Bi-RADS for Mammography and Ultrasound 2013
Updated version
Harmien Zonderland and Robin Smithuis
Radiology department of the Academical Medical Centre in Amsterdam and the Rijnland hospital in Leiderdorp, the Netherlands
Publicationdate
This article provides a summary of the BI-RADS® Atlas, 5th Edition (2013) for mammography and breast ultrasound.
It is an updated version of the 2005 article.
Since 2000, the use of BI-RADS has been mandatory in the Netherlands, as described in the updated Breast Cancer Guideline (2012) (6).
The implementation of BI-RADS is an integral part of the national quality assurance program for breast imaging.
We encourage all professionals involved in breast imaging to consult the illustrated BI-RADS Atlas, 5th Edition (2013)for comprehensive understanding and correct application of the system.
Introduction
The ACR BI-RADS Atlas 2013 (4) is the updated version of the 2003 Atlas.
BI-RADS® is designed to standardize breast imaging reporting and to reduce confusion in breast imaging interpretations.
It also facilitates outcome monitoring and quality assessment.
It contains a lexicon for standardized terminology (descriptors) for mammography, breast US and MRI, as well as chapters on Report Organization and Guidance Chapters for use in daily practice.
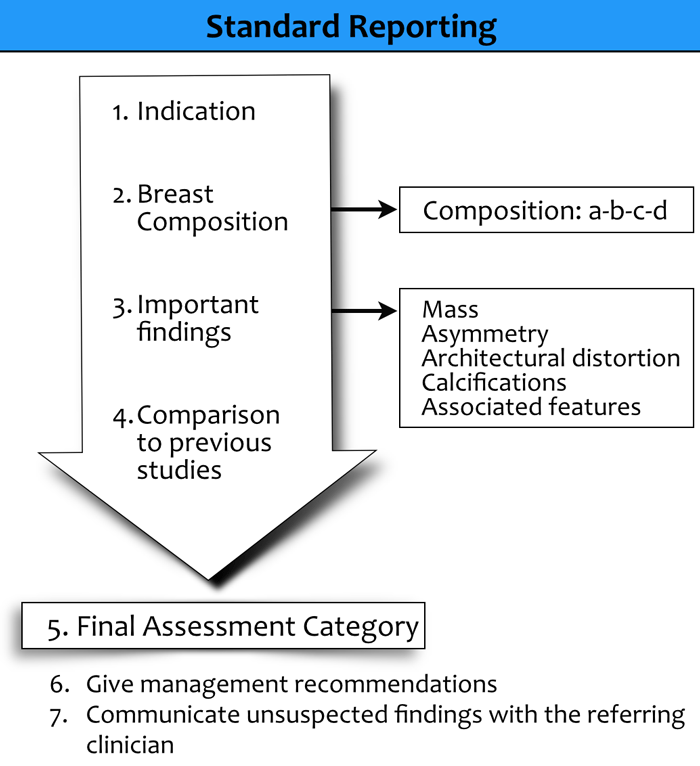
Standardized Reporting
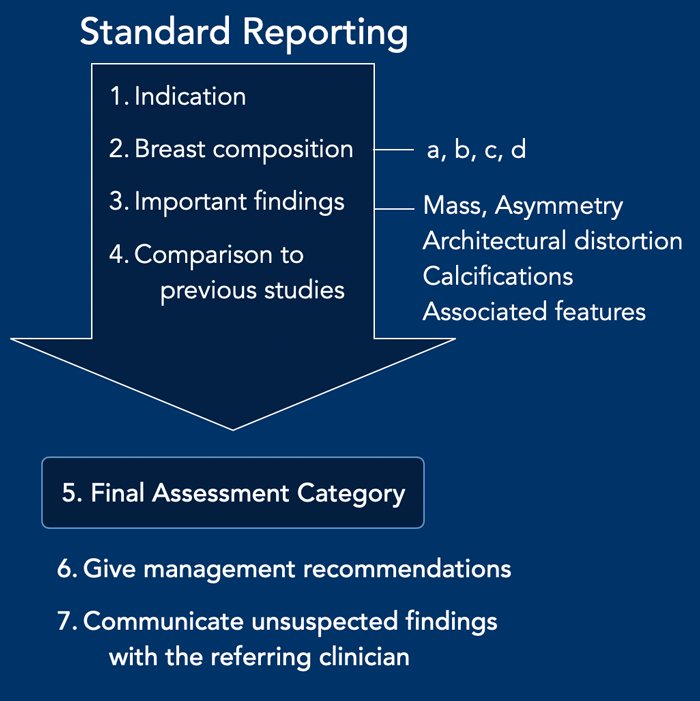
When reporting a breast imaging study, the following elements should be included:
- Indication for the study:
Specify whether the examination is screening, diagnostic, or follow-up.
Patient history: Include relevant clinical information. If an ultrasound is performed, specify whether it is targeted (focused on a specific area of concern) or performed as supplementary screening. - Breast composition:
Describe the breast density according to the BI-RADS categories. - Description of findings:
Use standardized terminology to describe all significant findings.
Morphologic descriptors include:- Mass
- Asymmetry
- Architectural distortion
- Calcifications
Correlate imaging findings with clinical information and results from mammography, ultrasound, and/or MRI.
Integrate mammographic and sonographic findings into a single, unified report. - Comparison with prior studies:
Compare with previous imaging when available.
Awaiting prior studies for comparison should only delay reporting if necessary for a definitive assessment. - Final assessment category:
Assign a BI-RADS category (0–6) and include the corresponding standardized phrase.
When both mammography and ultrasound are performed, the overall assessment should reflect the most suspicious finding—that is, the finding with the highest likelihood of malignancy. - Management recommendations:
Provide clear recommendations for further management or follow-up. - Communication of unexpected findings:
Any unexpected or clinically significant findings should be communicated promptly to the referring clinician.
Verbal discussions between the radiologist, patient, or referring clinician should be documented in the report.
Mammography and Ultrasound Lexicon
The table shows a summary of the mammography and ultrasound lexicon.
Enlarge the table by clicking on the image.
First describe the breast composition.
When there is a significant finding use the descriptors in the table.
The ultrasound lexicon has many similarities to the mammography lexicon, but there are some descriptors that are specific for ultrasound.
We will discuss the lexicon in more detail in a moment.
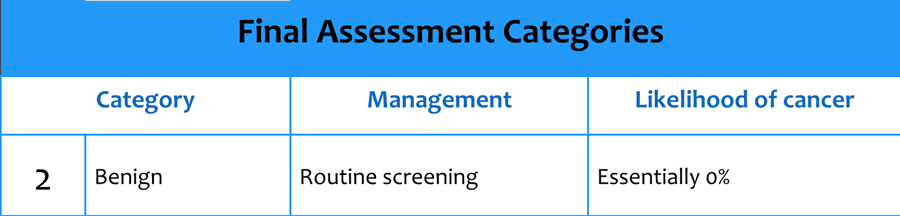
BI-RADS Assessment Categories
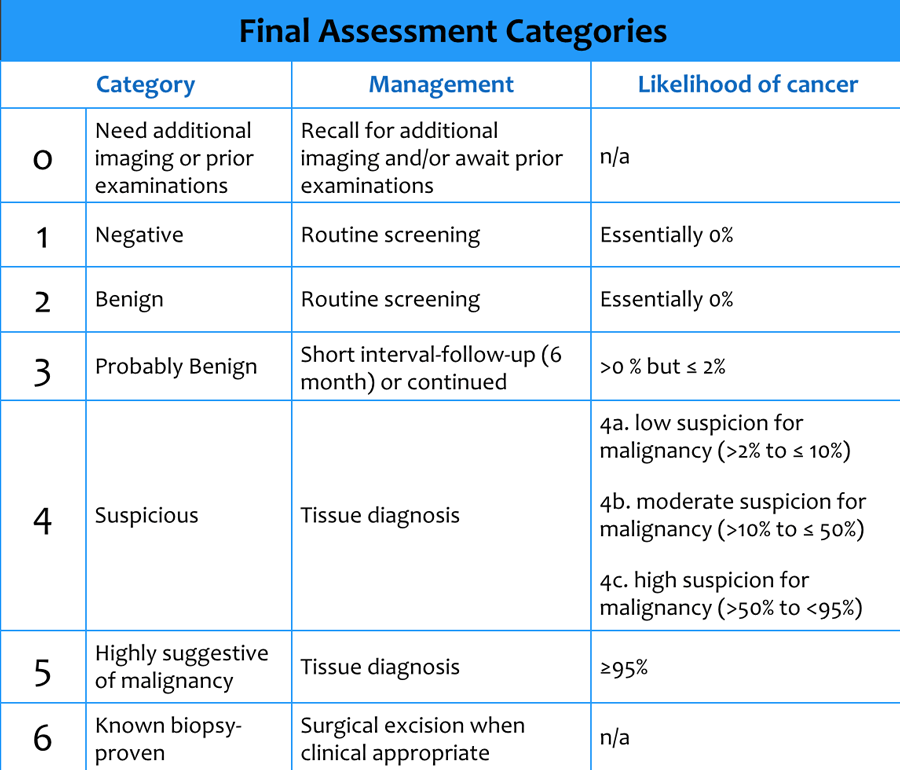
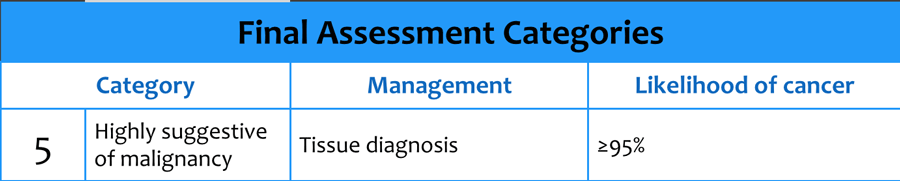
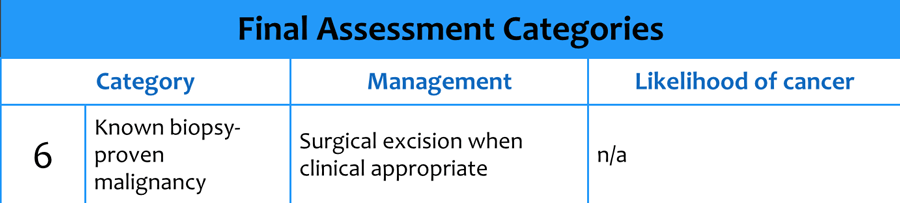
The table shows the final assessment categories.
