Myelopathy
Majda Thurnher and Robin Smithuis
Department of Radiology of the Medical University of Vienna, Austria and Rijnland hospital in Leiderdorp, the Netherlands
Publicationdate
In this article we will focus on spinal cord diseases that are characterised by high signal within the cord on T2WI.
The most common causes are inflammatory and demyelinating disorders like Multiple Sclerosis, Neuromyelitis Optica, Acute Disseminating Encephalomyelitis and Transverse myelitis.
We will discuss the differential diagnosis including tumors, inflammatory and vascular disorders.
Introduction
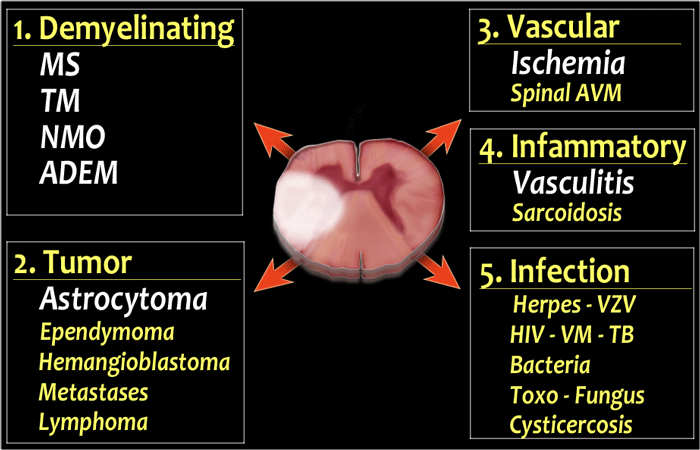
Differential diagnosis
- Demyelinating diseases
The first question is usually is it MS?
Does it look like spinal cord MS and does the brain look like MS.
If the patient has myelopathy and optic neuritis then also think of the possibility of Neuromyelitis Optica (NMO) and do the NMO-IgG test.
If both halves of the cord are involved than think of Transverse Myelitis (TM) which is not a specific diagnosis, but merely a reaction of the cord to various autoimmune and infectious stimuli. - Tumor
The major differential of demyelinating diseases is an astrocytoma, especially if there is swelling and some enhancement of the cord and when the symptoms are more slowly progressive.
The other common spinal cord tumors like ependymoma and hemangioblastoma do not cause differential diagnostic problems, because in most cases they just look like a tumor.
Metastases to the cord are very uncommon. - Vascular
Acute ischemia is typically seen as a complication of aortic aneurysm surgery or catheterisation.
Cord ischemia due to venous hypertension or arterial steal can be seen in vascular malformations like AV-fistula.
So always look for abnormal vessels around the cord. - Infammatory
Vasculitis - Infection
Infection rarely involves the spinal cord.
If we exclude myelopathy due to cord compression as seen in trauma, degeneration and metastatic disease, which is usually not a diagnostic dilemma, then the most common diseases of the spinal cord are demyelinating diseases.
MS is by far the most common demyelinating disease.
The diagnosis can only be made if there is dissemination over time and space.
Many patients who are diagnosed as having acute disseminating encephalomyelitis (ADEM) or Transverse Myelitis, may have recurrent disease and later turn out to have MS (red arrow).
Systematic approach
Whenever there is an abnormality in the spinal cord, we need a systematic approach to analyse the findings.
Clinical findings can be helpful but can be quite similar in most spinal cord disorders.
On MR look for the following:
- Short or Long segment?
In MS there is typically a short segment involved, i.e. less than 2 segments.
In other diseases like Transverse Myelitis, NMO and ischemia there is usually a long segment involved. - How much of the cord is involved on tranverse images?
Partial involvement is typically seen in MS. Complete involvement includes both halves of the cord and is typically seen in TM and NMO. - Location of the involvement on transverse images?
Use high resolution transverse images to detect the location within the cord. Is it posterior like in MS, vitamin B12 deficiensy, lateral like in MS or anterior like in arterial infarction. - Is the cord swollen?
In TM and tumor the cord is swollen, while in MS and ADEM the cord is not swollen or less swollen then you would expect for the size of the lesion. - Is there enhancement?
Many diseases show some enhancement, but the most important thing is that astrocytoma has to be included in the differential diagnosis.
