Mediastinal Masses - differential diagnosis
Sanjeev Bhalla, Marieke Hazewinkel and Robin Smithuis
Cardiothoracic Imaging Section of the Mallinckrodt Institute of Radiology, St. Louis, USA and the Radiology department the Medical Centre Alkmaar and the Rijnland Hospital, Leiderdorp, the Netherlands
Publicationdate
This review is based on a presentation given by Sanjeev Bhalla and was adapted for the Radiology Assistant by Marieke Hazewinkel and Robin Smithuis.
Sanjeev Bhalla is section chief of the Cardiothoracic Imaging Section of the Mallinckrodt Institute of Radiology.
This review will focus on how to narrow down the differential diagnosis of mediastinal lesions by localizing and characterizing them.
Introduction
Whenever you see a mass on a chest x-ray that is possibly located within the mediastinum, your goal is to determine the following:
- Is it a mediastinal mass?
- Is it in the anterior, middle or posterior mediastinum?
- Are you able to characterize the lesion by determining whether it has any fatty, fluid or vascular components?
The table on the left is the overall table for mediastinal masses.
In the next paragraphs we will discuss each compartment separately.
Statistically, it is important to remember the following:
- Most masses (> 60%) are:
- Thymomas
- Neurogenic Tumors
- Benign Cysts
- Lymphadenopathy (LAD)
- In children the most common (> 80%) are:
- Neurogenic tumors
- Germ cell tumors
- Foregut cysts
- In adults the most common are:
- Lymphomas
- LAD
- Thymomas
- Thyroid masses
Localize to the mediastinum
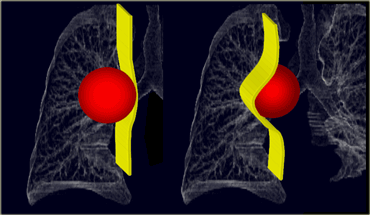 LEFT: A lung mass abutts the mediastinal surface and creates acute angles with the lung.RIGHT: A mediastinal mass will sit under the surface of the mediastinum, creating obtuse angles with the lung.
LEFT: A lung mass abutts the mediastinal surface and creates acute angles with the lung.RIGHT: A mediastinal mass will sit under the surface of the mediastinum, creating obtuse angles with the lung.
The following characteristics indicate that a lesion originates within the mediastinum:
- Unlike lung lesions, a mediastinal mass will not contain air bronchograms.
- The margins with the lung will be obtuse.
- Mediastinal lines (azygoesophageal recess, anterior and posterior junction lines) will be disrupted.
- There can be associated spinal, costal or sternal abnormalities.
A lung mass abutts the mediastinal surface and creates acute angles with the lung, while a mediastinal mass will sit under the surface creating obtuse angles with the lung (Figure).
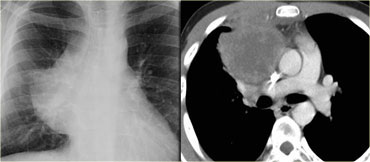
On the left you see two different patients.
Describe the findings and continue.
On the x-ray on the left there is a lesion that has an acute border with the mediastinum.
This must be a lung mass.
The chest radiograph on the right shows a lesion with an obtuse angle to the mediastinum.
This must be a mediastinal mass.
Since there is a silhouette-sign with the right heart border - which is located anteriorly - we can deduce that the mass must be located within the anterior mediastinum.
The lesion on the left was a pancoast tumor.
The lesion on the right was a thymoma, located within the anterior mediastinum.
Localize within the mediastinum
The mediastinum can be divided into anterior, middle and posterior compartments.
It is important to remember that there is no tissue plane separating these compartments.
On the lateral radiograph the anterior and middle compartments can be separated by drawing an imaginary line anterior to the trachea and posteriorly to the inferior vena cava.
The middle and posterior compartments can be separated by an imaginary line passing 1 cm posteriorly to the anterior border of the vertebral bodies.
This division allows us to make a more narrow differential diagnosis.
In many hospitals a CT will be made to further analyze and characterize anterior and middle mediastinal masses.
An MRI is usually made to analyze masses located in the posterior compartment because the majority of these masses turn out to be neurogenic in nature.
An additional CT can be performed, when bone needs to be assessed.
Anterior Mediastinum
The anterior mediastinum contains the following structures: thymus, lymph nodes, ascending aorta, pulmonary artery, phrenic nerves and thyroid.
The most common lesions that you will see in the anterior mediastinum will either be of thymic or lymph node origin.
Even the germ cell tumors arise from the pluripotent cells of the thymus.
Before you want to biopsy an anterior mediastinal mass, do not forget thta some of these lesions can be vascular in origin.
The four T's make up the mnemonic for anterior mediastinal masses::
- Thymus
- Teratoma (germ cell)
- Thyroid
- Terrible Lymphoma
On conventional radiographs look for the signs listed in the table on the left.
The finding of an obliterated retrosternal clear space is not so helpfull anymore, since nowadays many patients are obese.