We will first discuss the breast imaging lexicon of mammography and ultrasound and then discuss in more detail the final assessment categories and the do's and don'ts in these categories.
Click image to enlarge.
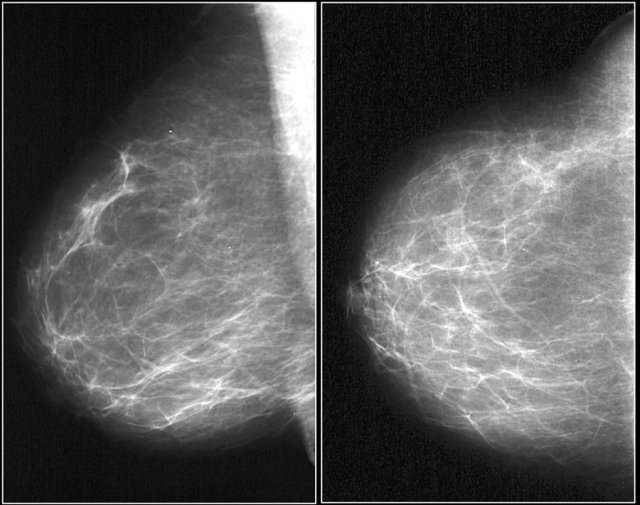
Study the images.
If you find any abnormality, make a decription and assessment category.
Mammography - Breast Imaging Lexicon
Breast Composition
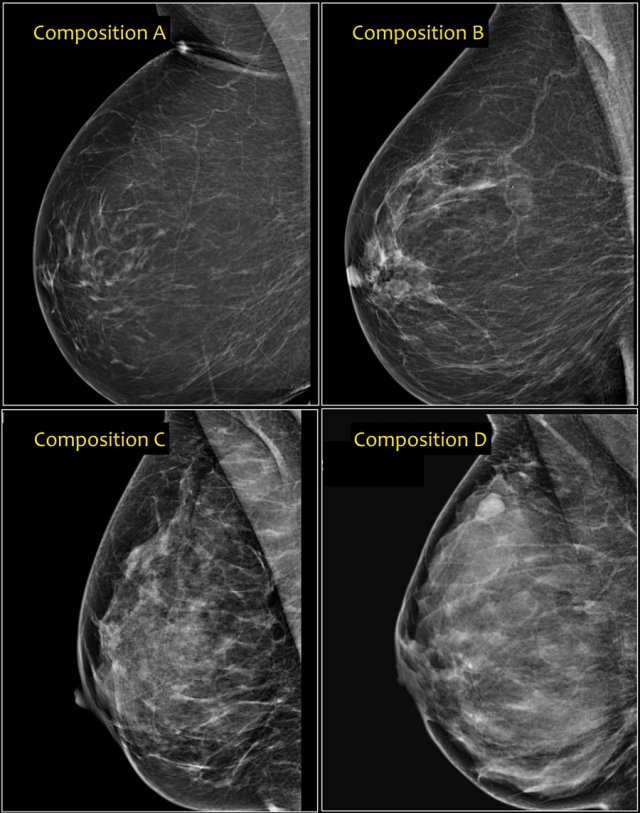
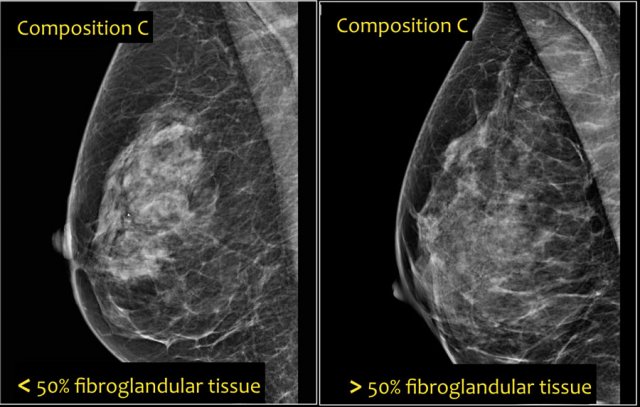
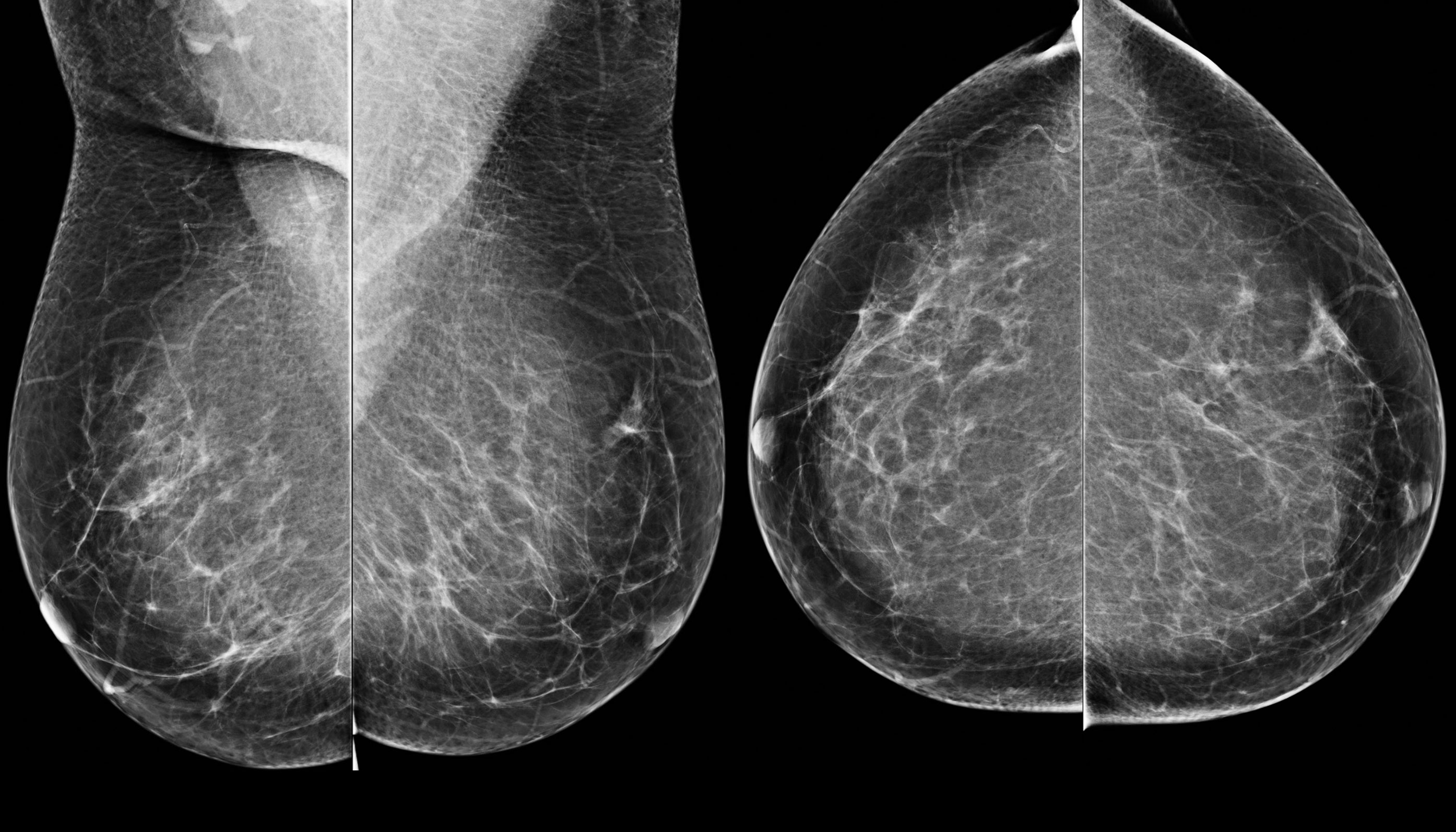
In the BI-RADS edition 2003 the assignment of the breast composition was based on the overall density resulting in ACR catergory 1 ( <25% fibroglandular tissue), category 2 ( 25-50%), category 3 (50-75%) and category 4 (>75%).
In BI-RADS 2013 the use of percentages is discouraged, because in individual cases it is more important to take into account the chance that a mass can be obscured by fibroglandular tissue than the percentage of breast density as an indicator for breast cancer risk.
In the BI-RADS edition 2013 the assignment of the breast composition is changed into a, b, c and d-categories followed by a description:
- a- The breast are almost entirely fatty.
Mammography is highly sensitive in this setting. - b- There are scattered areas of fibroglandular density.
The term density describes the degree of x-ray attenuation of breast tissue but not discrete mammographic findings. - c- The breasts are heterogeneously dense, which may obscure small masses.
Some areas in the breasts are sufficiently dense to obscure small masses. - d - The breasts are extremely dense, which lowers the sensitivity of mammography.
Notice in the left example the composition is c - heterogeneously dense, although the volume of fibroglandular tissue is less than 50%.
The fibroglandular tissue in the upper part is sufficiently dense to obscure small masses.
So it is called c, because small masses can be obscured.
Historically this would have been called an ACR 2: 25-50% density.
The example on the right has more than 50% glandular tissue and is also called composition c.
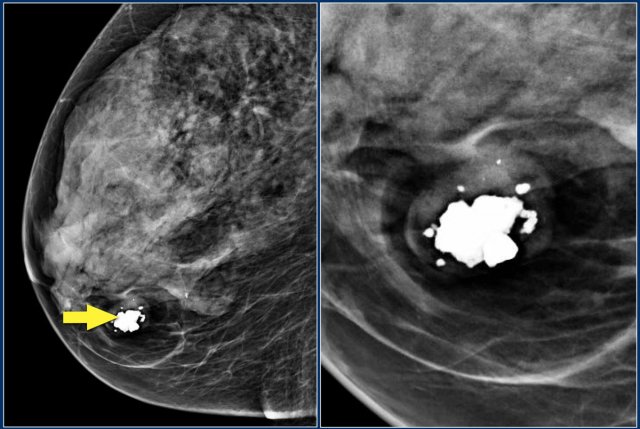
Mass
A 'Mass' is a space occupying 3D lesion seen in two different projections.
