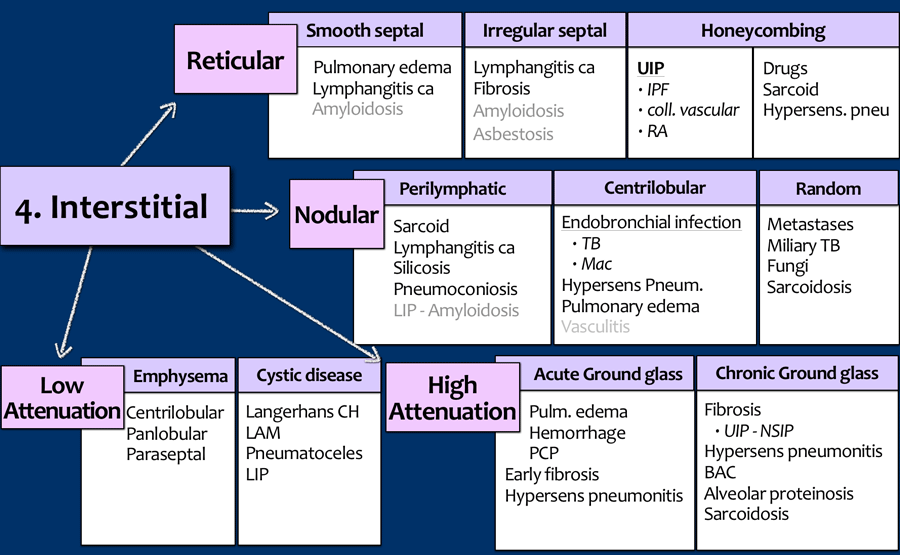
Lung abnormalities mostly present as areas of increased density, which can be divided into the following patterns:
- Consolidation
- Atelectasis
- Nodule or mass - solitary or multiple
- Interstitial
Less frequently areas of decreased density are seen as in emphysema or lungcysts.
These lung-patterns are discussed in Chest X-Ray - Lung disease four pattern approach.
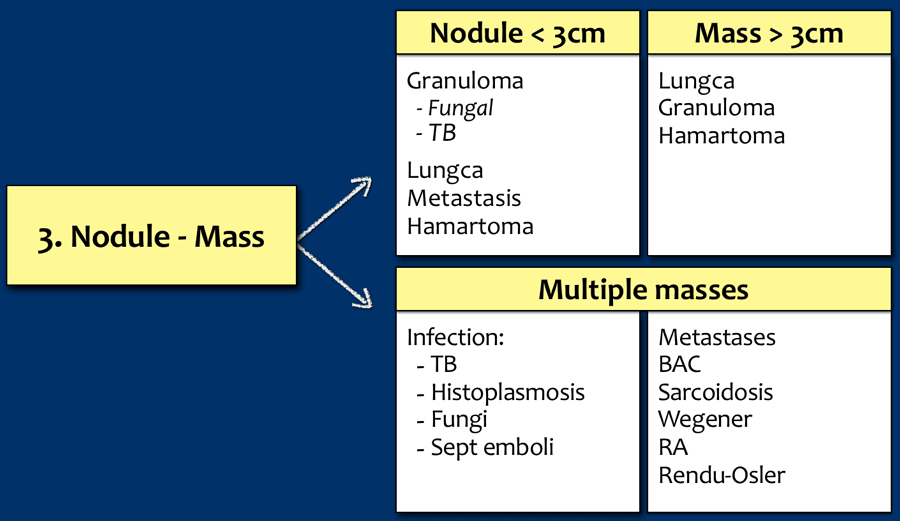
Nodule - Masses
Tap on image to enlarge.
Nodules and masses are discussed here...
Solitary pulmonary node - SPN is discussed here.
Pleura
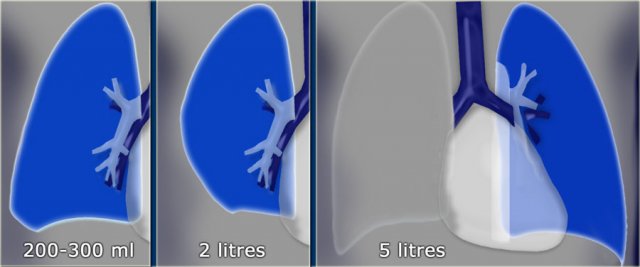
Pleural fluid
Case Example
A patient with bilateral carcinomatous pleuritis.
