Sclerotic bone tumors
Henk Jan van der Woude and Robin Smithuis
Radiology department of the Onze Lieve Vrouwe Gasthuis, Amsterdam and the Rijnland hospital, Leiderdorp, the Netherlands
Publicationdate
In the article Bone Tumors - Differential diagnosis we discussed a systematic approach to the differential diagnosis of bone tumors and tumor-like lesions.
The differential diagnosis mostly depends on the age of the patient and the findings on the conventional radiographs.
In this article we will discuss the differential diagnosis of sclerotic bone tumors and tumor-like lesions in more detail.
Introduction
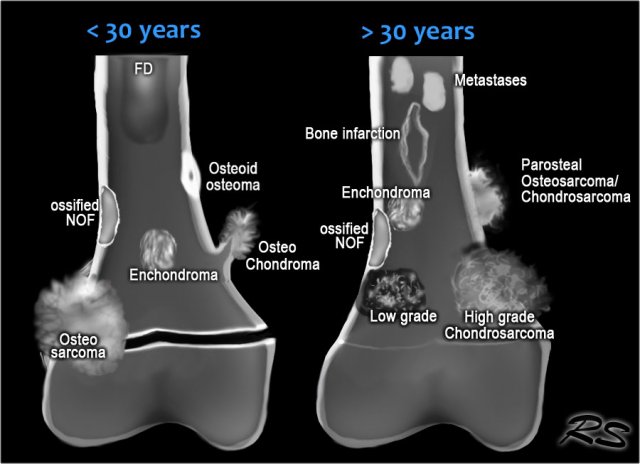
Here an illustration of the most common sclerotic bone tumors.
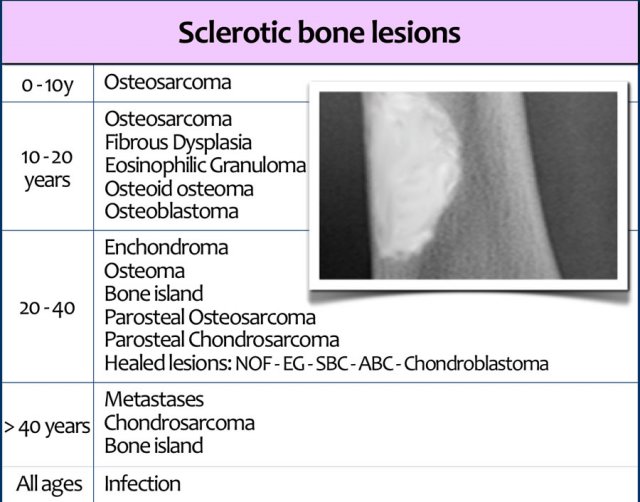
In the table the most common sclerotic bone tumors and tumor-like lesions in different age-groups are presented.
Fibrous dysplasia and eosinophilic granuloma more commonly present as osteolytic lesions, but they can be sclerotic.
Notice that many benign osteolytic lesions that are frequently seen in younger age groups may heal and appear as sclerotic lesions in the middle aged group.
Infection is seen in all ages.
Particularly chronic osteomyelitis may have a sclerotic appearance.
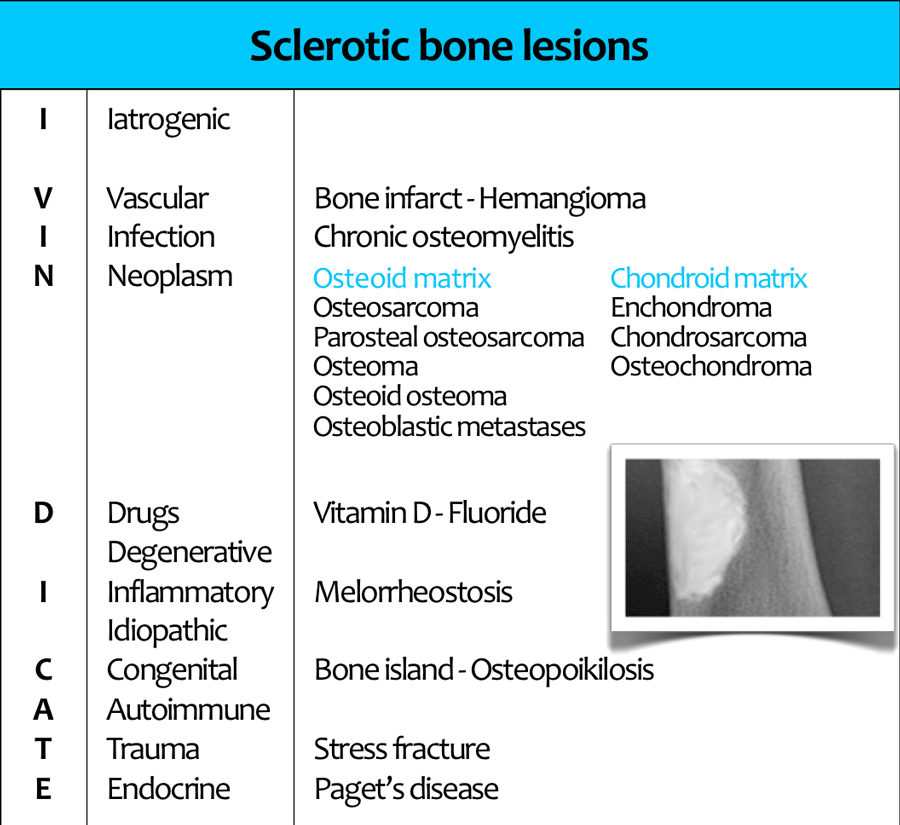
Another approach to the differential diagnosis of sclerotic bone lesions is to use the mnemonic I VINDICATE, which means 'I clear myself from accusation'.