If a potential mass is seen in only a single projection it should be called a 'asymmetry' until its three-dimensionality is confirmed.
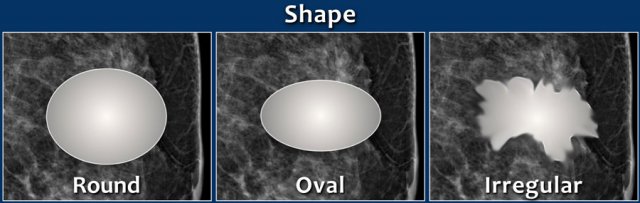
- Shape: oval (may include 2 or 3 lobulations), round or irregular
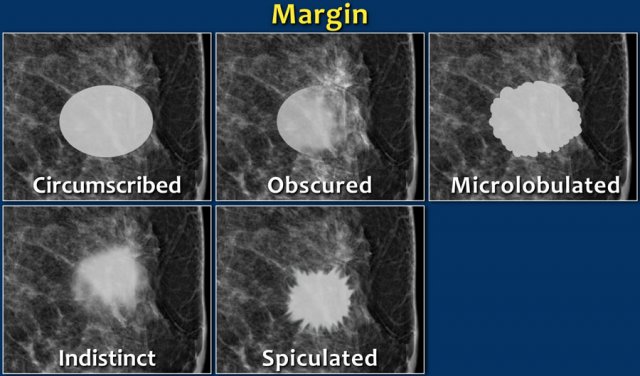
- Margins: circumscribed, obscured, microlobulated, indistinct, spiculated
- Density: high, equal, low or fat-containing.
The images show a fat-containing lesion with a popcorn-like calcification.
All fat-containing lesions are typically benign.
These image-findings are diagnostic for a hamartoma - also known as fibroadenolipoma.
The shape of a mass is either round, oval or irregular.
Always make sure that a mass that is found on physical examination is the same as the mass that is found with mammography or ultrasound.
Location and size should be applied in any lesion, that must undergo biopsy.
The margin of a lesion can be:
- Circumscribed (historically well-defined).
This is a benign finding. - Obscured or partially obscured, when the margin is hidden by superimposed fibroglandular tissue. Ultrasound can be helpful to define the margin better.
- Microlobulated. This implies a suspicious finding.
- Indistinct (historically ill-defined).
This is also a suspicious finding. - Spiculated with radiating lines from the mass is a very suspicious finding.
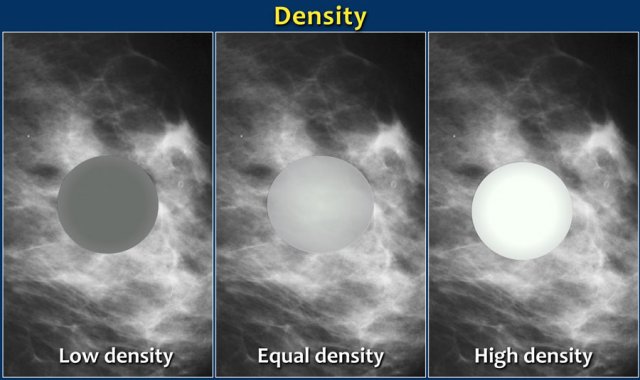
The density of a mass is related to the expected attenuation of an equal volume of fibroglandular tissue.
High density is associated with malignancy.
It is extremely rare for breast cancer to be low density.
Here multiple round circumscribed low density masses in the right breast.
These were the result of lipofilling, which is transplantation of body fat to the breast.
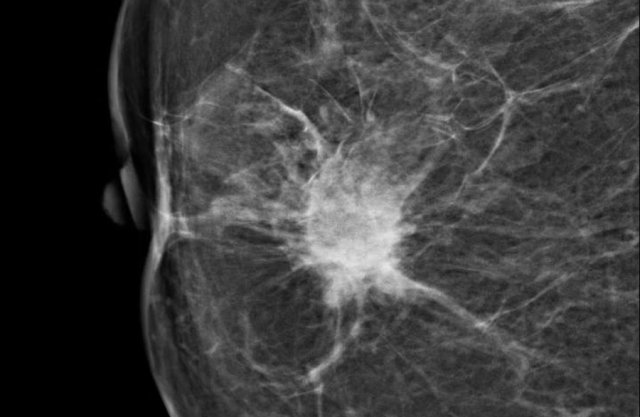
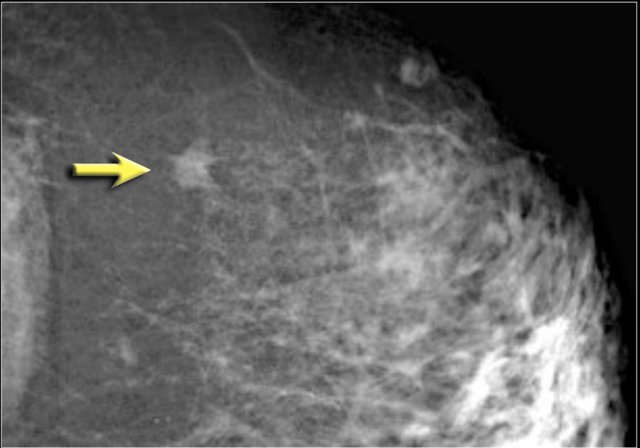
Here a hyperdense mass with an irregular shape and a spiculated margin.
Notice the focal skin retraction.
This was reported as BI-RADS 5 and proved to be an invasive ductal carcinoma.
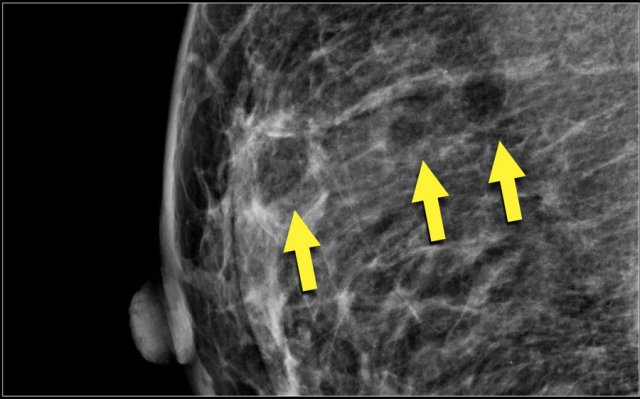
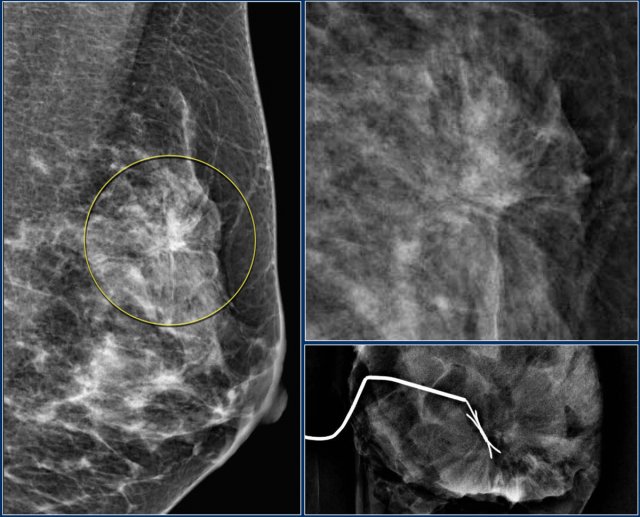
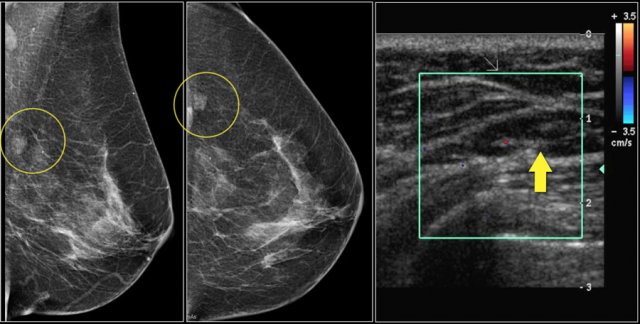
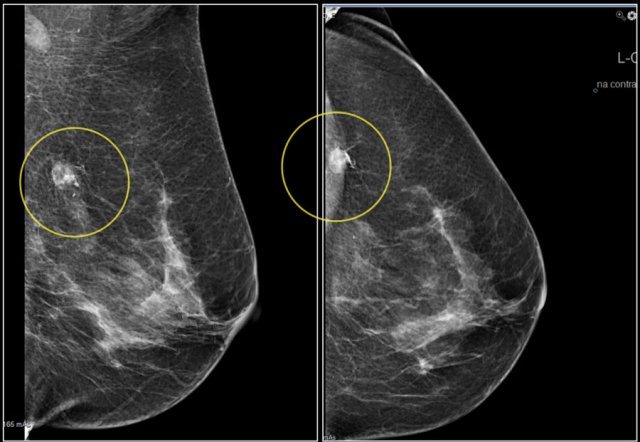
Architectural distortion
The term architectural distortion is used, when the normal architecture is distorted with no definite mass visible.
This includes thin straight lines or spiculations radiating from a point, and focal retraction, distortion or straightening at the edges of the parenchyma.
The differential diagnosis is scar tissue or carcinoma.
Architectural distortion can also be seen as an associated feature.
For instance if there is a mass that causes architectural distortion, the likelihood of malignancy is greater than in the case of a mass without distortion.