Findings
- Complete opacification of the right hemithorax.
- Air bronchogram in the right main bronchi (arrowheads), indicating compression atelectasis of the lung due to massive effusion.
Encysted Pleural Fluid ("Vanishing Tumor")
- Encysted pleural effusions may become trapped within the fissures, often mimicking a mass.
- This is sometimes referred to as a “vanishing tumor”, as it resolves with treatment of the underlying effusion.
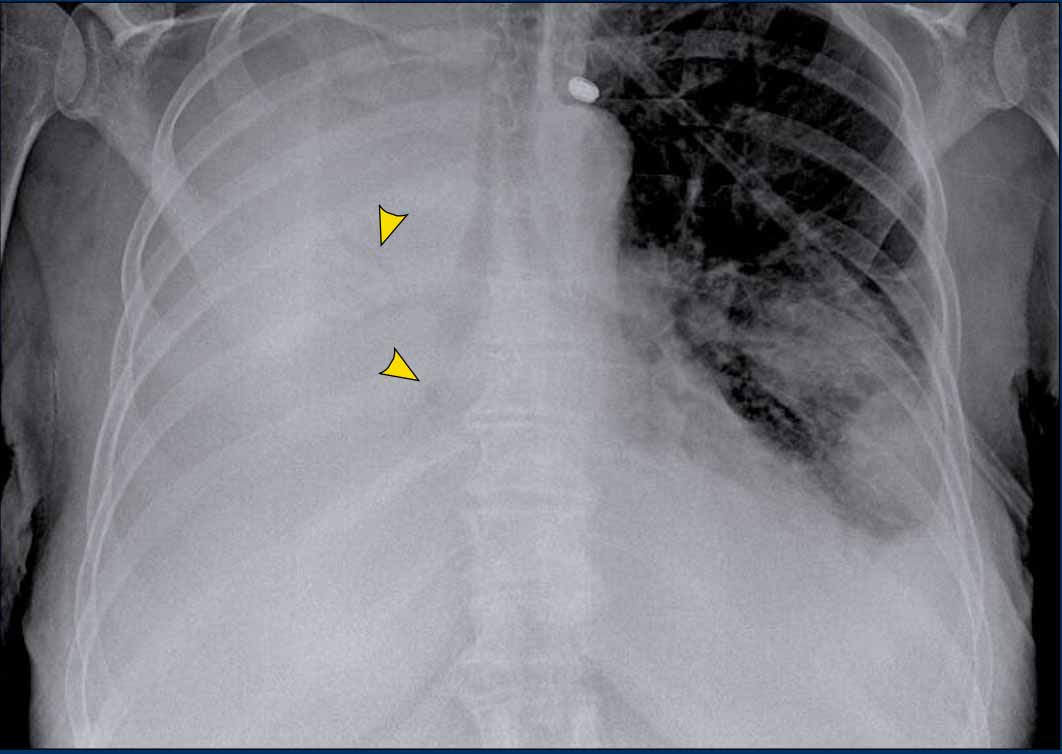
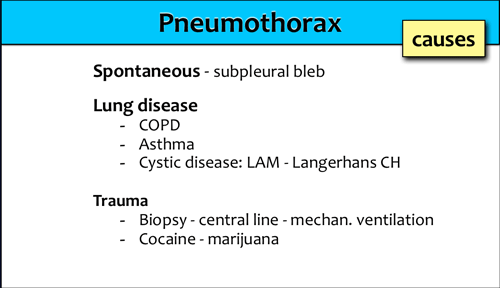
Pneumothorax
Etiologies:
Common causes of pneumothorax include trauma, spontaneous rupture of subpleural blebs, and iatrogenic events.
Another cystic lung disease causing pneumothorax is Langerhans Cell Histiocytosis (LCH), typically seen in smokers.
Case 1
Study the CXR.
There are two important findings.
Then continue reading...