The mnemonic I VINDICATE is a commonly used mnemonic for the differential diagnostis of any radiological lesion.
Bone infarction
Key facts
- Typical presentation: central lesion in metaphysis or diaphysis with a well defined serpentiginous border.
- May resemble cartilaginous tumors.
- Causes: corticosteroid use, sickle cell disease, trauma, Gaucher's disease, renal transplantation.
The term bone infarction is used for osteonecrosis within the diaphysis or metaphysis.
If the osteonecrosis is located in the epiphysis, the term avascular osteonecrosis is used.
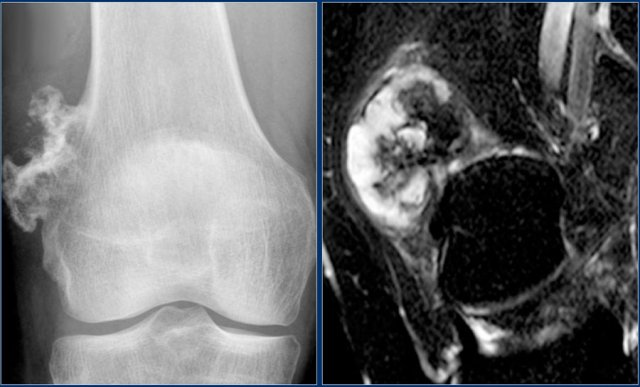
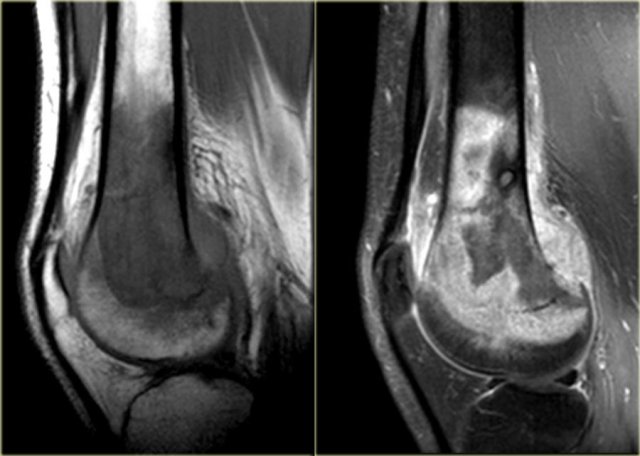
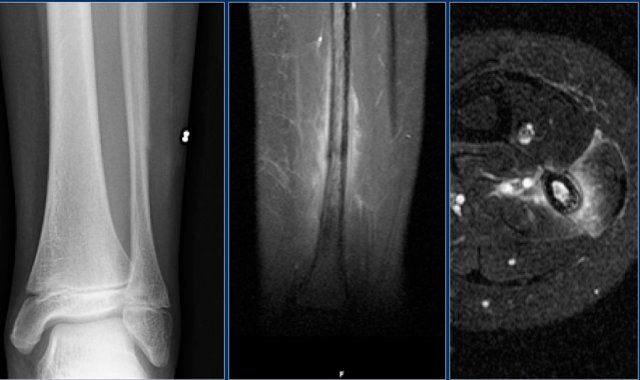
The radiograph shows typical bone infarcts in diaphysis and metaphysis of femur and tibia..
On MR imaging bone infarcts are characterized by irregulair serpentiginous margins with low signal intensity on both T1 and T2 WI and with intermediate to high fat signal in the center part.
Enhancement after i.v. Gadolinium is usually minimal or absent (see right image).
At the periphery of the infarct a zone of relative high signal intensity on T2WI may be found.
Differentiating a bone infarct from an enchondroma or low-grade chondrosarcoma on plain films can be difficult or even impossible.
Cartilaginous tumors in particular chondrosarcoma may show endosteal scalloping, while a bone infarct does not.
Chrondroid tumors are more frequently encountered than bone infarcts.
Here a lesion in the epiphysis, which was the result of post-traumatic osteonecrosis.
In the epiphysis we use the term avascular necrosis and not bone infarction.
Bone island
Key facts
- Benign lesion consisting of well-differentiated mature bone tissue within the medullary cavity.
- Also known as enostosis
- The shape is usually round or oval.
- Frequently encountered as a coincidental finding and can be found in any bone.
- Occasionally slowly enlargement can be seen.
- Bone islands can be large at presentation.
- Bone scan shows no high activity, opposed to low-grade intraosseous osteosarcoma
Click here for more information about bone island.
Chondroblastoma
key facts:
- Typical presentation: well-defined osteolytic lesion in tarsal bone, patella or epiphysis of a long bone in a 20-year old with pain and swelling in a joint.
- Abundant edema is almost always present.
- DD: Ganglion cyst, osteomyelitis, GCT, ABC, enchondroma.
Here a lesion located in the epi- and metaphysis of the proximal humerus.
The lesion is predominantly calcified.
Coronal T1W image shows lobulated margins and peripheral low SI due to the calcifications.
Click here for more examples of chondroblastoma.