Short or long segment involvement
-
Short segment involvement
- common in:
- MS
- uncommon in:
- Transverse myelitis - partial form
- common in:
-
Long segment involvement
- common in:
- Transverse myelitis - complete form
- Neuromyelitis Optica
- uncommon in:
- MS
- common in:
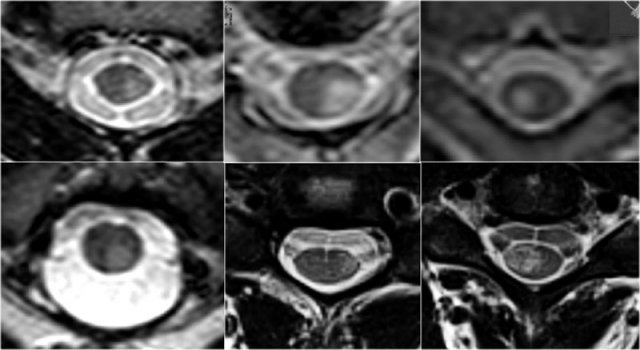
Transverse involvement
Transverse images are very helpful in the differential diagnosis.
You need high resolution images.
Look for how much is involved (both halves or not), which part is involved and what is the form of the involvement.
-
MS typically is triangular in shape and mostly located dorsally or laterally.
However MS can look like anything and may uncommonly involve the whole transverse diameter or only the anterior part. - Ischemia as a result of arterial infarction is typically located in the anterior parts, but may involve the entire transverse diameter.
- Transverse myelitis and Neuromyelitis optica typically involve the whole cord.
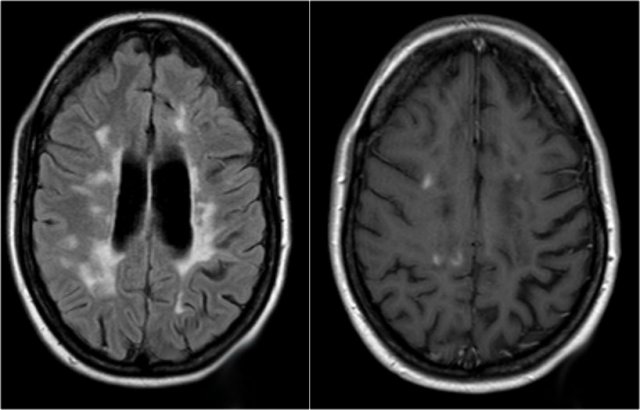
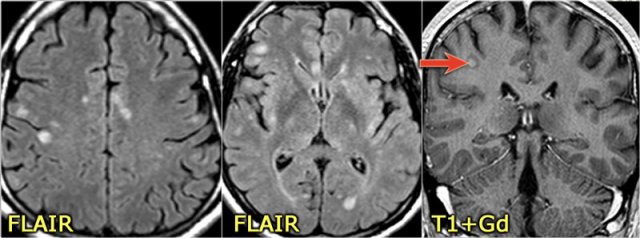
Brain abnormalities
In many cases of myelopathy there will also be brain abnormalities and these can be a diagnostic clue to the diagnosis.
Multiple Sclerosis
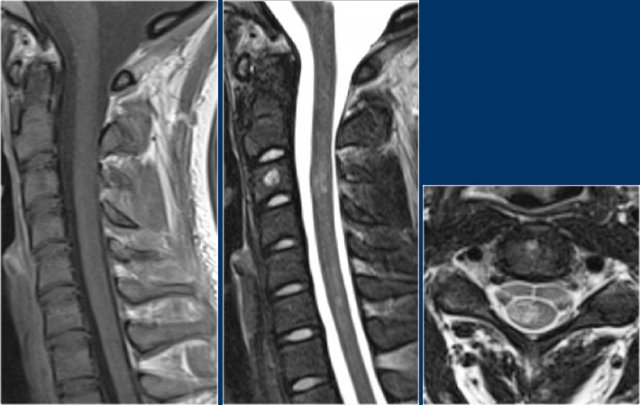
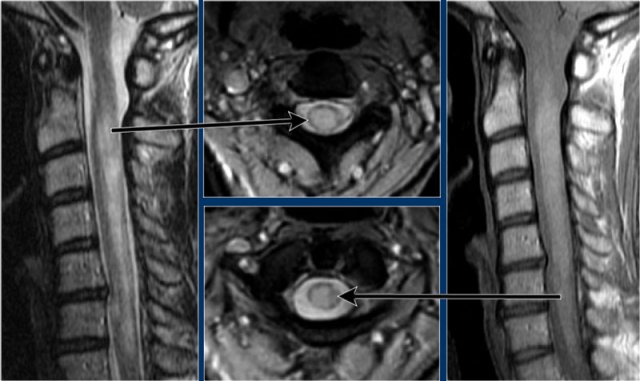
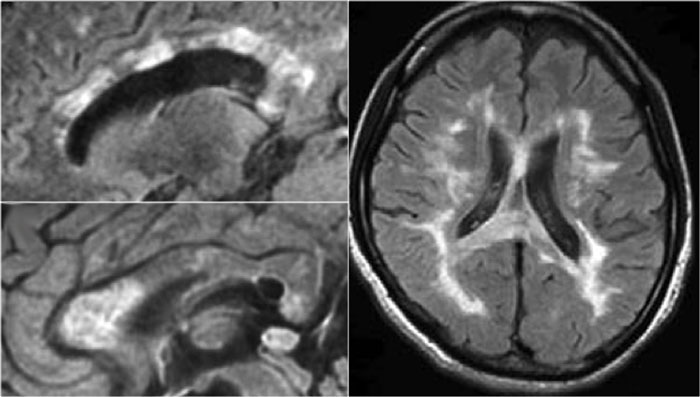
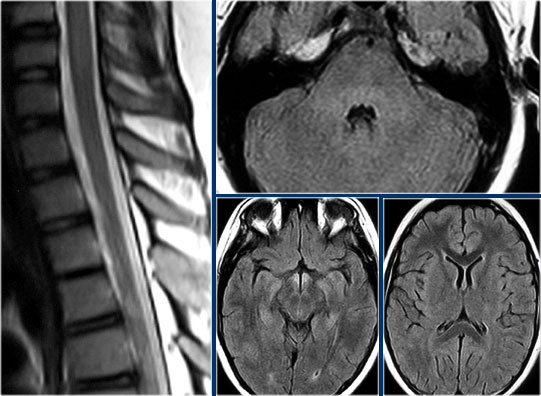
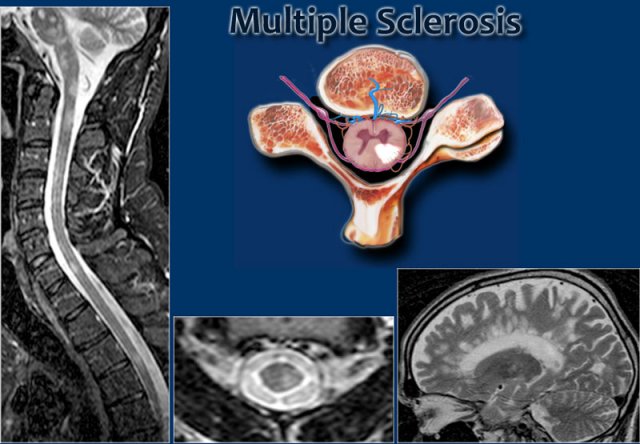 MS: short segment focal wedge-shaped involvement of the posterior column of the spinal cord with typical periventricular WM-lesions.