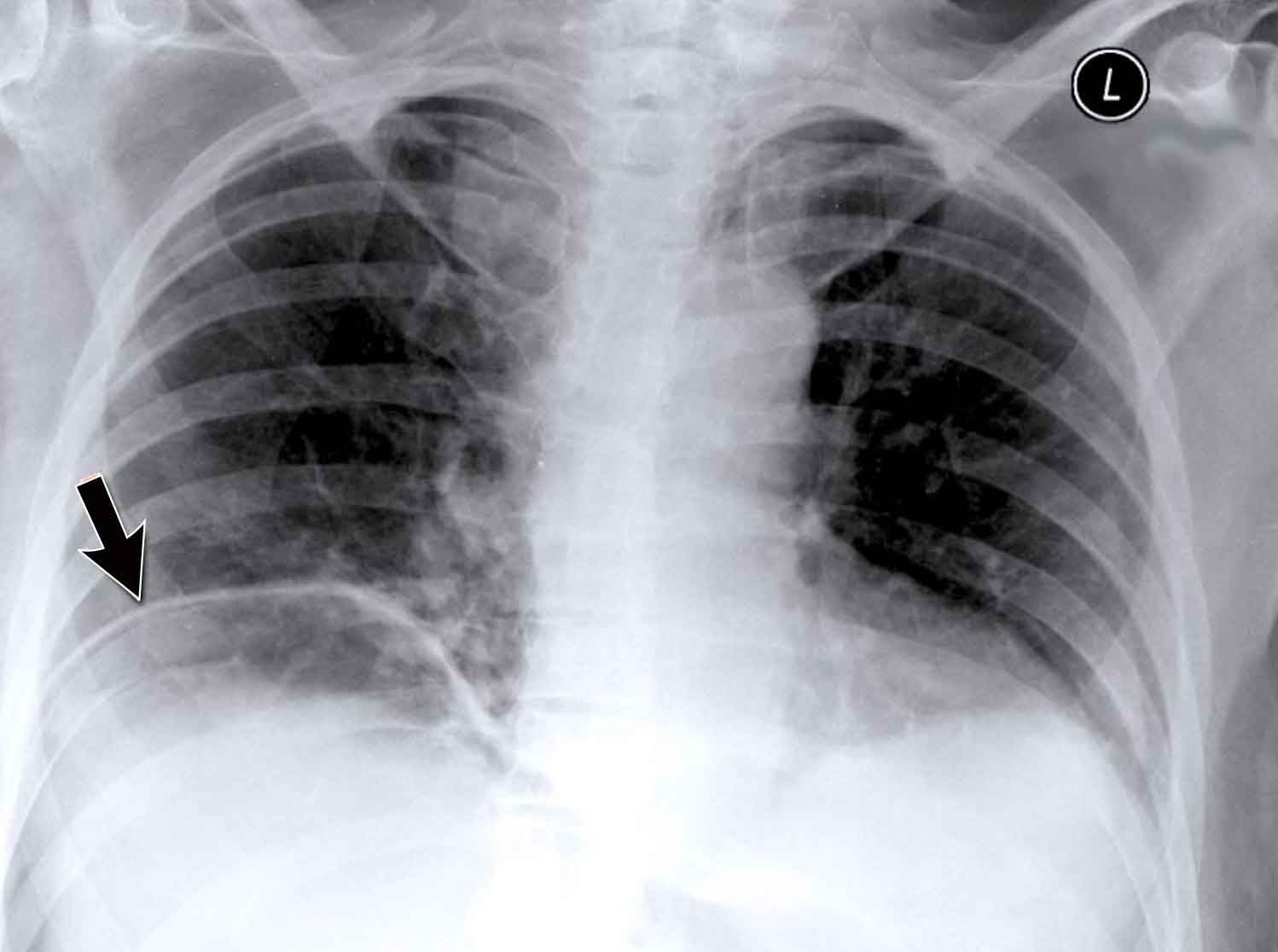
Case 1 – Hydropneumothorax
- Chest X-ray shows a retracted visceral pleura (blue arrow), consistent with pneumothorax.
- A horizontal air–fluid level (yellow arrow) is seen, confirming hydropneumothorax.
Normally there are no straight lines in the human body unless when there is an air-fluid level.
- In small pneumothoraces, this may be the only diagnostic clue.
Case 2 – Pneumothorax
Study the CXR.
There are 3 important findings.
Notice that the mediastinum is slightly displaced to the left.
Does this mean that there is a tension pneumothorax?
Do you have an idea about the cause of the pneumothorax?
Case 2 – Cystic Lung Disease with Hydropneumothorax
- Chest X-ray
- Mediastinal shift to the left
- Air-fluid level (hydropneumothorax) (black arrow)
- Upper lobe adhesions to the chest wall. Maybe this patient was treated for a prior pneumothorax.