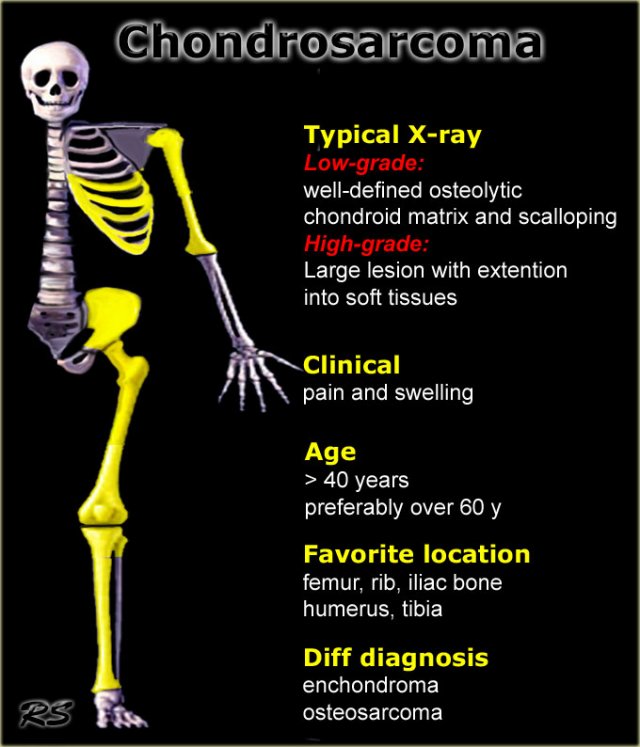
Chondrosarcoma
Key facts
- Most common malignant bone tumor, which is almost always low-grade
- Primary sites of origin: proximal long bones, around knee, pelvis and shoulder girdle, usually central and metaphyseal
- Radiological hallmark: formation of a chondroid (cartilagenous) matrix, which presents as punctuated, stippled or popcorn-like calcifications.
- The chondroid matrix is of a variable amount from almost absent to dens compact chondroid matrix.
- Disappearane of calcifications in a pre-existing enchondroma should raise the suspicion of malignant transformation.
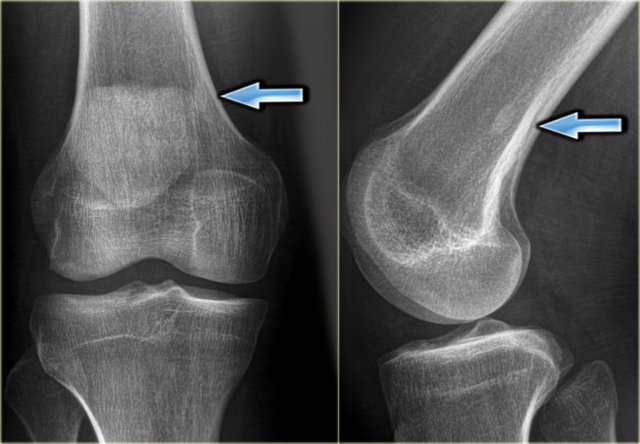
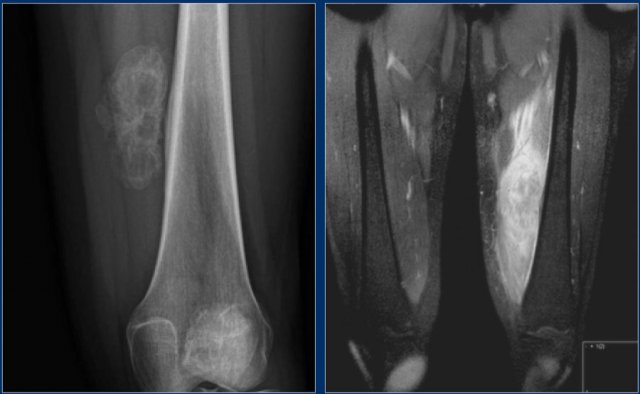
The image shows a calcified lesion in the proximal tibia without suspicious features.
This could very well be an enchondroma.
There were other features that favored the diagnosis of a low-grade chondrosarcoma like a positive bone scan and endosteal scalloping of the cortical bone on an MRI (not shown).
A chondrosarcoma was diagnosed at biopsy.
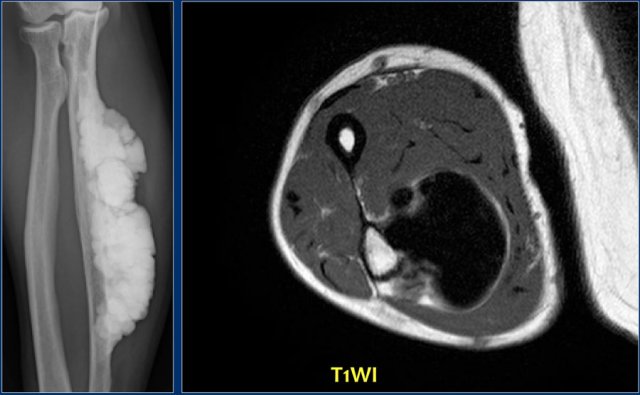
Here a 44-year old male with a mixed lytic and sclerotic mass arising from the fifth metacarpal bone.
There are calcified strands within the soft tissues.
T2-weighted axial MR image demonstrates high signal intensity of the tumor in the metacarpal bone with extension of a lobulated soft tissue mass.
Diagnosis: chondrosarcoma grade 2
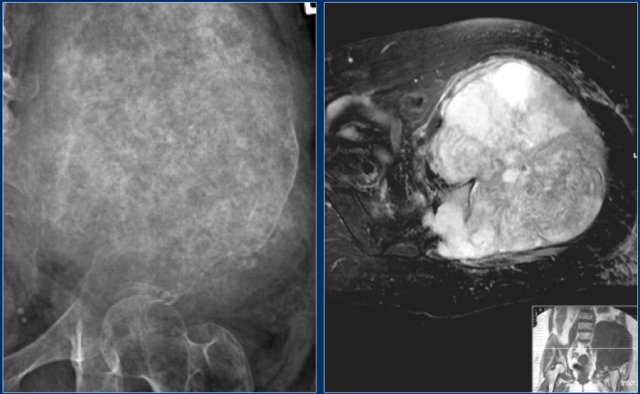
Here a chondrosarcoma of the left iliac bone.