MS: short segment focal wedge-shaped involvement of the posterior column of the spinal cord with typical periventricular WM-lesions.
key facts:
- MS is an immune-mediated inflammatory demyelinating disease of the brain and the spinal cord.
- Multiple lesions disseminated over time and space.
- Brain lesions are typically in periventricular, subcortical and cerebellar white matter and also in brainstem and corpus callosum.
- CSF: monoclonal bands.
MS is the most common demyelinating disease and there is overlap between these diseases.
NMO was first thought to be a form of MS, but is now considered to be a distinct form.
ADEM can relapse and progress to MS.
The partial form of transverse myelitis
Here we have images of a typical case.
Many times the clinical history is very helpful like in this case.
This 24-year old patient had visual disturbances on one eye followed by weakness and sensory disturbances of the lower and upper extremities a couple of years later.
Now she presents with sensory disturbances of both lower extremities.
So we already think MS.
In the cord there are some well-defined lesions, but also some ill-defined foggy lesions.
The transverse image shows the dorsal location and the typical triangular shape.
Continue with the contrast-enhanced images
On the contrast-enhanced images there is no enhancement.
Active MS-lesions in the spine may enhance, but it is not that common as we see in active lesions in the brain.
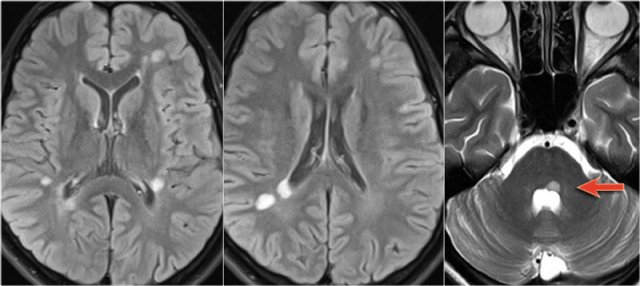
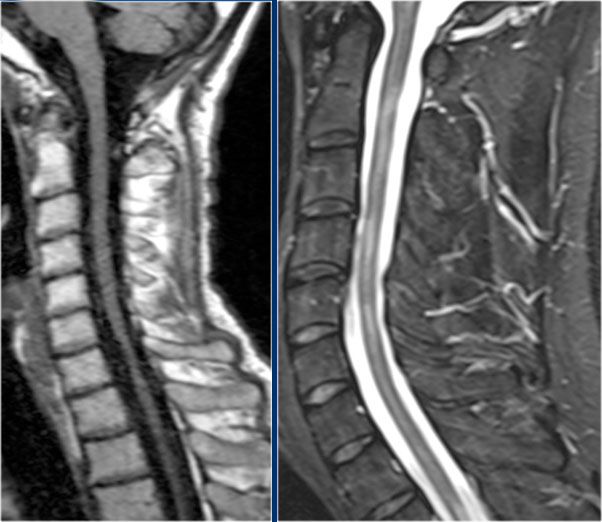
Whenever spinal lesions are encountered, it can be helpful to image the brain aswell.