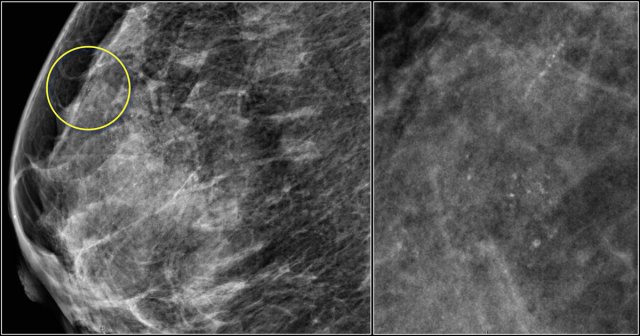
Notice the distortion of the normal breast architecture on oblique view (yellow circle) and magnification view.
A resection was performed and only scar tissue was found in the specimen.
Asymmetries
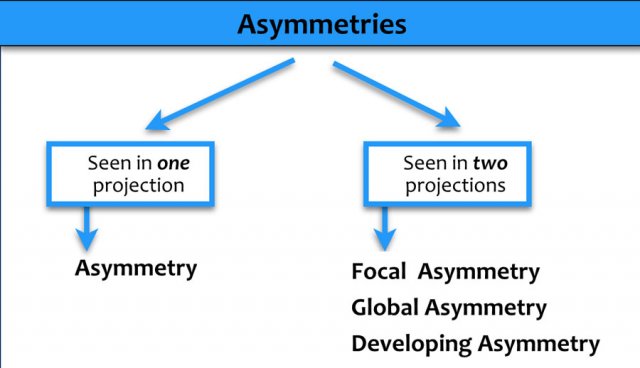
Definition
Asymmetries are findings that represent unilateral deposits of tissue that do not meet the definition of a mass.
Types
- Asymmetry in a single projection: Usually caused by superimposition of normal tissue.
- Focal asymmetry: Visible on two projections; a real finding that must be differentiated from a mass.
- Global asymmetry: Involves at least one-quarter of the breast and is usually a normal variant.
- Developing asymmetry: A new, larger, or more conspicuous asymmetry compared with prior examinations.
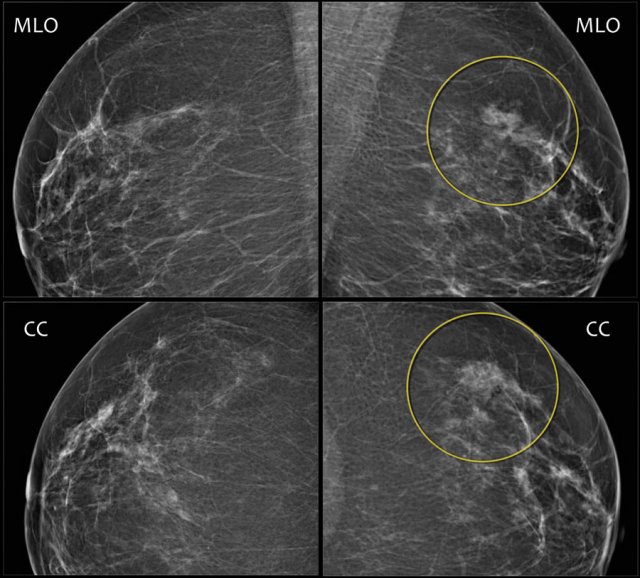
Here an example of a focal asymmetry seen on MLO and CC-view.
Local compression views and ultrasound did not show any mass.
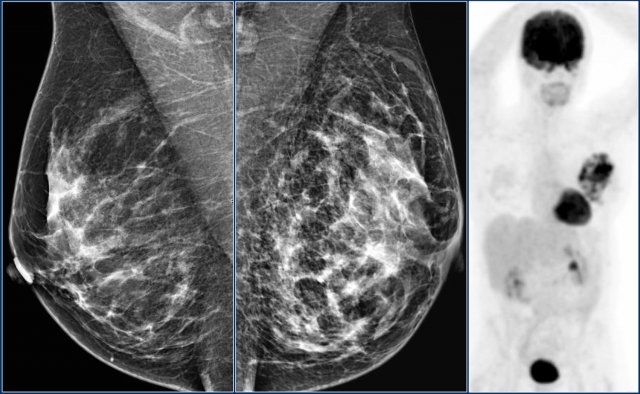
Here an example of global asymmetry.
In this patient this is not a normal variant, since there are associated features, that indicate the possibility of malignancy like skin thickening, thickened septa and subtle nipple retraction.
Ultrasound (not shown) detected multiple small masses that proved to be adenocarcinoma.
The PET-CT shows diffuse infiltrating carcinoma.
Asymmetry versus Mass
All types of asymmmetry have different border contours than true masses and also lack the conspicuity of masses.
Asymmetries appear similar to other discrete areas of fibroglandulair tissue except that they are unitaleral, with no mirror-image correlate in the opposite breast.
An asymmetry demonstrates concave outward borders and usually is interspersed with fat, whereas a mass demonstrates convex outward borders and appears denser in the center than at the periphery.
The use of the term "density" is confusing, as the term "density" should only be used to describe the x-ray attenuation of a mass compared to an equal volume of fibroglandular tissue.
Calcifications
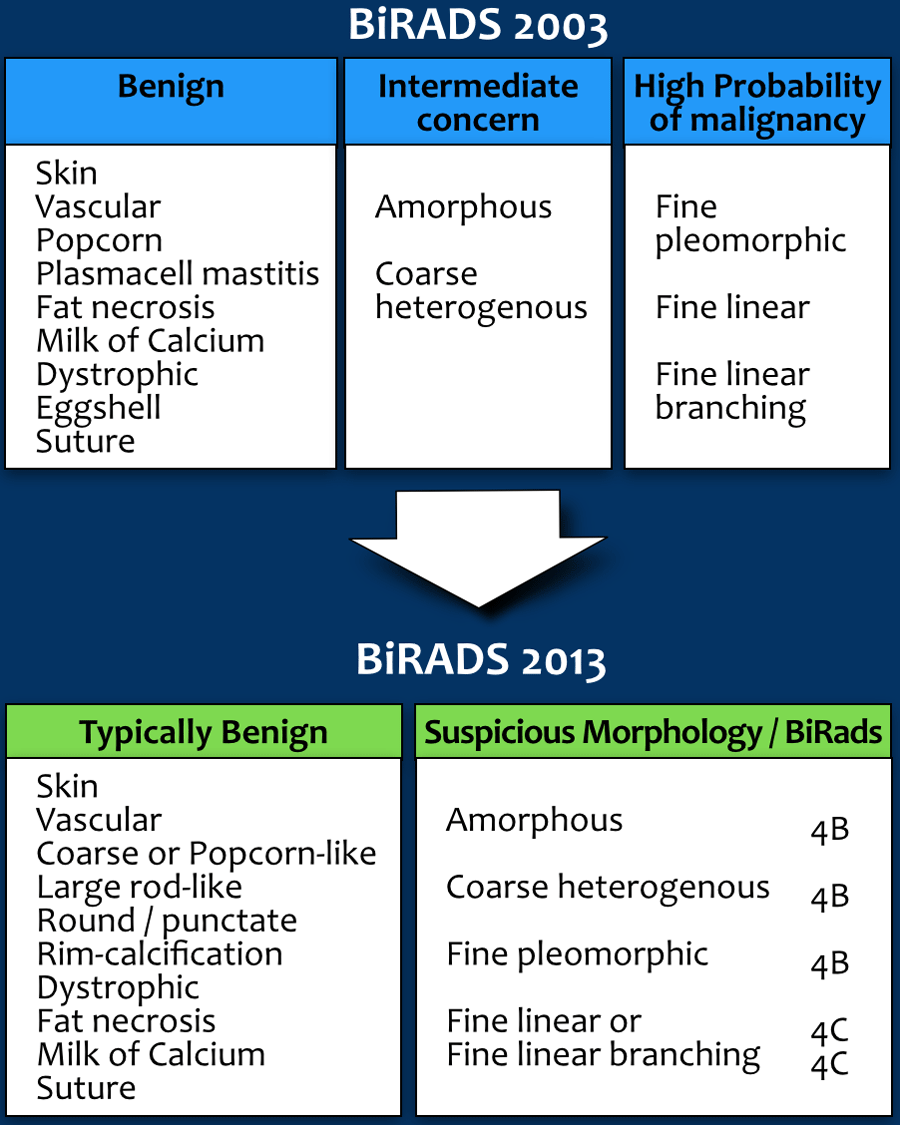
In the 2003 atlas calcifications were classified by morphology and distribution either as benign, intermediate concern or high probability of malignancy.
In the 2013 version the approach has changed.
Since calcifications of intermediate concern and of high probability of malignancy all are being treated the same way, which usually means biopsy, it is logic to group them together.
Calcifications are now either typically benign or of suspicious morphology.
Within this last group the chances of malignancy are different depending on their morphology (BI-RADS 4B or 4C) and also depending on their distribution.
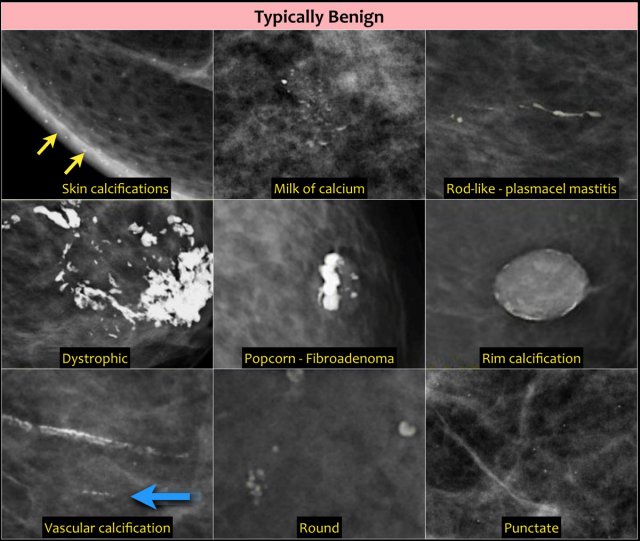
Typically benign
Skin, vascular, coarse, large rodlike, round or punctate (< 1mm), rim, dystrophic, milk of calcium and suture calcifications are typically benign.
There is one exception of the rule: an isolated group of punctuate calcifications that is new, increasing, linear, or segmental in distribution, or adjacent to a known cancer can be assigned as probably benign or suspicious.