Because of the large dimensions with soft tissue extension on plain radiograph and axial T2-weighted MR image, a high grade chondrosarcoma was suspected.
Biopsy showed grade 2 chondroarcoma.
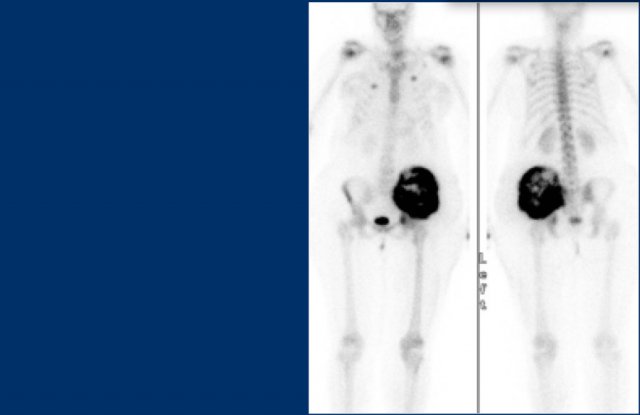
Continue with the bone scan.
Intense uptake on bone scintigraphy as we would expect in high grade chondrosarcoma.
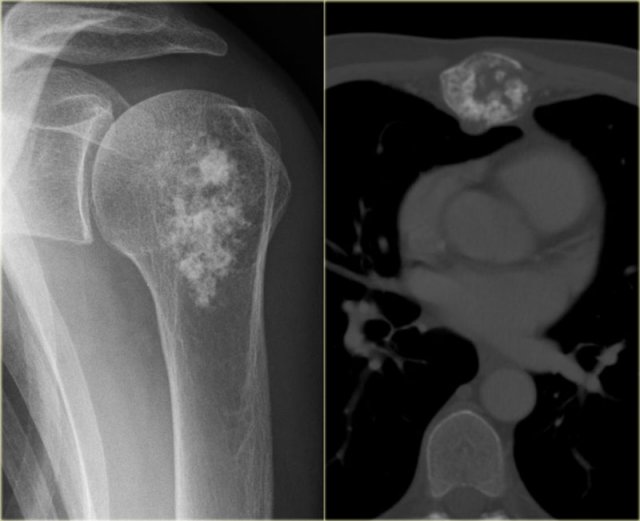
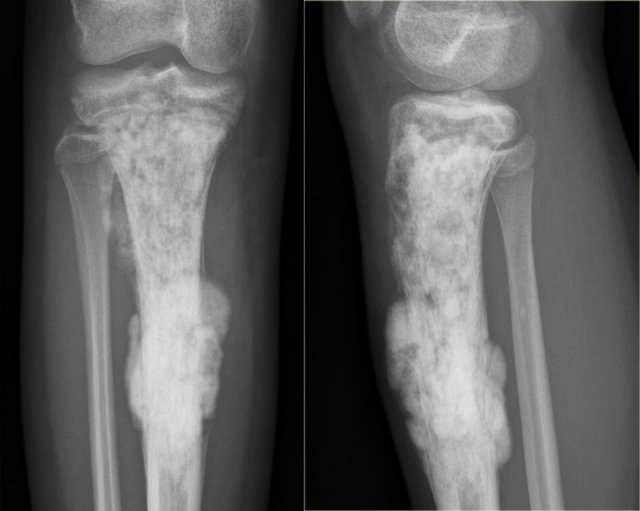
Here two other lesions in different patients that proved to be chondrosarcoma.
The sclerotic lesion in the humeral head could very well be a benign enchondroma based on the imaging findings.
Symptoms are usually absent, however, in adult patients with a chondroid lesion in a long bone, particularly of larger size, always consider low-grade chondrosarcoma.
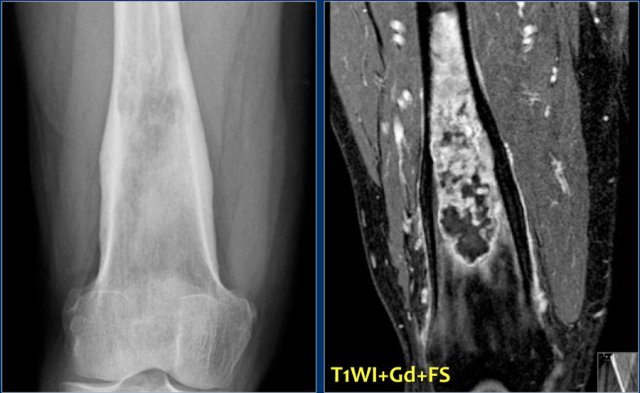
Plain radiograph and coronal T1-weighted contrast-enhanced fat-suppressed MR image of a mixed lytic and sclerotic lesion of the distal femoral diaphysis.
Notice the homogeneous thickening of the cortical bone.
There are no calcifications.
The MR image shows that the lesion has lobulated contours and nodular enhancement.
The homogeneous enhancement in the upper part with edema and cortical thickening are not typical for a low-grade chondrosarcoma.
A high grade chondrosarcoma must be considered in the differential diagnosis.
Biopsy revealed dedifferentiated chondrosarcoma.
Peripheral chondrosarcoma
Key facts
- Accounts for 8% of all chondrosaromas.
- Prevalence of 3-5% in patients with hereditary multiple osteohondromas.