Now sometimes the patient is only sceduled for MRI of the spine and you don't have time to do a full brain examinations.
In those cases consider to do only a sagittal FLAIR.
Continue with the images of the brain.
The MRI of the brain shows periventricular lesions and a lesion in the corpus callosum.
These locations are very specific for MS.
In another patient there are non-specific lesions in the cord.
Based on the examination of the spine alone, we have a broad differential diagnosis.
However when we examine the brain, it becomes obvious that we are dealing with MS.
Continue with the images of the brain.
In this case the findings in the brain are very helpful.
The location of the lesions is very typical: pons, periventricular and subcortical.
Now what can we expect in the spinal cord of patients with MS.
It is like in the brain.
Frequently the lesions are focal like we see on the left image.
Less commonly there are diffuse abnormalities and then we have a tough differential diagnosis which will include TM and NMO.
In long standing cases atrophy will be seen.
One third of MS patients will have spinal symptoms.
One third of patients have isolated spinal MS without any findings in the brain.
However pathologic studies have shown that 95% of MS patients have spinal cord lesions, whether they have spinal symptoms or not.
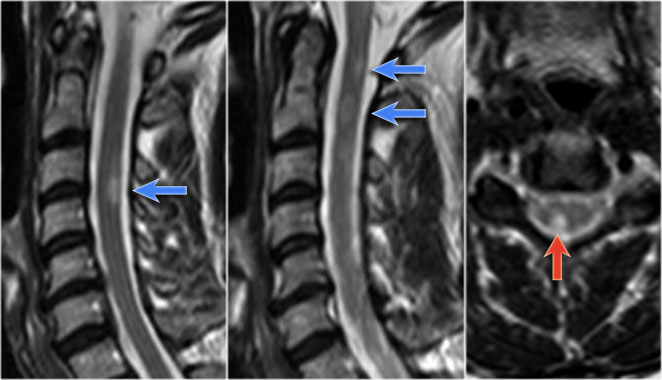
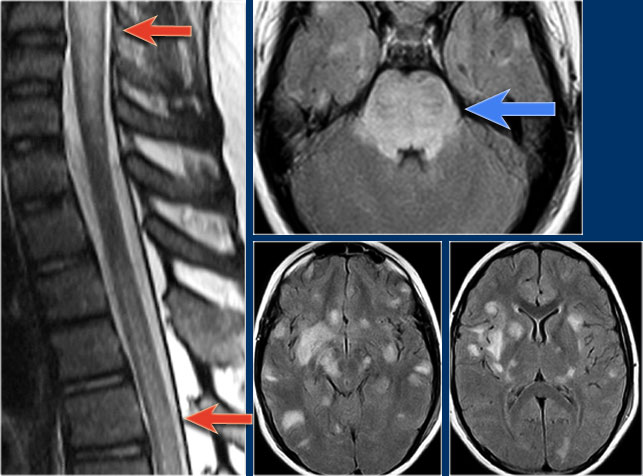
On transverse images MS lesions typically have a round or triangular shape and are located posteriorly or laterally.
So can we exclude MS if a lesion is located anteriorly?
Unfortunately not.
MS is the great mimicker and can also be located anteriorly like in this patient who has a lesion in the typical location (blue arrow) but also a lesion ventrally in the cord (red arrow).
This is uncommon, but you can not exclude MS.
When MS lesions are active, they can enhance, but enhancement is not as common as in the brain.
The enhancement patterns are non-specific.
You can see ring enhancement, intense and less-intense enhancement.
The less intense or vague enhancement is the most common pattern.
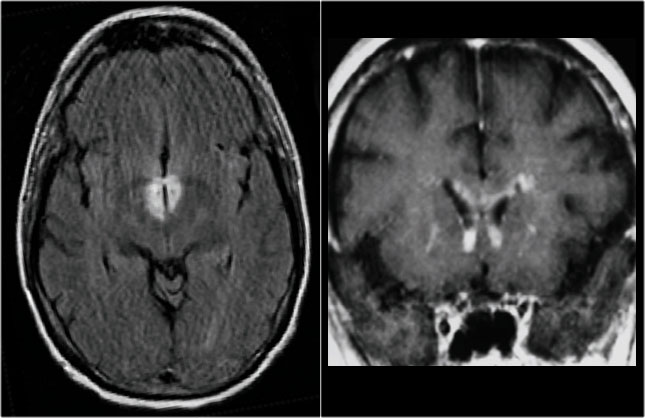
These are images of a patient with longstanding MS and acute exacerbation.