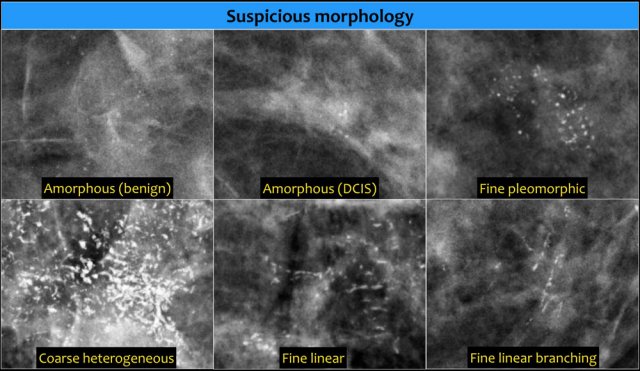
Suspicious morphology
- Amorphous (BI-RADS 4B)
So small and/or hazy in appearance that a more specific particle shape cannot be determined. - Coarse heterogeneous (BI-RADS 4B)
Irregular, conspicuous calcifications that are generally between 0,5 mm and 1 mm and tend to coalesce but are smaller than dystrophic calcifications. - Fine pleomorphic (BI-RADS 4B)
Usually more conspicuous than amorphous forms and are seen to have discrete shapes, without fine linear and linear branching forms, usually < 0,5 mm. - Fine linear or fine-linear branching (BI-RADS 4C)
Thin, linear irregular calcifications, may be discontinuous, occasionally branching forms can be seen, usually < 0,5 mm.
Read more on breast calcifications.
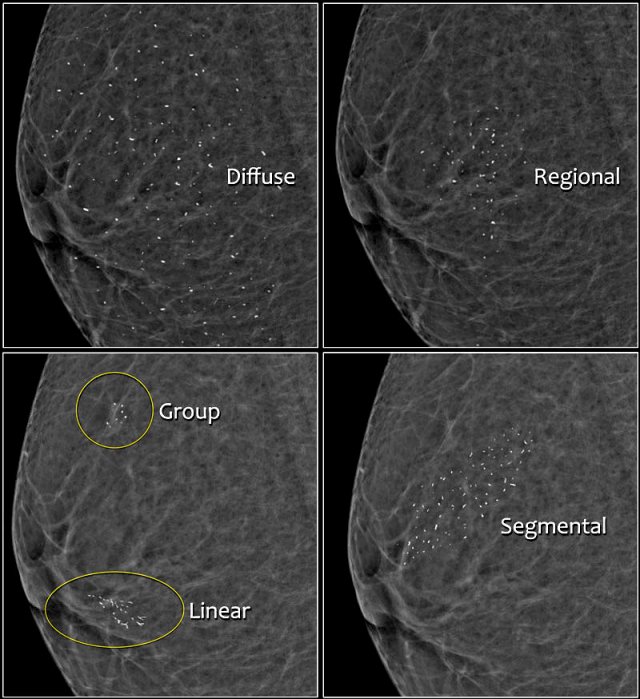
Distribution of calcifications
The arrangement of calcifications, the distribution, is at least as important as morphology.
These descriptors are arranged according to the risk of malignancy:
- Diffuse: distributed randomly throughout the breast.
- Regional: occupying a large portion of breast tissue > 2 cm greatest dimension
- Grouped (historically cluster): few calcifications occupying a small portion of breast tissue: lower limit 5 calcifications within 1 cm and upper limit a larger number of calcifications within 2 cm.
- Linear: arranged in a line, which suggests deposits in a duct.
- Segmental: suggests deposits in a duct or ducts and their branches.
The 2013 edition refines the upper limit in size for grouped distribution as 2 cm (historically 1 cm) while retaining > 2 cm as the lower limit for regional distribution.
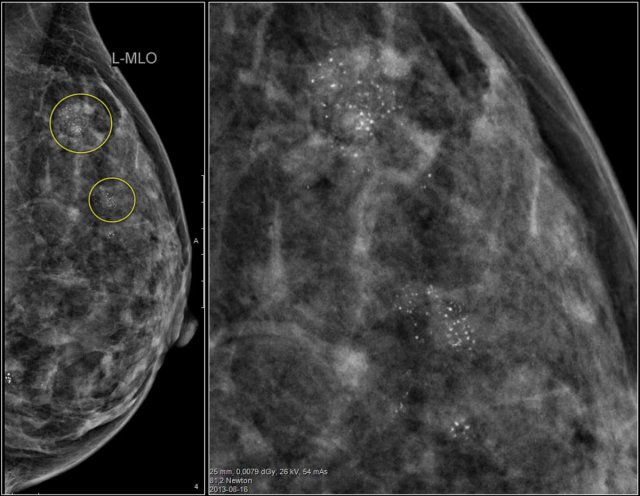
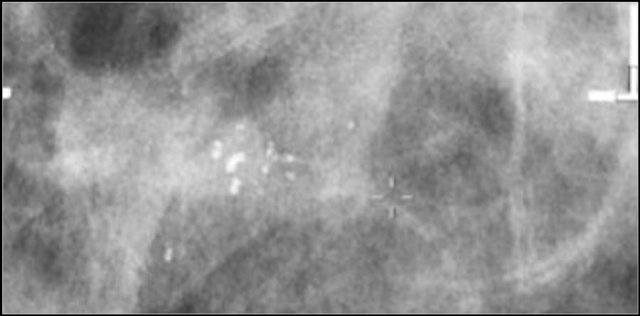
Study the images and describe the calcifications.
Then continue reading.
The findings are:
- Morphology: some are coarse heterogenous and some look more like fine pleomorphic.
- Distribution: Some calcifications are in a group ( <2cm) and some are in a regional distribution ( >2cm), but not in a segmental or linear arrangement.
This proved to be multifocal DCIS with areas of invasive carcinoma.
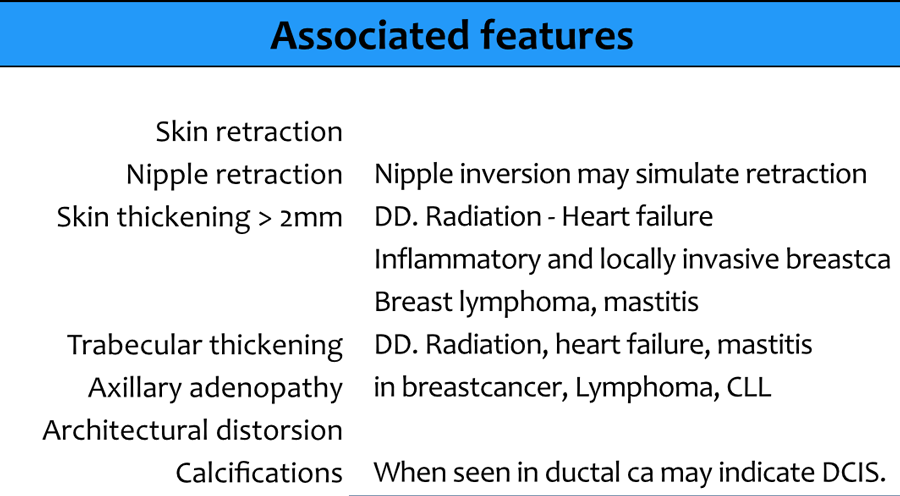
Associated features
Associated features are things that are seen in association with suspicious findings like masses, asymmetries and calcifications.
Associated features play a role in the final assessment.
For instance a BI-RADS 4-mass could get a BI-RADS 5 assessment if seen in association with skin retraction.
Special cases
Special cases are findings with features so typical that you do not need to describe them in detail, like for instance an intramammary lymph node or a wart on the skin.
Ultrasound - Breast Imaging Lexicon
Many descriptors for ultrasound are the same as for mammography.
For instance when we describe the shape or margin of a mass.
Here we will focus on findings that are specific for ultrasound:
Breast Composition:
- Homogeneous echotexture-fat
- Homogeneous echotexture-fibroglandular
- Heterogeneous echotexture
Mass:
- Orientation: unique to US-imaging, and defined as parallel (benign) or not parallel (suspicious finding) to the skin.
- Echo pattern: anechoic, hypoechoic, complex cystic and solid, isoechoic, hyperechoic, heterogeneous.
Echogenicity can contribute to the assessment of a lesion, together with other feature categories. Alone it has little specificity. - Posterior features: enhancement, shadowing.
Posterior features represent the attenuation characteristics of a mass with respect to its acoustic transmission, also of additional value. Alone it has little specificity.
Calcifications:
- On US poorly characterized compared with mammography, but can be recognized as echogenic foci, particularly when in a mass.
Associated features:
- Architectural distortion
- Duct changes
- Skin changes
- Edema
- Vascularity
- Elasticity assessment
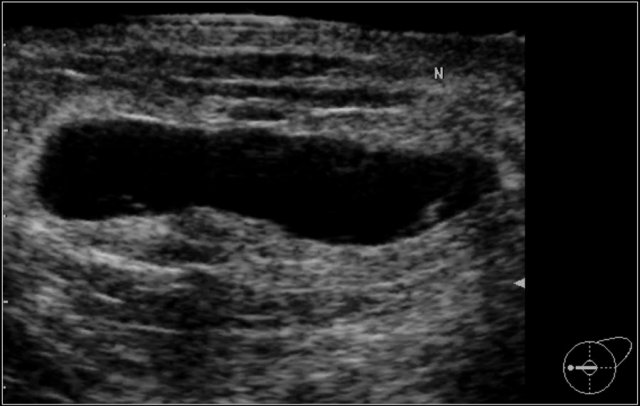
Special cases - cases with a unique diagnosis or pathognomonic ultrasound appearance:
- Simple cyst
- Complicated cyst
- Clustered microcysts
- Mass in or on skin
- Foreign body including implants
- Lympnodes- intramammary
- Lymph nodes- axillary
- Vascular abnormalities
- Postsurgical fluid collection
- Fat necrosis
Final Assessment Categories
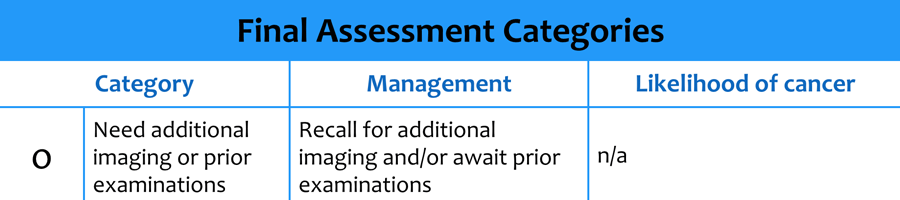
BI-RADS 0
Need Additional Imaging Evaluation and/or Prior Mammograms For Comparison:
Category 0 or BI-RADS 0 is utilized when further imaging evaluation (e.g. additional views or ultrasound) or retrieval of prior examinations is required.