- Lung cyst in the right upper lobe (yellow arrowhead)
Conclusion
We are dealing with a woman with a cystic lung disease, who probably had prior pneumothoraces.
The most likely diagnosis is lymphangioleiomyomatosis (LAM), a rare cystic lung disease involving proliferation of smooth muscle, leading to airway obstruction, pulmonary cysts, and recurrent pneumothoraces.
LAM can occur sporadically or in association with tuberous sclerosis complex (TSC).
Pneumothorax Mimic – Skin Fold
- Chest X-ray shows a line mimicking a pneumothorax, but lung markings are visible beyond the line, confirming this is a skin fold artifact.
- Caused by supine positioning and improper cassette placement resulting in a skinfold.
Pneumothorax Mimic – Skin Fold
Additional images demonstrate similar artifacts in another patient with obvious skin folds.
Pneumothorax Detection on Supine Films
- Recognition depends on air volume and patient position.
- Up to 30% of pneumothoraces are missed on supine films.
- Key sign: Deep sulcus sign – lucency at the lateral costophrenic angle extending inferiorly toward the hypochondrium.
Case
- ICU patient on mechanical ventilation with acute respiratory deterioration.
- Chest X-ray shows:
- Deep sulcus sign on the left
- Depressed left hemidiaphragm – suggests tension pneumothorax
Follow-up
Post–chest tube insertion, the diaphragm returns to normal position (arrow(), confirming decompression.
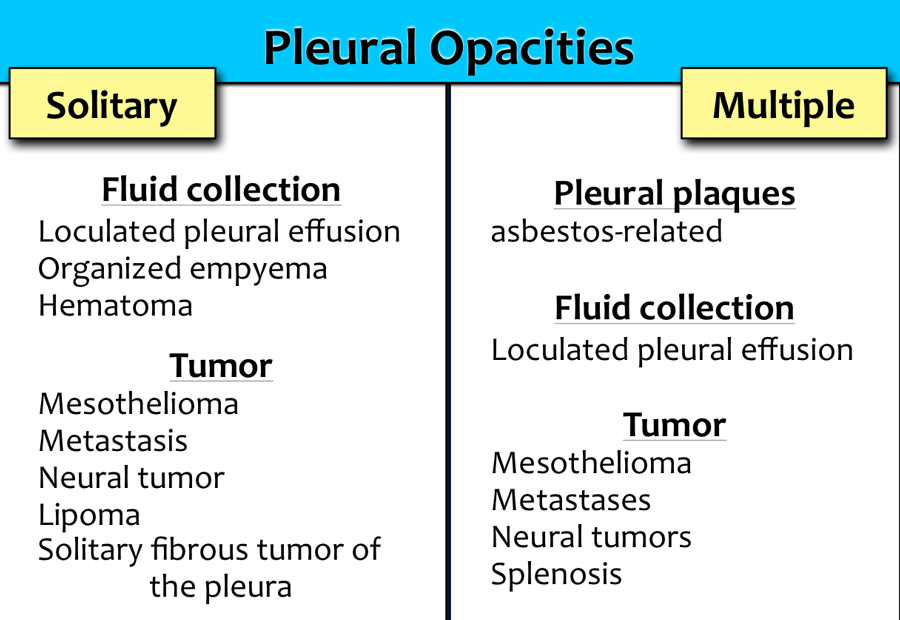
Pleural opacities
Common Causes
See reference table.