There is enhancement in the active lesions.
Continue with the images of the cervical spine.
Also in the spinal cord there are multiple lesions.
On the transverse image a typical triangular shaped dorsal lesion is seen.
Continue with the contrast-enhanced images.
Also in the spine there are multiple enhancing MS-lesions.
MS usually presents with focal abnormalities.
Diffuse abnormalities that can look like transverse myelitis or extensive astrocytoma are sometimes seen.
This pattern is more common in primary progressive and secondary progressive MS.
Some say that spinal cord atrophy is specific for primary progressive MS (PPMS).
The atrophy correlates very well with the clinical disability.
It is more prominent in the upper part of the spinal cord.
Duration of the disease is the most important determinant of cord atrophy.
Neuromyelitis Optica
key facts:
- Neuromyelitis Optica (NMO) is an autoimmune demyelinating disease induced by a specific auto-antibody, the NMO-IgG.
- NMO preferentially affects the optic nerve and spinal cord.
- Brain lesions do occur and often are distinct from those seen in MS.
- Demyelination of the spinal cord looks like transverse myelitis, i.e. often extensive over 4 -7 vertebral segments and the full transverse diameter.
- NMO IgG is a specific biomarker for NMO.
- Female:male = 9:1
- Also called Devic disease
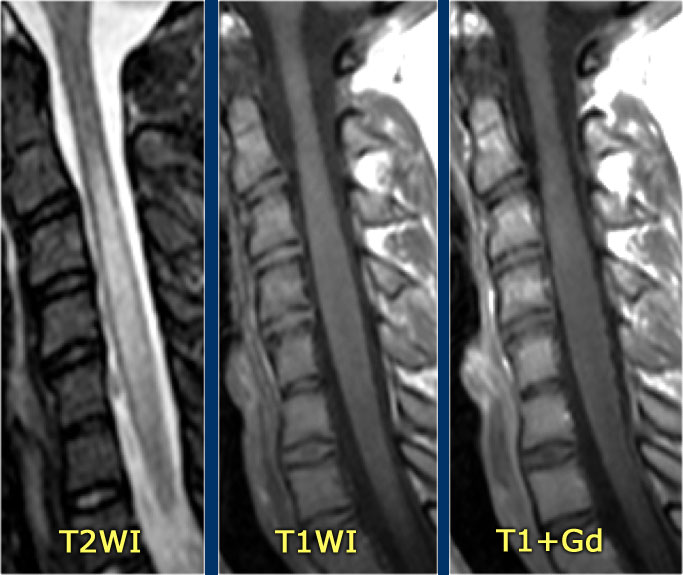
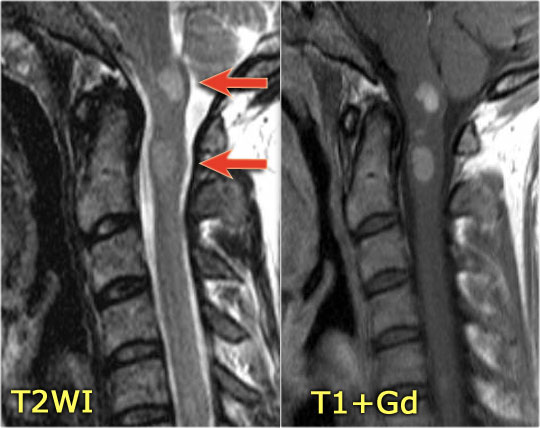
On the left images of a child who presented with unilateral neuritis optica.
Images of the brain were otherwise normal.
Continue with MRI of the spine.
Patients who have one episode of optic neuritis or myelitis and who test positive for NMO-IgG are at high risk for developing the full spectrum of NMO.
One month later this child presented with acute transverse myelopathy, i.e. bilateral symptoms.
The images show abnormal signal in the spinal cord with swelling and some enhancement.
An astrocytoma could very well present with these images, but given the history of an optic neuritis and the acute myelopathy, we do not think of a tumor.
This proved to be NMO and the Ig-test for NMO was positive.
In the original description of Devic's disease the optic neuritis and the myelopathy were simultaneously, but now we know that this is not always the case.