When additional imaging studies are completed, a final assessment is made.
Always try to avoid this category by immediately doing additional imaging or retrieving old films before reporting.
Even better to have the old examinations before starting the examination.
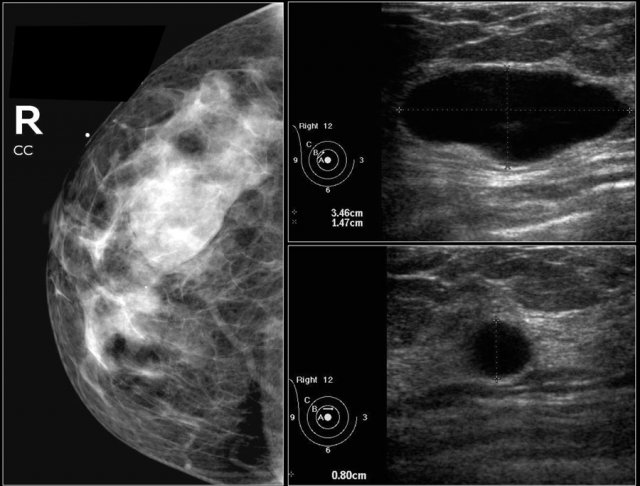
This patient presented with a mass on the mammogram at screening, which was assigned as BI-RADS 0 (needs additional imaging evaluation).
Additional ultrasound demonstrated that the mass was caused by an intramammary lymph node.
The final assessment is BI-RADS 2 (benign finding).
Don't forget to mention in the report that the lymph node on US corresponds with the noncalcified mass on mammography.
In the paragraph on location we will discuss how we can be sure that the lymph node that we found with ultrasound is indeed the same as the mammographic mass.
DO
- Use if additional mammographic imaging is needed: additional mammographic views, spot compression
- Use if additional US or (complete) mammography is needed ONLY if equipment or personnel is not available or patient is unable to wait
- Use if prior mammography or US are required to make a final assessment and issue an addendum including a revised assessment
DON'T
- Don't use if prior mammography or US are not available, however NOT required to make a final assessment.
- Don't use if prior mammography or US are irrelevant, because the finding is already suspicious.
- Don't use for findings that warrant further evaluation with MRI, but make a report before the MRI is performed.
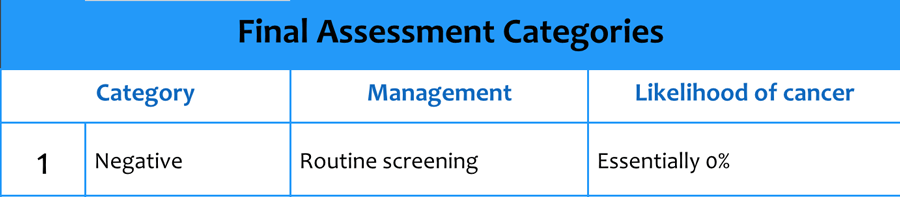
BI-RADS 1
Negative:
There is nothing to comment on.
The breasts are symmetric and no masses, architectural distortion or suspicious calcifications are present.
BI-RADS 1
DO
- Use BI-RADS 1 if there are no abnormal imaging findings in a patient with a palpable abnormality, possible a palpable cancer, BUT add a sentence recommending surgical consultation or tissue diagnosis if clinically indicated.
BI-RADS 2
Benign Finding:
Like BI-RADS 1, this is a normal assessment, but here, the interpreter chooses to describe a benign finding in the mammography report, like:
- Follow up after breast conservative surgery
- Involuting, calcified fibroadenomas
- Multiple large, rod-like calcifications
- Intramammary lymph nodes
- Vascular calcifications
- Implants
- Architectural distortion clearly related to prior surgery.
- Fat-containing lesions such as oil cysts, lipomas, galactoceles and mixed-density hamartomas. They all have characteristically benign appearances, and may be labeled with confidence.
BI-RADS 2
DO
- Agree in a group practice on whether and when to describe benign findings in a report
- Use in screening or in diagnostic imaging when a benign finding is present
- Use in the presence of bilateral lymphadenopathy, probably reactive or infectious in origin
- Use in diagnostic imaging and recommend management if appropriate,
- - as in abscess or hematoma
- - as in implant rupture and other foreign bodies
DON'T
- Don't use when a benign finding is present but not described in the report, then use Category 1.
- Don't recommend MRI to further evaluate a benign finding.
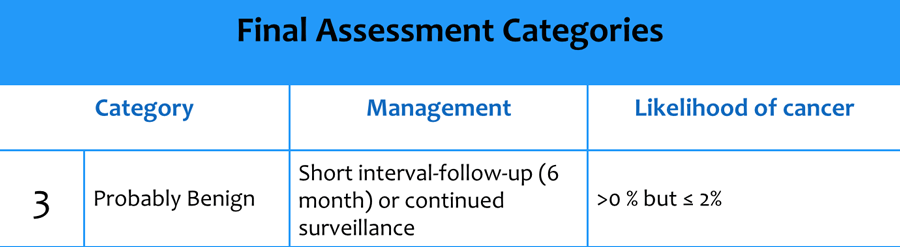
BI-RADS 3
Probably Benign Finding
Initial Short-Interval Follow-Up Suggested:
A finding placed in this category should have less than a 2% risk of malignancy.
It is not expected to change over the follow-up interval, but the radiologist would prefer to establish its stability.
Lesions appropriately placed in this category include:
- Non-calcified circumscribed mass on a baseline mammogram (unless it can be shown to be a cyst, an intramammary lymph node, or another benign finding),
- Focal asymmetry which becomes less dense on spot compression view
- Solitary group of punctate calcifications
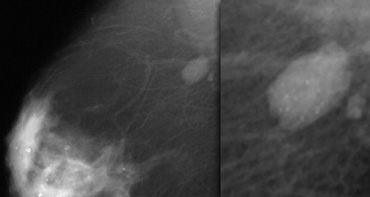
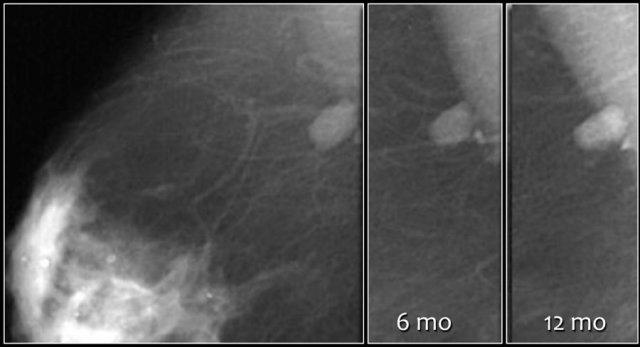
Here a non-palpable sharply defined mass with a group of punctate calcifications.
The mass was categorized as BI-RADS 3.
Continue with follow up images.
- The initial short-term follow-up of a BI-RADS 3 lesion is a unilateral mammogram at 6 months, then a bilateral follow-up examination at 12 months. Assuming stability perform a follow-up after one year and optionally after another year.
- If the findings shows no change in the follow up the final assessment is changed to BI-RADS 2 (benign) and no further follow up is needed.
Follow-up at 6, 12 and 24 months showed no change and the final assessment was changed into a Category 2.
Nevertheless the patient and the clinician preferred removal, because the radiologist was not able to present a clear differential diagnosis.
So add the following sentence in your report:
- BI-RADS 2 (benign finding).
- Instead of stopping the follow-up, tissue diagnosis will be performed, due to patient and referring clinician concern.
PA: benign vascular malformation.
If a BI-RADS 3 lesion shows any change during follow up, it will change into a BI-RADS 4 or 5 and biopsy should be performed.
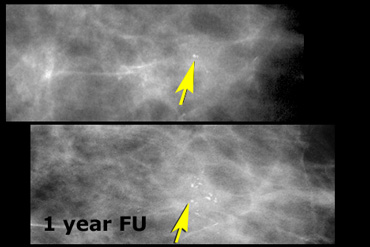
The upper image shows a few amorphous calcifications initially classified as BI-RADS 3.
At 12 month follow up more than five calcifications were noted in a group.
The findings were now classified as BI-RADS 4.
This proved to be DCIS with invasive carcinoma.
BI-RADS 3
DO
- Do perform initial short term follow-up after 6 months. Assuming stability perform a second short term follow-up after 6 months (With mammography: image both breasts). Assuming stability perform a follow-up after one year and optionally another year. Then use Category 2.
- Do realize, that a benign evaluation may always be rendered before completion of the Category 3 analysis, if in the opinion of the radiologist the finding has no chance of malignancy and thus is Category 2.
- Use in findings on mammography like
- Noncalcified circumscribed solid mass
- Focal asymmetry
- Solitary group of punctuate calcifications - Use in findings on US with robust evidence to suggest
- Typical fibroadenoma
- Isolated complicated cyst
- Clustered microcysts - Use in a probably benign finding, while the patient or referring clinician still prefers biopsy. Then add sentence: 'Instead of follow-up tissue diagnosis will be performed, due to patient or referring clinician concern'.
DON'T
- Don't use if unsure whether to render a benign (Category 2) or suspicious (Category 4) assessment. Then use Category 4.
- Don't use in a screening examination
- Don't use in a diagnostic examination if additional imaging is required to make a final assessment
- Don't use if a lesion, previously assessed as Category 3 has increased in size or extent, like a mass on US with an increase of 20% or more of longest dimension. Then use category 4.