In these patients the retrosternal space can be filled with fat.
Obliterated retrosternal clear space
Describe the images on the left.
Then continue.
On the PA film there is a lobulated widening of the superior mediastinum.
On the lateral chest film the retrosternal clear space is obliterated.
This happened to be a patient with lymphoma.
On the left FDG-PET images of the same patient.
There are multiple lymphatic masses in the anterior, middle and even posterior mediastinum, spreading to the neck.
Hilum Overlay Sign
When there is a mediastinal mass and you still can see the hilar vessels through this mass, then you know the mass does not arise from the hilum.
This is known as the hilum overlay sign.
Because of the geometry of the mediastinum most of these masses will be located in the anterior mediastinum.
Describe the images on the left.
Then continue.
On the chest film there is a mass that has obtuse angles with the mediastinum, so it is a mediastinal mass.
The hilar vessels are seen through this mass, so it does not arise from the hilum and probably will arise from the anterior mediastinum.
The anterior location was confirmed on a CT.
Most commonly this will be a mass of thymic or lymphatic origin.
This proved to be a lymphoma in a HIV-positive patient.
Cystic masses
The anterior mediastinum is an important location for cystic masses.
Masses can be entirely cystic (thymic cysts) or have solid components (lymphoma or cystic thymoma).
Some masses are cystic with enhancing septations - in these cases you should think of a germ cell tumor.
Describe the image on the left.
Then continue.
The CT shows an anterior mediastinal mass with water density attenuation.
This is typical for a thymic cyst.
Describe the image on the left.
Then continue.
The CT shows a mass located in the anterior mediastinum.
The mass is cystic but has solid enhancing septa.
This finding is very specific for a germ cell tumor.
Now many think that germ cell tumors contain fat and if a lesion does not contain fat, it cannot be a germ cell tumor.
You have to remember, that only about 60 % of germ cell tumors contain fat, so you must realize that the absence of fat does not exclude a germ cell tumor from the differential diagnosis.
The more solid components a germ cell tumor has, the more likely the tumor is to be malignant.
Describe the image on the left.
Then continue.
The CT shows a mass located in the anterior mediastinum.
The mass is cystic but has solid enhancing components, so we are worried about lymphoma, germ cell tumor and cystic thymoma.
This proved to be a cystic thymoma.
Middle Mediastinum
The middle mediastinum contains the following structures: lymph nodes, trachea, esophagus, azygos vein, vena cavae, posterior heart and the aortic arch.
The majority of middle mediastinal masses will consist of foregut duplication cysts (eg oesophageal duplication or bronchogenic cysts) or lymphadenopathy.
Aortic arch anomalies can also present as middle mediastinal masses.
Fluid containing lesions are usually duplication cysts or necrotic lymph nodes.
A pancreatic fluid collection due to pancreatitis may also present as a mediastinal mass.
A fibrovascular esophageal polyp is a mesenchymal lesion which almost always contains fat.
Vascular lesions are arch anomalies, azygos continuation due to interrupted inferior vena cava or hyperenhancing lymph nodes.
On conventional radiographs look for the signs listed in the table on the left.
Displaced azygoesophageal recess wiil be seen on the right.
On the left you may have a pseudoparavertebral line.
This is a new interface that looks like a paravertebral line.
Describe the image on the left.
Then continue.
On the AP chest radiograph of this patient there is widening of the azygoesophageal recess on the right.
There is an apparent widening of the paravertebral line on the left.
On the lateral film the mass is anterior to the spine and therefore is located in the middle mediastinal.
On the CT the azygoesophageal recess is displaced to the right due to oesophageal varices (blue arrow) and there is also a new interface on the left.
This is a patient with cirrhosis of the liver and varices as a result of portal hypertension.
On the left a patient with a small cell lung carcinoma.
Describe the images on the left.
Then continue.
On the PA film there is a lobulated paratracheal stripe on the right.
On the lateral radiograph there is a density overlying the ascending aorta and filling the retrosternal space.
These findings indicate a mass in the anterior aswell as in the middle mediastinum.
The CT confirms the presence oof lymphomas in both the anterior and the middle mediastinum.
On the left two different patients.
One of these patients has pulmonary hypertension and the other has sarcoidosis.
Describe the images on the left.
Then continue.
On the right image there is a lobulated mass surrounding the right bronchus creating a 'doughnut' with the bronchus as the hole in the doughnut.
On the left image there is only density in the area from 9 o'clock to 3 o'clock and not in the 3 - 9 o'clock area.
So the patient on the left has pulmonary hypertension with moderately enlarged vessels while the patient on the right has sarcoidosis with widespread lymphadenopathy.
When there is a density in the 3 - 9 o'clock area, there should always be concern about mediastinal masses.
Posterior Mediastinum
The posterior mediastinum contains the following structures: sympathetic ganglia, nerve roots, lymph nodes, parasympathetic chain, thoracic duct, descending thoracic aorta, small vessels and the vertebrae.