- Development in centrally located osteochondromas like the pelvis, hip and shoulder is most common.
Consider peripheral chondrosaroma in growing osteochondromas with or without pain after closure of the physeal plate.
Radiographic or CT features that suggest malignancy:
- growth of osteohondroma in skeletally mature patients
- irregular or indistinct surface of lesions
- erosion or destruction of adjacent bone
- soft tissue mass with scattered or irregular calcifications
Use MRI with water-sensitive sequence (T2 FS) to determine cartilage cap thickness.
Consider progression of osteohondroma to chondrosarcoma when cartilage cap measures > 10 mm.
Click here for more examples of chondrosarcoma.
Periosteal or juxtacortical chondrosarcoma
A juxtacortical chondrosarcoma has be considered in the differential diagnosis when a mineralized lesion adjacent to the cortical bone is seen.
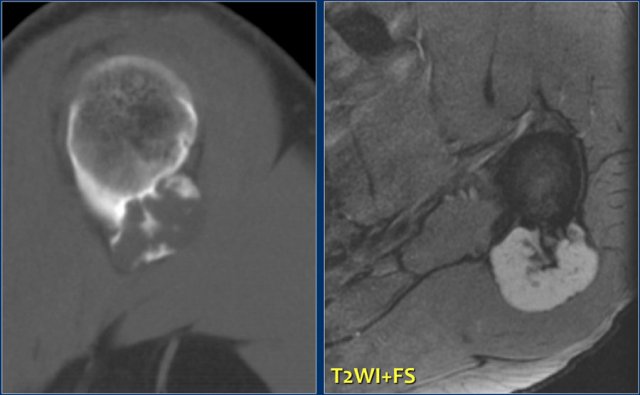
Here a partially calcified mass against the proximal humerus with involvement of the cortical bone on an axial CT image.
T2-weighted MR image reveals a lobulated mass with high signal intensity.
The bone marrow compartment is not involved which is important for the surgical strategy.
A periosteal chondroma may have the same imaging characteristics, however, these are almost always much smaller.
Plain radiograph in another patient shows irreglar mineralized lesion with elevation of the periosteum and cortical involvement. On the right T2-WI with FS of same patient.. The juxtacortical mass has a high SI and lobulated contours. DD: juxtacortical chondrosarcoma, parosteal osteosarcoma.
Enchondroma
Most commonly encountered bone tumor in the small bones of the hand and foot.
Here on a radiograph the typical calcifications in the chondroid matrix of an enchondroma.
Notice how easily MRI depicts these lesions.
Enchondroma is a fairly common benign cartilaginaous lesion which may present as an entirely lytic lesion without any calcification, as a dense calcified lesion or as a mixed leson with osteolysis and calcifications.
Enchondromas aswell as low-grade chondrosarcomas are frequently encountered as coincidental findings in patients who have a MRI or bone scan for other reasons.
Click here for more examples of enchondromas.
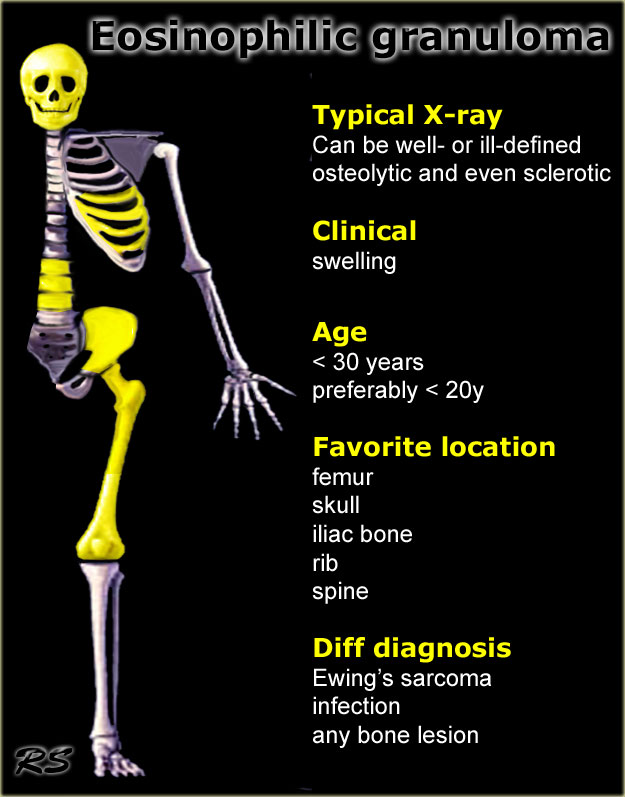
Eosinophilic granuloma
key facts:
- Typically presents as a lytic lesion in a flat bone, vertebra or diaphysis of long bone.
- May show extinction and become sclerotic and indolent,.
- MR usually shows a large amount of reactive changes in bone and soft tissue.
- In the active phase there is multilaminar periosteal reaction and bone and soft tissue edema.
- Eosinophilic granuloma like osteomyelitis, can be a serious mimicker of malignancy (particularly Ewing sarcoma).
- Should be included in the differential diagnosis of young patient with multiple lucent lesions (Langerhans cell histiocytosis).