- Don't recommend MRI to further evaluate a probably benign finding
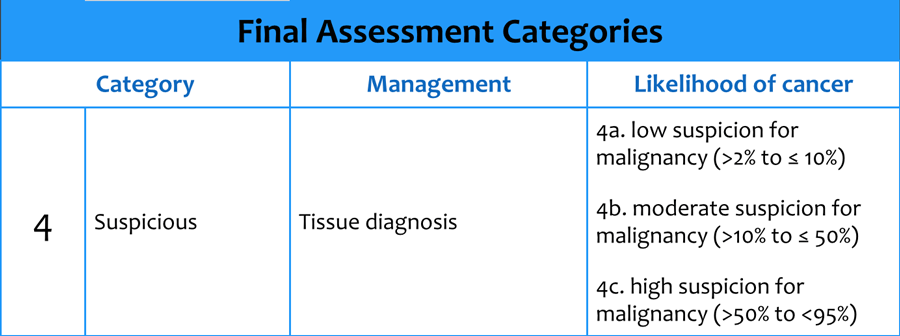
BI-RADS 4
Suspicious Abnormality - Biopsy Should Be Considered:
This category is reserved for findings that do not have the classic appearance of malignancy but are sufficiently suspicious to justify a recommendation for biopsy.
BI-RADS 4 has a wide range of probability of malignancy (2 - 95%).
By subdividing Category 4 into 4A, 4B and 4C , it is encouraged that relevant probabilities for malignancy be indicated within this category so the patient and her physician can make an informed decision on the ultimate course of action.
DO
- Use for findings sufficiently suspicious to justify biopsy
- Use for findings sufficiently suspicious to justify biopsy and the patient or referring clinician refrain from biopsy because of contraindications. Then add sentence: "Biopsy should be performed in the absence of clinical contraindications".
- Use in the presence of suspicious unilateral lymphadenopathy without abnormalities in the breast
- Do use Category 4a in findings as:
- Partially circumscribed mass, suggestive of (atypical) fibroadenoma
- Palpable, solitary, complex cystic and solid cyst
- Probable abscess - Do use Category 4b in findings as:
- Group amorphous or fine pleomorphic calcifications
- Nondescript solid mass with indistinct margins - Do use Category 4c in findings as:
- New group of fine linear calcifications
- New indistinct, irregular solitary mass
The CC mammographic image shows a finding, not reproducible on the MLO view.
This finding is sufficiently suspicious to justify biopsy.
A benign lesion, although unlikely, is a possibility.
This could be for instance ectopic glandular tissue within a heterogeneously dense breast.
This lesion is categorized as BI-RADS 4.
Here another BI-RADS 4 abnormality.
The pathologist could report to you that it is sclerosing adenosis or ductal carcinoma in situ.
Both diagnoses are concordant with the mammographic findings.
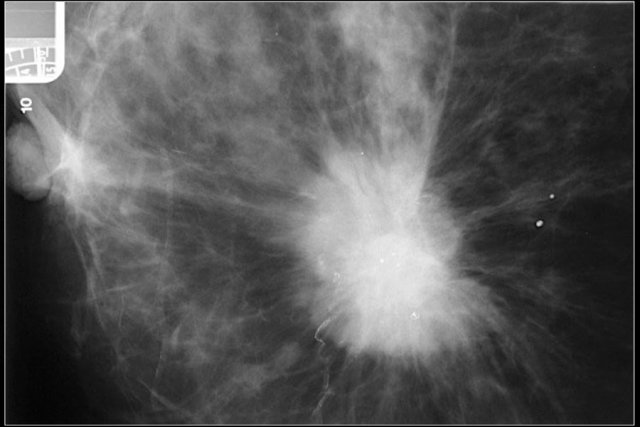
BI-RADS 5
Highly Suggestive of Malignancy.
Appropriate Action Should Be Taken:
BI-RADS 5 must be reserved for findings that are classic breast cancers, with a >95% likelihood of malignancy.
The current rationale for using category 5 is that if the percutaneous tissue diagnosis is nonmalignant, this automatically should be considered as discordant.
- Spiculated, irregular highdensity mass.
- Segmental or linear arrangement of fine linear calcifications.
- Irregular spiculated mass with associated pleomorphic calcifications.
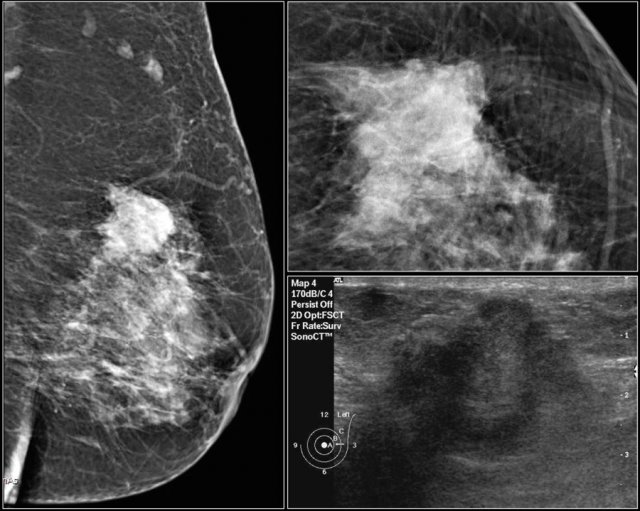
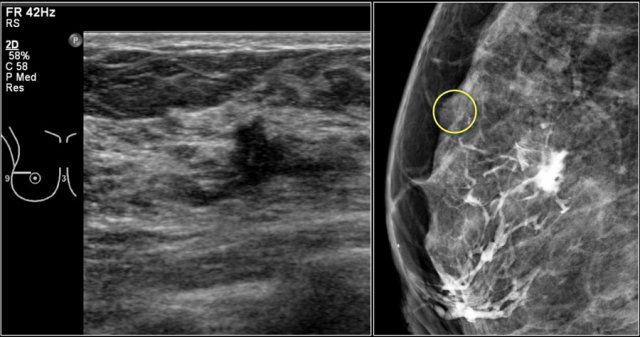
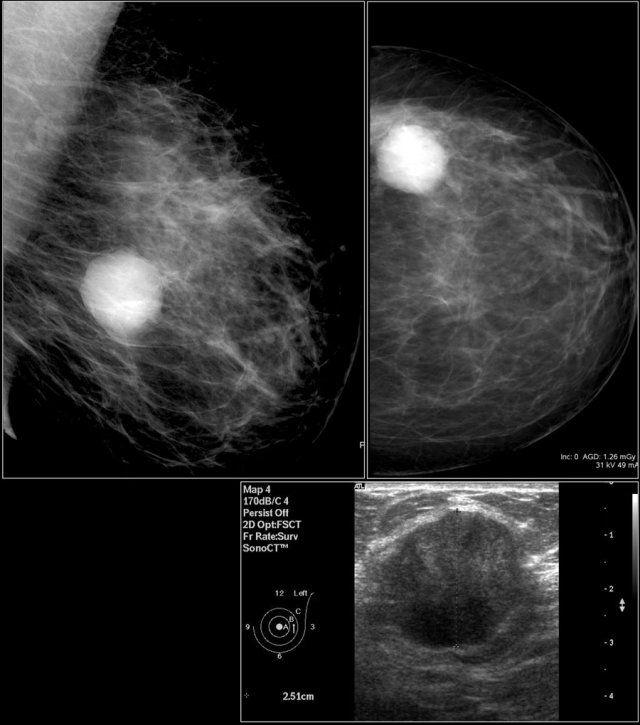
First study the images and describe the findings.
Then continue reading.
The findings are:
- Mass with irregular shape.
- Spiculated margin.
- High density.
- Ultrasound also shows irregular shape with indistinct margin.
This mass is categorized as BI-RADS 5.
BI-RADS 5
DO
- Use if a combination of highly suspicious findings are present:
- Spiculated, irregular mass + high-density.
- Fine linear calcifications + segmental or linear arrangement .
- Irregular spiculated mass + associated pleomorphic calcifications.
- Use in findings for which any nonmalignant percutaneous tissue diagnosis is automatically considered discordant
- Use in findings sufficiently suspicious to justify Category 5 and the patient or referring clinician refrain from biopsy because of contraindications or other concerns.
Then add sentence: "Biopsy should be performed in the absence of clinical contraindications".
DON'T
- Don't use if only one highly suspicious finding is present.
Then use Category 4c.
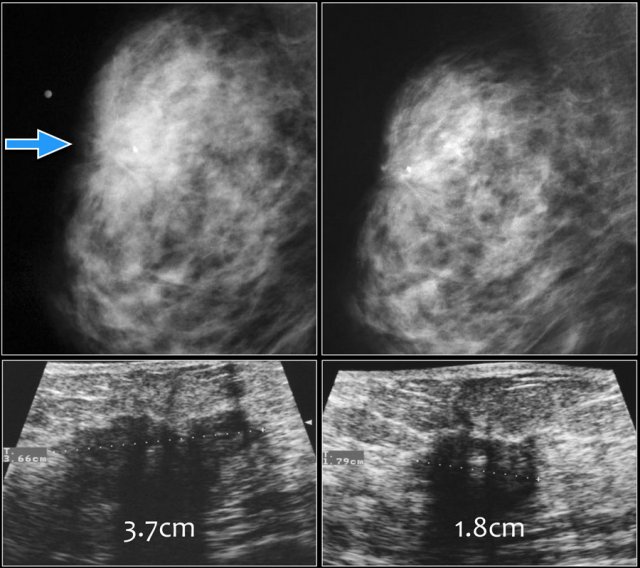
BI-RADS 6
DO
- Use after incomplete excision
- Use after monitoring response to neoadjuvant chemotherapy
DON'T
- Don't use after attempted surgical excision with positive margins and no imaging findings other than postsurgical scarring. Then use category 2 and add sentence stating the absence of mammographic correlate for the pathology.
- Don't use for imaging findings, demonstrating suspicious findings other than the known cancer, then use Category 4 or 5.
Here images of a biopsy proven malignancy.