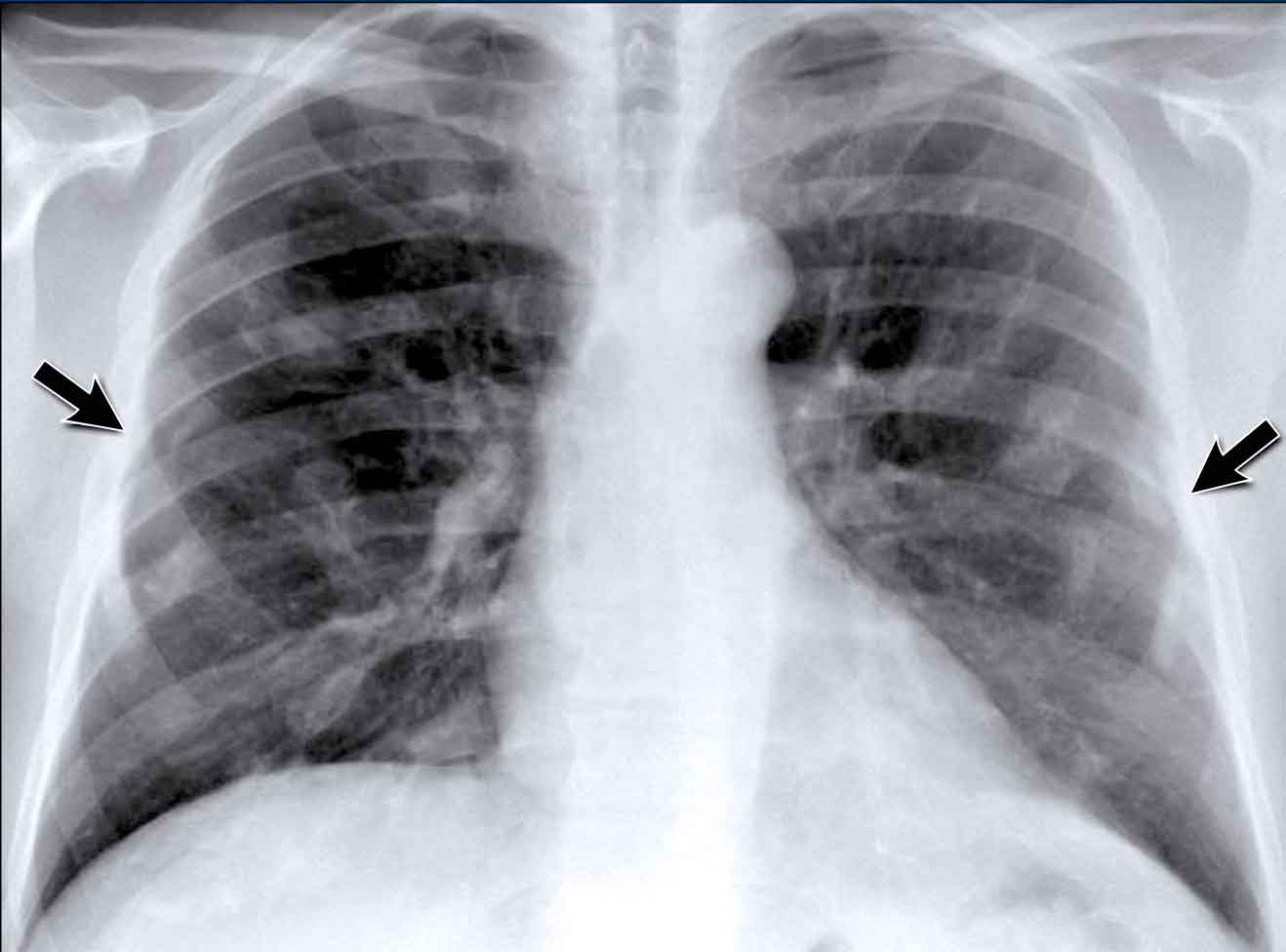
Pleural Plaques (Asbestos-Related)
- Multiple irregular pleural opacities are seen.
- Some follow the contours of the chest wall (arrows).