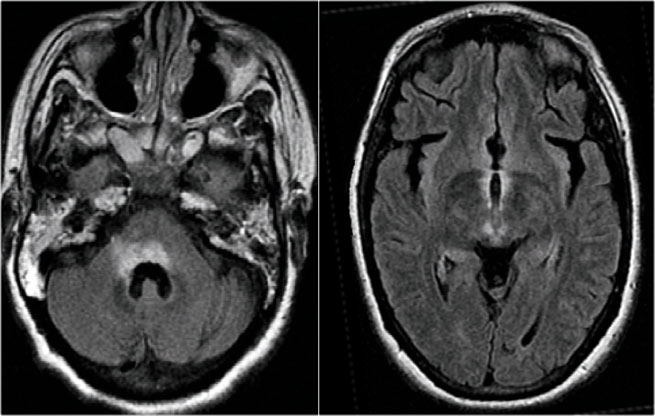
Brain lesions in NMO
Previously it was thought that in NMO the brain was spared, but now we know, that brain lesions do occur.
They are often distinct from those seen in MS.
In Asia 60-80% of patients with NMO have brain abnormalities.
In Europe only 25-40%.
The location of the brain lesions in NMO is only around the ventricles.
The reason why these brain lesions are located around the ventricles is the following:
The NMO IgG auto-antibodies are directed against Aquaporin-4 water-channels.
So just like sodium- and potassium channels in the cells, there are also water-channels.
The highest concentration of these Aquaporin-4 water-channels is seen around the ventricles.
The images show abnormal signal around the third and frontal horns of the lateral ventricles.
Things become even more complicated, since it is also possible to have large lesions in the corpus callosum of patients with NMO as was described by Nakamura (6).
So in any CNS disease with optic nerve and spinal cord involvement it is goos to do the test for NMO-IgG.
ADEM
key facts:
- Acute disseminated encephalomyelitis (ADEM) is an inflammatory demyelinating disease of the CNS after viral infection or vaccination.
- In 75% of patients there is a clear infectious event or vaccination (1-4 weeks)
- Typically monophasic in 90%.
- Multiphasic illness in 10%. In these cases ADEM behaves like MS and cannot be differentiated from MS.
- Mostly seen in young children.
- In 50% of ADEM patients the anti-MOG IgG test is positive and supports the diagnosis. This is antibody-reactivity against Myelin Oligodendrocyte Glycoprotein (MOG).
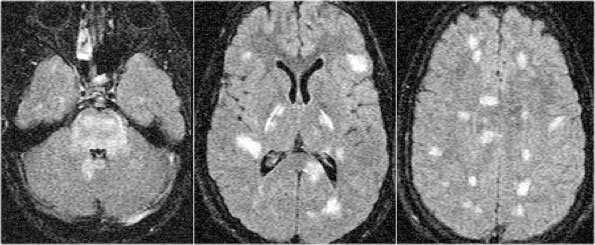
On the left images of a teenage child with a typical history:
- Three weeks after respiratory infection sudden onset of neurological symptoms.
-
Dysarthria, dysphagia, tetraplegia.
Eye movement disturbance and impairment in consciousness.
This clinical history is typical for ADEM.
Usually the brain is also involved.
30% of cases has spinal involvement.
The imaging findings in this case are also typical.
There is swelling and cord involvement like in TM and no enhancement.
Continue with the images of the brain.
First look at the images of the brain and decide what is different from MS-lesions.
What is typical for ADEM and uncommon for MS is:
- Massive involvement of the pons.
- Involvement of the basal ganglia.
The follow up MR shows that the cord has returned to normal again.
On the left another case of ADEM.
ADEM is typically seen in children.
Again there is diffuse involvement of the spinal cord without enhancement and there is involvement of the brain.
Another case of ADEM.
Notice the typical involvement of the pons and basal ganglia.
Continue with follow up scan.
On follow up scan almost complete normalisation.
Transverse Myelitis (TM)
key facts:
- Focal inflammatory disorder of the spinal cord resulting in motor, sensory and autonomic dysfunction.
-
Imaging findings:
- More than 2/3 of the cross sectional area is involved.
- Focal enlargement.
- T2WI hyperintensity
- Enhancement + / -.
- Two forms of TM:
- Acute partial transverse myelitis - APTM
Lesions extending less than two Segments.
These patients are at risk of developing MS. - Acute complete transverse myelitis - ACTM
Lesions extending more than two Segments .