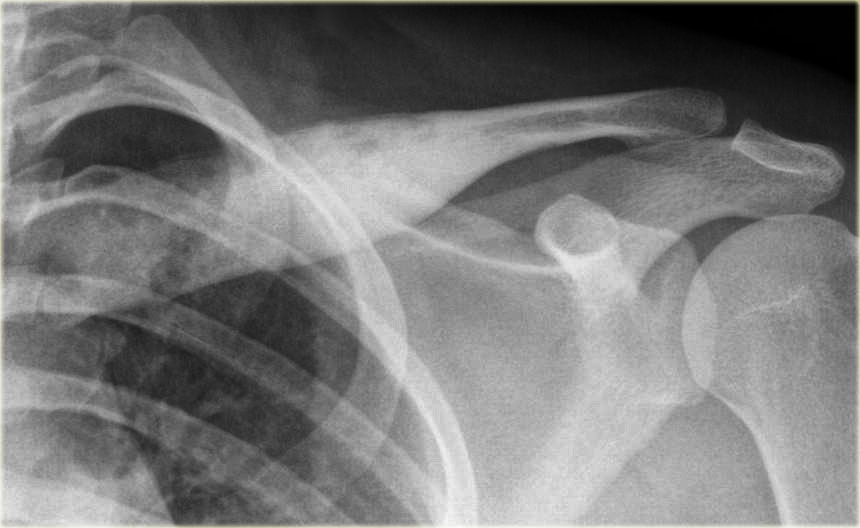
This image is of a 20 year old patient with a sclerotic expansile lesion in the clavicle.
Notice that there are small areas of ill-defined osteolysis.
In an older patient one should first consider an osteoblastic metastasis.
If the patient had fever and a proper clinical setting, osteomyelitis would be in the differential diagnosis.
Click here for more examples of eosinophilic granuloma.
Fibrous dysplasia
FD is often purely lytic, but may have a groundglass appearance as the matrix calcifies.
Ossifications or calcifications can be present in variable amounts.
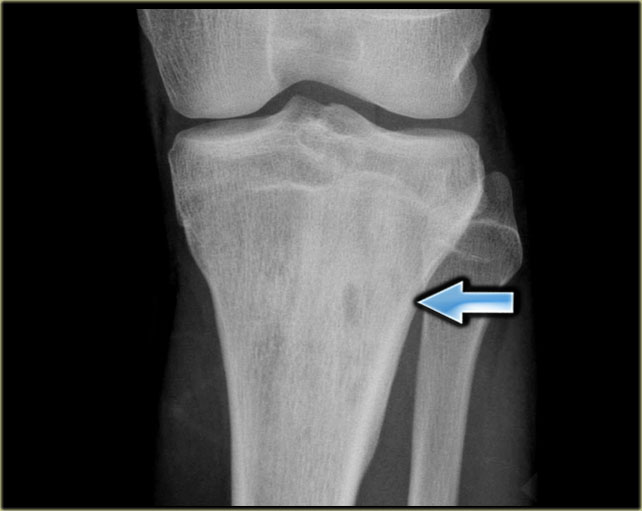
Here a rather wel-defined eccentric lesion which is predominantly sclerotic.
The differential diagnosis includes:
- Fibro-osseous lesion like fibrous dysplasia.
- Non-ossifying fibroma which has been filled in.
- Adamantinoma in case of a sclerotic lesion with several lucencies of the tibia in a young patient.
Here a well-defined mixed sclerotic-lytic lesion of the left iliac bone.
The diagnosis was fibrous dysplasia.
DD: old SBC.
Bone scintigraphy can be either negative or show limited uptake.
The signal intensity on MR depends on the amount of calcifications and ossifications and fibrous tissue (low SI) and cystic components (high SI on T2).
Fibrous dysplasia can be monostotic or polyostotic.
Usually it is a lesion of childhood or young adults. Not infrequently encountered as coincidental finding at later age.
Central location most common with some expansion and cortical thinning
Click here for more detailed information about fibrous dysplasia.
Melorrheostosis
Melorrheostosis is a dysplasia of the bone, characterized by apposition of mature bone on the outer or inner surface of cortical bone.
Usually one bone is involved.
The epiphysis, metaphysis and diaphysis may be involved.
Usually new bone is added to one side of the cortex only.
Complete envelopment may occur.
Here Melorrheostosis of the ulna with the appearance of candle wax.
A surface osteosarcoma could be considered in the differential diagnosis
Axial T1-weighted MR image shows homogeneous low signal intensity due to the compact bone apposition.
Click here for more examples.
Metastases
key facts
- Sclerotic osteoblastic metastases must be included in the differential diagnosis of any sclerotic bone lesion in a patient > 40 years.
- Most commonly originate from prostate and breast cancer and less frequently from lung cancer, lymphoma or carcinoid.
- In breast cancer, metastases may present as lytic lesions that may become sclerotic expressing a favourable response to chemotherapy.
Here images of a patient with prostate cancer.
Notice the numerous predominantly osteoblastic metastases.
Here images of a patient with breast cancer.
There is a metastasis, which presents as a subtle sclerotic lesion in the humerus metaphysis.
This could be an osteoblastic metastasis or an osteolytic metastasis that responded to chemotherapy.