Most masses in the posterior mediastinum are neurogenic in nature.
These can arise from the sympathetic ganglia (eg neuroblastoma) or from the nerve roots (eg schwannoma or neurofibroma).
Don't forget lymphadenopathy, the vertebrae and the descending thoracic aorta as potential causes for posterior mediastinal masses.
Cystic lesions will be either neuroenteric cysts, schwannomas or meningoceles.
Fat containing lesions will be extramedullary hematopoiesis.
When the anemia is resolved the extramedullary marrow will stop producing blood and become fatty.
On conventional radiographs look for:
- Cervicothoracic Sign
- Widening of the paravertebral stripes
Cervicothoracic sign
The anterior mediastinum stops at the level of the superior clavicle.
Therefore, if the cranial border of a lesion is obscured at or below the level of the clavicles, it is located in the anterior mediastinum.
A lesion clearly visible above the clavicles must lie posteriorly and thus located within the posterior mediastinum.
Example:
The lateral and superior borders of this mediastinal lesion are clearly visible meaning that the lesion is bordered by lung tissue. The lesion extends above the clavicle and therefore is located in the posterior mediastinum.
On the left the MR of the same patient.
It turned out to be a schwannoma.
On the left images of a patient, who has a disease, that is the most commonly missed diagnosis in the emergency department resulting in the number one cause of law suits.
Study the images and then continue.
Notice the widening of the paravertebral stripes on both the left and the right on the PA radiograph.
On the lateral radiograph there is a severely narrowed disc space.
The diagnosis is discitis.
On MR you will notice the edema of the soft tissues and the high signal intensity of the disc.
More than one compartment
Since there are no tissue planes separating the mediastinal compartments, there are lesions that do not respect our approach to the mediastinum.
These lesions tend to occupy more than one compartment and include: mediastinitis, hematomas, vascular entities, bronchogenic cancer, metastases and lymphangiomas (fluid containing).
Characterize
Once you have localized a mediastinal mass, next try to charcterize it by assessing whether it has any of the following characteristics:
- Does the mass contain fluid?
- Does it contain fat?/li>
- Does it enhance following the administration of intravenous contrast?
Fluid containing masses
This is a list of mediastinal msses that may contain fluid:
- Thymic Cyst
- Thymoma
- Teratoma
- Pericardial Cyst
- Foregut Duplication
- Meningocoele
- Neuroenteric Cyst
- Cystic Lymphadenopathy
- Lymphangioma
If a mass contains fluid it could be a teratoma (on the left) or a thymic cyst (on the right).
Note that this teratoma does not contain fat.
Teratomas are the most common benign germ cell tumors.
The most common malignant germ cell tumor is the seminoma.
Describe the image on the left.
Then continue.
There is are multiple masses in both the anterior and middle mediastinum.
The attenuation values are of water density.
These findings favor the diagnosis of cystic lymphadenopathy in a patient with metastatic disease.
Describe the image on the left.
Then continue.
There is a cystic lesion in the middle mediastinum.
There is a fluid fluid level with milk of calcium.
Foregut duplication cysts occasionally contain milk of calcium like in this example of an esophageal duplication cyst.
Fat containing masses
The differential diagnosis of fat containing mediastinal masses is:
- Thymolipoma
- Teratoma (Germ cell tumors)
- Esophageal lipoma
- Fat deposition
- Lipoma
- Lipoblastoma
- Liposarcoma
- Extramedullary hematopoiesis
On the left we see an fat-containing anterior mediastinal mass.
This is the typical finding of a fat-containing teratoma.
Describe the image on the left.
Then continue.
The axial CT and sagittal MR demonstrate a lipomatous lesion within the lumen of the esophagus.
This is typical for a esophageal lipoma and its fibrovascular stalk.
Enhancing masses
The differential diagnosis of enhancing mediastinal masses is:
- Hyperenhancing lymph nodes
- Thyroid tissue
- Paragangliomas
- Hemangiomas
- Vascular Etiologies
On the left multiple enhancing lesions.
This is typical for hyperenhancing lymph nodes.
Enhancing lymphomas can be seen in:
- Melanoma
- Renal cell carcinoma
- Thyroid carcinoma
- Castlemann's disease (as in this case)
Describe the image.
Then continue.
First notice the large thymus in this young child.
There is also an enhancing mass in the posterior mediastinum extending into the vertebral canal.
This is typical for a hemangioma.
Describe the image.
Then continue.
Somewhat irregular enhancing mass in the anterior mediastinum.
This proved to be a thyroid mass.
Charity
All the profits of the Radiology Assistant go to Medical Action Myanmar which is run by Dr. Nini Tun and Dr. Frank Smithuis sr, who is a professor at Oxford university and happens to be the brother of Robin Smithuis.
Click here to watch the video of Medical Action Myanmar and if you like the Radiology Assistant, please support Medical Action Myanmar with a small gift.