- Acute partial transverse myelitis - APTM
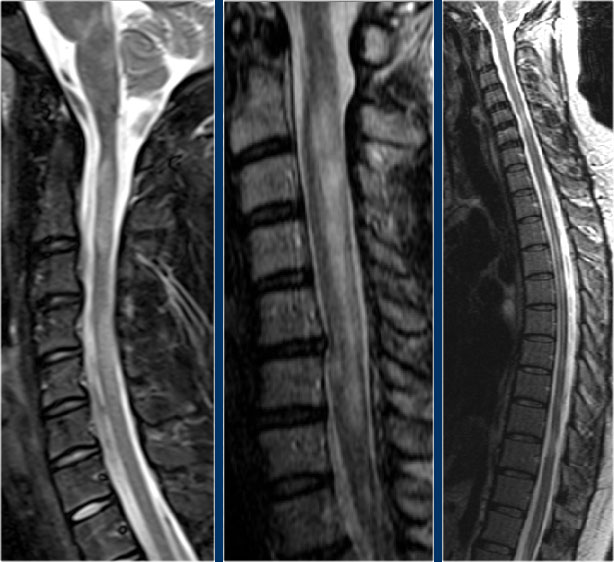
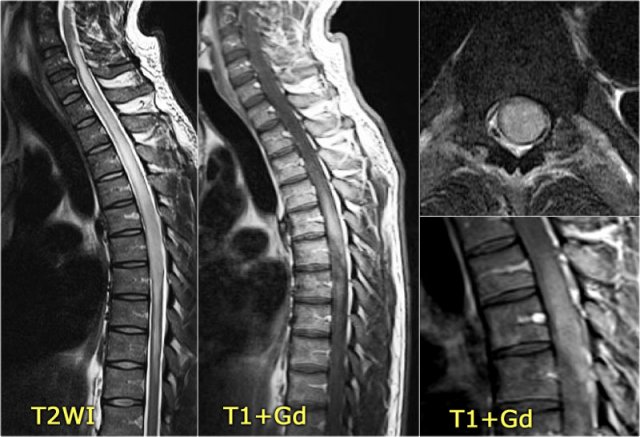
The sagittal image shows a large segment of hyperintensity on T2WI.
The transverse image shows that most of the cord is involved.
These images are of a 31 year old male with headache, voiding disturbances, urinary retention, sensory level C3.
The CSF analysis revealed 400/3 cells (meaning no infection) and a slightly higher protein level.
The images show a long segment myelopathy with full transverse involvement.
There is no swelling and no enhancement.
It does not look like MS or tumor, so we are thinking ATM - acute transverse myelitis.
Diseases associated with Transverse Myelitis
Transverse myelitis may occur in isolation or in the setting of another illness.
When it occurs without apparent underlying cause, it is referred to as idiopathic.
Idiopathic transverse myelitis is assumed to be the result of abnormal activation of the immune system against the spinal cord.
The table provides a list of illnesses associated with TM (7).
Patients with an acute short segment TM (or APTM) are at risk of developing MS if there is one of the following:
- partial TM, i.e. short segment TM.
- Family history of MS. Brain lesions on MR.
- Oligoclonoal bands in CSF.
In children with TM the expression is usually more severe.
60-90% are unable to move their legs.
However the outcome is usually better than in adults and in 30-50% there is complete recovery.
Typical for TM is that on the initial MR the abnormalities are usually extensive and less or completely resolved on follow up scans.
Longitudinal case series of TM reveal that approximately 1/3 of patients recover with little to no sequelae, 1/3 are left with moderate degree of permanent disability, and 1/3 have severe disabilities.
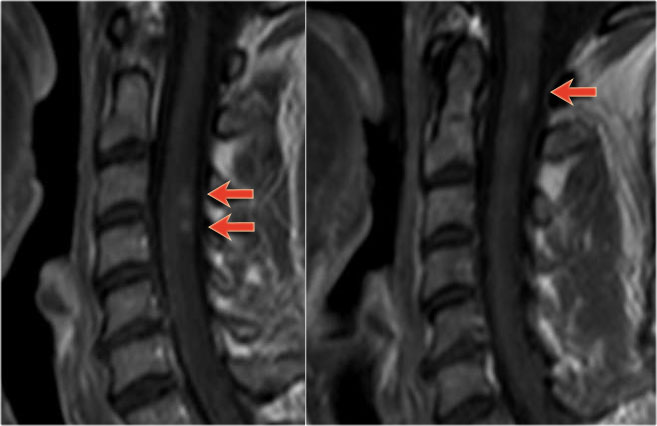
Here images of a typical case of TM.
There is multisegment high signal on STIR and T2WI with some swelling.
Most of the cord in the transverse diameter is involved.
There is no enhancement, which is usually the case in TM.
Sometimes there is some patchy enhancement.
When there is enhancement, it can be difficult to differentiate TM from an astrocytoma.
On the left images of a 60 year old male with an astrocytoma.
He presented with pain in the thoracic region and sensory disturbances in the left lower extremity followed by left hemiparesis.
There is multisegment high signal on T2WI with some swelling, just like we have seen in cases of TM.
On CE-T1WI there is a region of enhancement.
The region of enhancement is more tumor-like, but the differentiation is difficult.
Spinal cord tumor
Astrocytoma
As we have just seen, the major differential of the spinal cord diseases that we have discussed so far is an astrocytoma.
Astrocytoma is a diffusely infiltrating tumor, that is not mass-like.