Osteoblastic metastases (2)
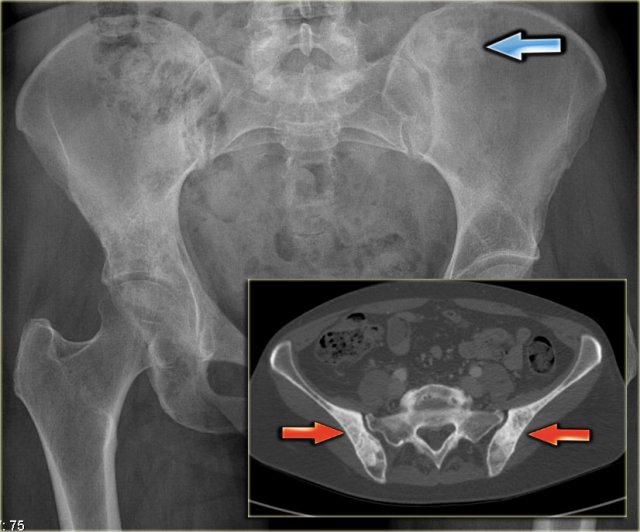
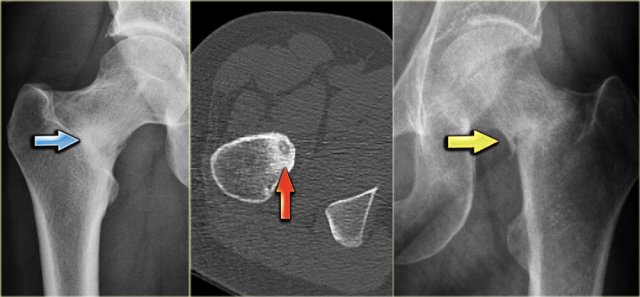
Here a radiograph of the pelvis with a barely visible osteoblastic metastasis in the left iliac bone (blue arrow).
Notice that CT depicts these lesions far better (red arrows).
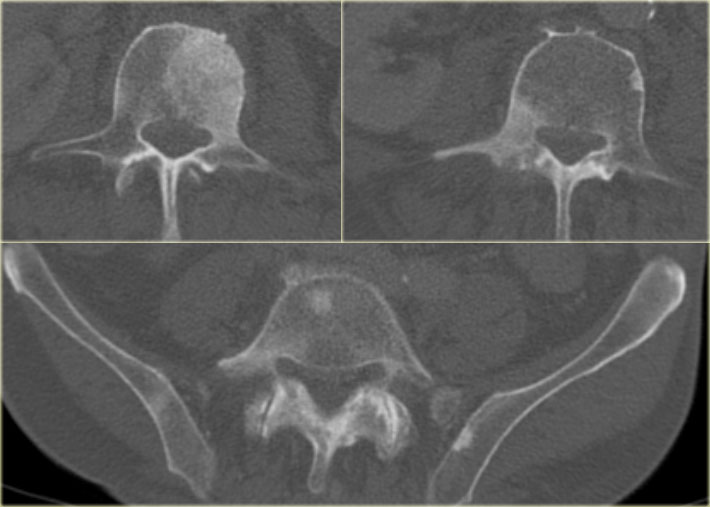
Here CT-images of a patient with prostate cancer.
Notice the numerous ill-defined osteoblastic metastases.
Non-ossifying fibroma
Non-ossifying fibroma (NOF) can be encoutered occasionally as a partial or completely sclerotic lesion.
Typically a NOF presents as an eccentric well-defined lytic lesion, usually found as a coincidental finding.
These lesions usually regress spontaneously and may then become sclerotic.
Other benign lesions, like solitary bone cyst, fibrous dysplasia, chondroblastoma and other benign bone tumors may become inert and may also become sclerotic.
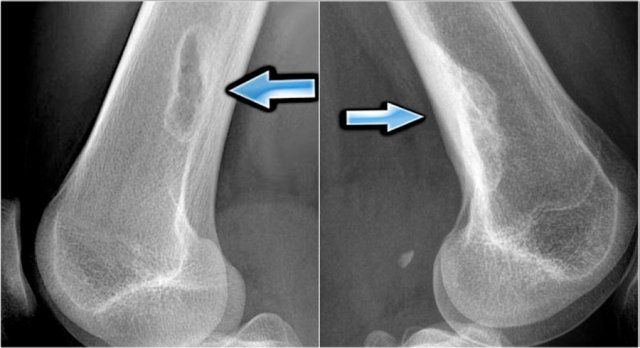
The images show on the left a typical osteolytic NOF with a sharp sclerotic border.
The image on the right is of a different patient who has an old NOF that shows complete fill in.
Click here for more detailed information about NOF.
Here an incidental finding of several eccentric sclerotic lesions of the distal femur.
These are inert filled-in non-ossifying fibromas.
No further examination is needed.
Osteochondroma
Osteochondroma is a bony protrusion covered by a cartilaginous cap.
Growth of the osteochondroma takes place in the cap, corresponding with normal enchondral growth at the growth plates.
Accordingly, growth of osteochondromas is allowed until a patient reaches adulthood and the physeal plates are closed.
Growth of osteochondromas at adult ages, which is characterized by a thick cartilaginous cap (high SI on T2WI) should raise the suspicion of progression to a peripheral chondrosarcoma.
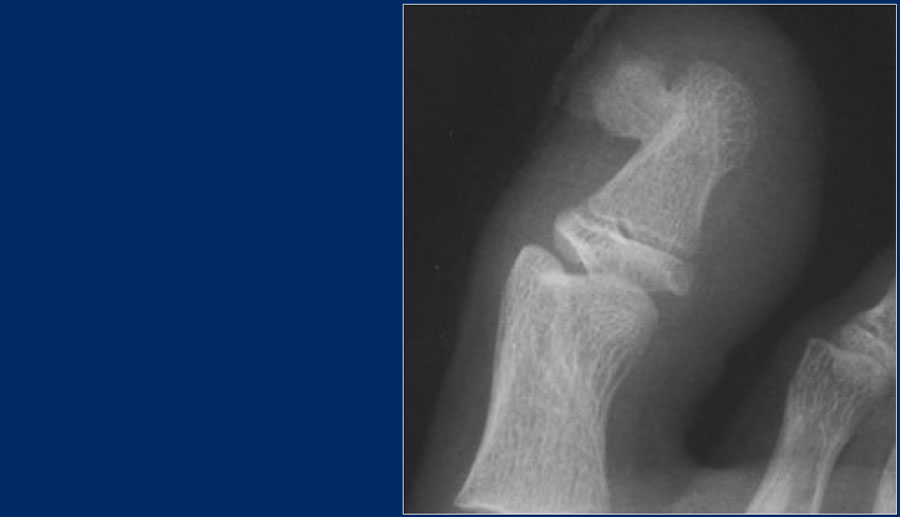
Here a patient with a broad-based osteochondroma.