On the initial mammogram a marker is placed in the palpable tumor.
Due to the dense fibroglandular tissue the tumor is not well seen.
Ultrasound demonstrated a 37 mm mass with indistinct and angular margins and shadowing.
After chemotherapy the tumor is not visible on the mammogram.
Ultrasound showed shrinkage of the tumor to a 18 mm mass, which was categorized as BI-RADS 6.
Location in Mammography and US
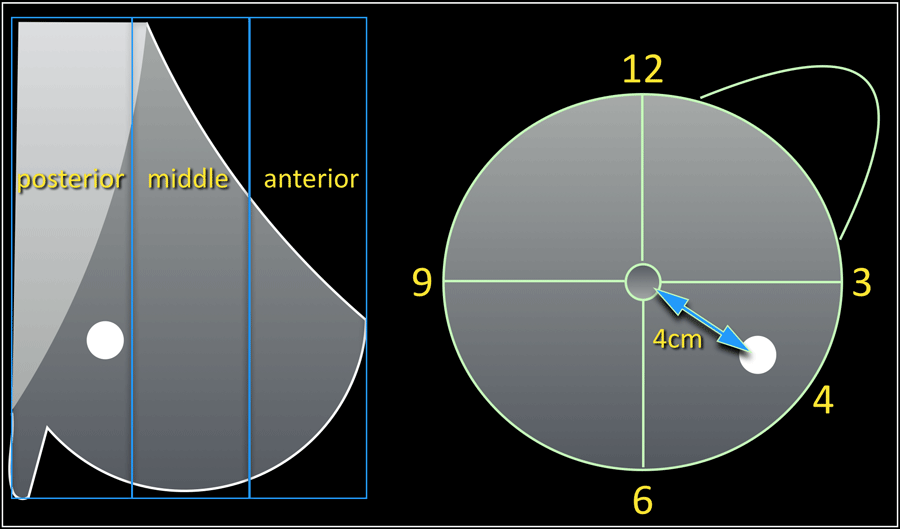 A mass is seen in the outer lower quadrant of the left breast at 4 o' clock in the posterior portion of the breast at 4cm distance from the nipple.
A mass is seen in the outer lower quadrant of the left breast at 4 o' clock in the posterior portion of the breast at 4cm distance from the nipple.
A complete set of location descriptors consists of:
- Designation of right or left breast
- Quadrant and clockface notation (preferably both)
- On US quarter and clockface notation should be supplemented on the image by means of bodymark and transducer position.
- Depth: anterior, middle or posterior third (Mammography only)
- Distance from nipple
There may be variability within breast imaging practices, members of a group practice should agree upon a consistent policy for documenting.
When you use more modalities, always make sure, that you are dealing with the same lesion.
For instance a lesion found with US does not have to be the same as the mammographic or physical finding.
Sometimes repeated mammographic imaging with markers on the lesion found with US can be helpful.
Cysts can be aspirated or filled with air after aspiration to make sure that the lesion found on the mammogram is caused by a cyst.
Solid lesions can be injected with contrast or a marker can be placed in difficult cases.
Here images that you've seen before.
They are of a patient with a new lesion found at screening.
With ultrasound an intramammary lymph node was found, but we weren't sure whether this was the same as the mass on the mammogram.
Continue with the mammographic images after contrast injection.
Contrast was injected into the node and a repeated mammogram was performed.
Here we have proof that the mass is caused by an intramammary lymph node, since the mammographic mass contains the contrast.
This patient presented with a tumor in the left breast.
However in the right breast a group of amorphous and fine pleomorphic calcifications was seen.
Ultrasound examination was performed
Ultrasound of the region demonstrated an irregular mass, which proved to be an adenocarcinoma with fine needle aspiration (FNA).
To find out whether the mass was within the area of the calcifications, contrast was injected into the mass.
The mass is evidently in another region of the breast.
Now a vacuum assisted biopsy has to be performed of the calcifications, because maybe we are dealing with DCIS in one area and an invasive carcinoma in another area.
Size measurement
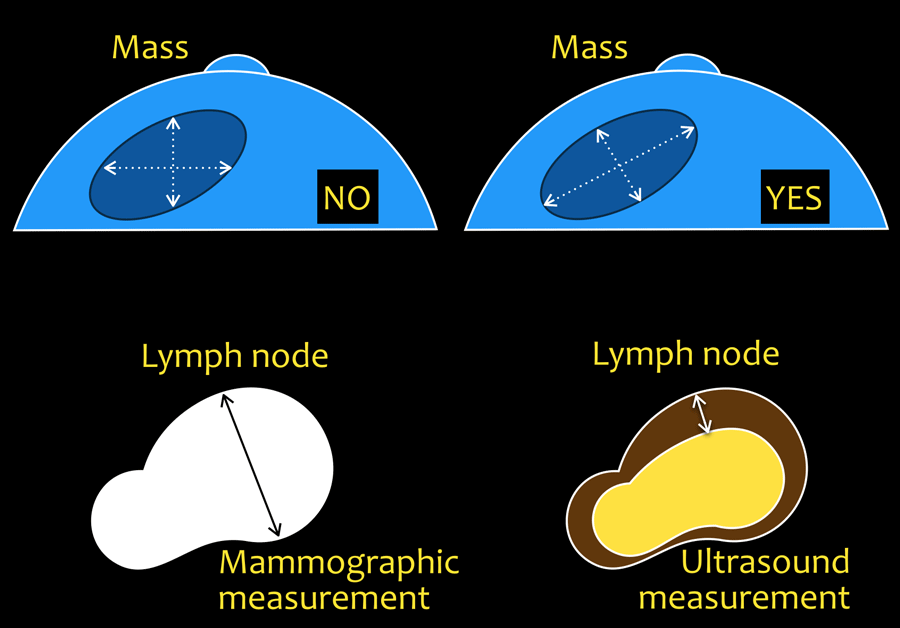
Mass
Longest axis of a lesion and a second measurement at right angles.
In a spiculated mass the spiculations should not be included.
Architectural distortion and Asymmetries
Approximation of its greatest linear dimension.
Calcifications
The distribution should be measured by approximation of its greatest linear dimension.
Lymphnode
Mammography: short axis.
Ultrasound: cortical thickness.
Reporting
- Describe the indication for the study.
Screening, diagnostic or follow-up.
Mention the patient's history.
If Ultrasound is performed, mention if the US is targeted to a specific location or supplementary screening. - Describe the breast composition.
- Describe any significant finding using standardized terminology.
Use the morphological descriptors: mass, asymmetry, architectural distortion and calcifications.
These findings may have associated features, like for instance a mass can be accompanied with skin thickening, nipple retraction, calcifications etc.
Correlate these findings with the clinical information, mammography, US or MRI.
Integrate mammography and US-findings in a single report. - Compare to previous studies.
Awaiting previous examinations for comparison should only take place if they are required to make a final assessment - Conclude to a final assessment category.
Use BI-RADS categories 0-6 and the phrase associated with them.
If Mammography and US are performed: overall assessment should be based on the most abnormal of the two tests, based on the highest likelihood of malignancy. - Give management recommendations.
- Communicate unsuspected findings with the referring clinician.
Verbal discussions between radiologist and referring clinician should be documented in the report.
Examples of reporting
Indication for examination
Painful mobile lump, lateral in right breast. No previous history of breast pathology.
Findings
No previous exams available.
Mammography
Overall breast composition: b. Scattered areas of fibroglandular density.
Lateral in the right breast, concordant with the palpable lump, there is a mass with an oval shape and margin, partially circumscribed and partially obscured.
The mass is equal dense compared to the fibroglandular tissue.
Location: Right breast, 9 o'clock position, middle third of the breast.
Size: approximation of largest diameter = 3 cm.
Additional US of the mass: Concordant with the lump and the mass on the mammogram there is an oval simple cyst, parallel orientation, circumscribed, Anechoic with posterior enhancement. Size : 3,5 x 1,5 cm.
In the right breast at least 2 more smaller cysts.
Assessment
BI-RADS 2 (benign finding).
The palpable mass is a simple cyst. There are at least two more, smaller cysts present in the right breast.
Management
The palpable cyst was painful, after informed consent uncomplicated puncture for suction of the cyst was performed.
No indication for follow-up, unless symptoms return, as explained to the patient.
Note:
- No need to describe the cyst in detail: it is a 'special case'/unique diagnosis.
- No need to describe the additional cysts in more detail or size. Only the size of the most important cyst (1) should be mentioned.
- Do not use terms different from the BI-RADS 2013 descriptors.
- If Mammography and US are performed: Always describe in two paragraphs integrated in a single report.
- Verbal discussions between radiologist, patient and referring clinician should be documented in the original report or in an addendum.
Indication for examination
Referral from general practitioner.
Mobile lump, lateral in left breast, since 2 months.
No previous history of breast pathology.
No previous exams available.
Findings
Mammography: Overall breast composition: a. The breasts are almost entirely fatty.
Lateral in the left breast, at 3 o'clock position in the posterior third of the breast, concordant with the palpable lump there is a 3 cm hyperdense mass with a rounded, but also irregular shape.
The margins are partially circumscribed and partially not circumscribed with some microlobulations.
Ultrasound: concordant with the lump and the mass on the mammogram there is an slightly irregular hypoechoic mass with a non-parallel orientation, > 75% circumscribed and locally indistinct margin.
Assessment
BI-RADS 4a (low suspicion for malignancy).
The palpable mass is concordant with a solid mass, predominantly well circumscribed.
In this 35-year old patient the differential diagnosis consists of an atypical fibroadenoma or a phyllodes.
Management
After informed consent of the patient a 14G core needle biopsy was performed, two specimens were obtained. No complications.
It was discussed with the patient and the referring general practitioner, that in case of BI-RADS 4(a) referral to the breast clinic is advised. The patient and the referring general practitioner preferred to await the results of the biopsy .
Addendum
The biopsy showed a fibro-epithelial lesion, probably a benign phyllodes.
Referral to the breast clinic was now strongly indicated and was put in motion by the general practitioner after telephone consultation.
Diagnosis after excision: 3 cm highly cellular fibroadenoma.