Usually there is some patchy enhancement.
On the left an astrocytoma in a 66 year old patient who presented with progressive sensory complaints.
Biopsy revealed astrocytoma.
Continue with the follow up.
The patient was not operable and a follow up scan shows progressive disease.
The other two common spinal cord tumors are ependymoma and hemangioblastoma and they just look like a tumor.
They present as enhancing masses and will not cause a differential problem.
All other cord tumors are uncommon.
The images are of a patient with neurofibromatosis who has multiple ependymomas.
They present as multiple enhancing masses.
Vascular
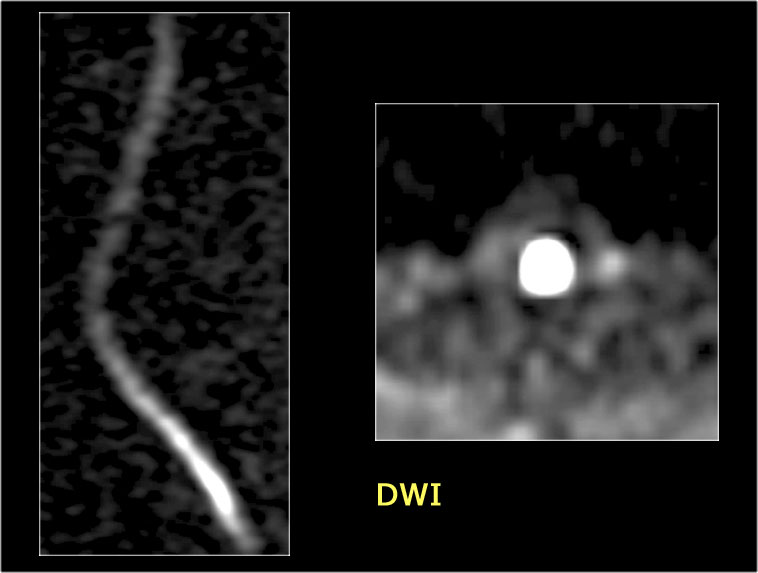
Arterial infarction
Spinal cord ischemia is typically seen as a complication of aortic aneurysm surgery or stenting.
The images are of a patient who developed a paraparesis after stenting of an aortic aneurysm.
Notice the high signal ventrally in the chord, which is typical for arterial infarction.
On transverse images a typical snake-eye appearance can be seen.
Aortic aneurysm stenting is the most common cause of spinal chord infarction.
The diffusion images show restricted diffusion.
Vasculitis
The images are of a child with headache, fever, hyperalgesia and numbness of the left side of the body.
There is also abducens nerve palsy.
The images are non-specific with multiple focal lesions and probably the first choise would be MS.
The differential diagnosis would include inflammation, infection and metastases.
In such cases always perform a transverse image of the spine to look for the exact location and perform a MRI of the brain.
Continue.
The lesions are located dorsally and one of the lesions is enhancing.
Now if this was infection or metastases it would be strange that not all lesions enhance.
MS is still on our list.
Continue with the MR of the brain.
On the CE-T1WI only one lesion shows enhancement.
The location of the lesions and the enhancement could very well fit to the diagnosis of MS, but this proved to be vasculitis.
Vasculitis can be idiopathic, but is also seen in SLE, Sj?gren and Behcet.
Normally you think of vasculitis as a disease of the vessels in the brain, but all vasculitis can be seen in the spine as well.
It produces MS-like images.
Spinal AVF
The most common vascular malformation of the spinal cord is the dural AV-fistula.
It consist of an abnormal connection between the artery and the veins , which can lead to increased venous pressure and predisposes the cord to ischemia and less commonly to hemorrhage.
AVF's are mostly seen in the elderly population and are believed to be the result of trauma.
An accurate diagnosis is important because these lesions may represent a reversible cause of myelopathy.
Notice the high signal in the lower thoracic cord and the surrounding dilated vessels on the T2WI.
On the enhanced T1WI there is subtle enhancement.
Another case with myelopathy and dilated veins as a result of an AVF.
Another patient with myelopathy and dilated vessels surrounding the cord.
Notice the hypointense areas on the T2WI which represents hemorrhage.
Another AVF with myelopathy and dilated vessels.
Cord compression
Although beyond the scope of this article, the most common cause of myelopathy is cord compression as seen in trauma, metastatic disease and epidural hemorrhage.
This patient has a fracture with posterior displacement.
There is myelopathy due to traumatic cord compression.
Another case of cord compression in a patient who was treated with anticoagulantia.
There is myelopathy as a result of compression by a dorsally located epidural hemorrhage.
The most common cause of cord compression is metastatic disease.
Notice the abnormal signal in the vertebral body as a result of a metastasis which extends into the vertebral canal.