- Typical features of asbestos-related pleural plaques:
- Bilateral, extensive
- Often involve the diaphragmatic domes
Unilateral calcified pleural opacities may indicate:
- Tuberculosis (TB)
- Empyema
- Hemorrhagic effusion
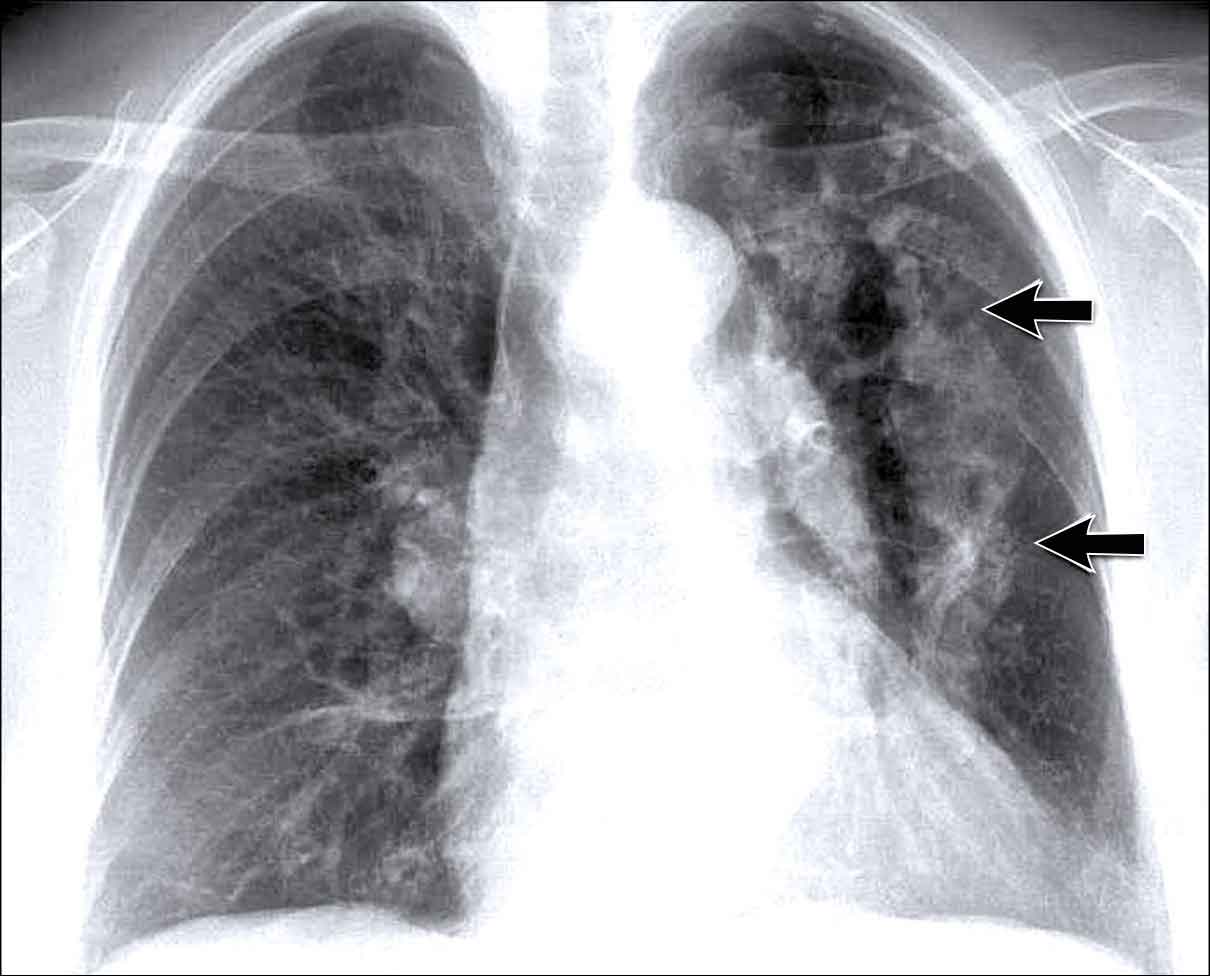
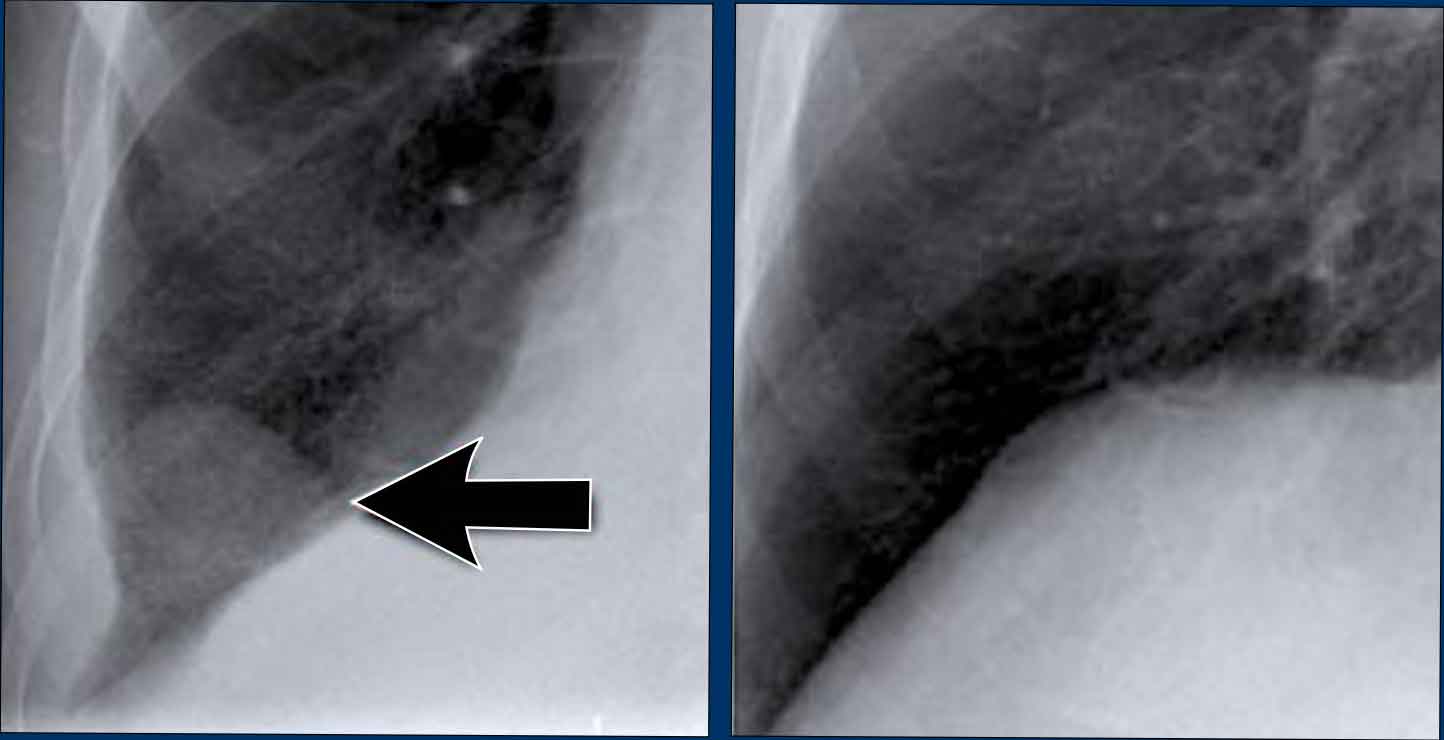
Pleural Hematoma
- Seen in a patient following chest trauma.
- Presented as a pleural opacity, presumed to be a hematoma (arrow).
- Resolved spontaneously on follow-up imaging.
Chest wall
Rib Fractures
The most commonly observed chest wall abnormalities on chest X-ray are healed rib fractures.
The radiograph demonstrates multiple rib deformities consistent with old fractures (arrows).
Rib Fractures mimicking a mass
- Healing fractures may show callus formation, which can mimic a pulmonary mass (blue arrow).
- In some cases, CT imaging is required to distinguish between a healing rib fracture and a true lung lesion.
Associated Findings
Increased lung volumes and prominent pulmonary arteries are noted, suggestive of pulmonary arterial hypertension, likely in the context of chronic obstructive pulmonary disease (COPD).
Bone Metastases
- The second most frequent chest wall abnormalities are osseous metastases involving the ribs and vertebral bodies.
- Example: An expansile lesion is noted in the posterior aspect of a right rib, compatible with metastatic disease.
Abdomen
Abdominal Free Air on Chest X-Ray
Pneumoperitoneum:
- The most striking finding on the chest X-ray is the presence of free intraperitoneal air beneath the diaphragm, indicative of bowel perforation.
- Differential includes postoperative pneumoperitoneum, which may persist for several days after abdominal surgery.
Incidental Thoracic Finding
- A subtle density is visible over the first rib in the left upper lobe, located in the so-called "hidden area".
- This was subsequently diagnosed as a primary lung carcinoma.
Another Example of Free Air
- A second patient presents with free subdiaphragmatic air.
- A thin, well-defined diaphragmatic contour is visible (arrow), differentiating it from plate-like atelectasis, which may mimic this appearance in cases of suboptimal inspiration.
Charity
All the profits of the Radiology Assistant go to Medical Action Myanmar which is run by Dr. Nini Tun and Dr. Frank Smithuis sr, who is a professor at Oxford university and happens to be the brother of Robin Smithuis.
Click here to watch the video of Medical Action Myanmar and if you like the Radiology Assistant, please support Medical Action Myanmar with a gift.