Notice that the cortical bone extends into the lesion.
This feature differentiates it from a juxtacortical tumor.
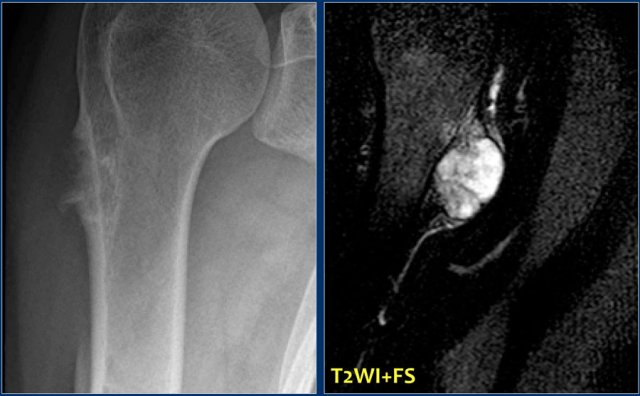
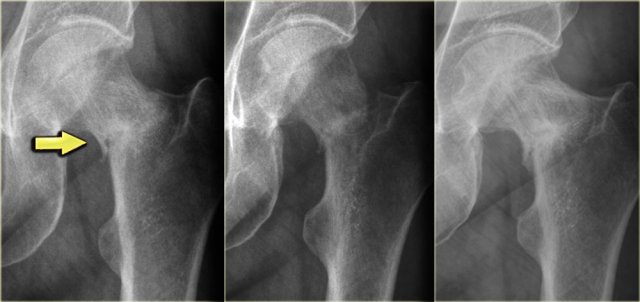
Here a patient with a broad-based osteochondroma with extension of the cortical bone into the stalk of the lesion.
Notice the lytic peripheral part with subtle calcifications.
This part corresponds to a zone of high SI on T2-WI with FS on the right.
This represents a thick cartilage cap.
This is an example of progression of an osteochondroma to a peripheral chondrosarcoma.
Malignant transformation
Radiographic features that should raise the suspicion of malignant transformation on plain radiographs or CT include:
- Growth of osteochondroma in skeletally mature patient
- Irregular or indistinct surface of lesions
- focal lucent regions in interior of lesions
- erosion or destruction of adjacent bone
- presence of soft tissue mass with scattered or irregular calcifications
Osteoid osteoma
key facts:
- Small osteolytic lesion (up to 1.5 cm) with or without central calcification.
- Surrounded by a prominent zone of reactive sclerosis due to a periosteal and endosteal reaction, which may obscure the central nidus.
- In juxta-articular localisation, the reactive sclerosis may be absent.
- Localisation: femur, tibia, hands and feet, spine (arch).
- Axial imaging for differentiation from Brodie abscess, osteoblastoma, stress fracture
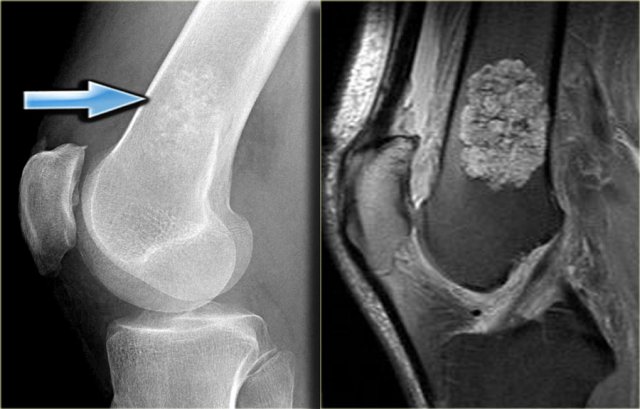
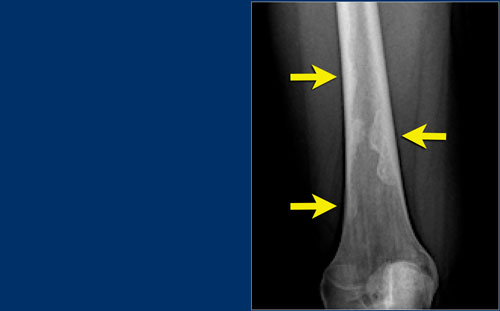
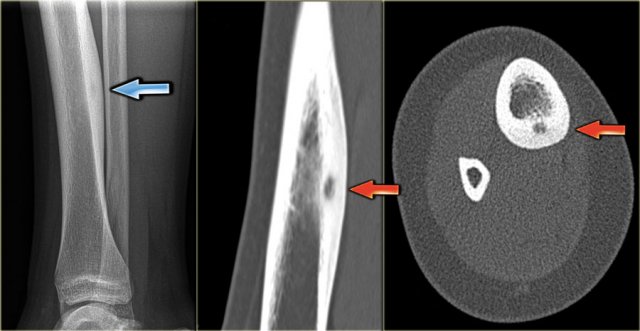
Here the reactive sclerosis is the most obvious finding on the X-ray.
There is reactive sclerosis with a nidus that is barely visible on the radiograph (blue arrow), but clearly visible on the CT (red arrows).
CT scan is usually very helpful in detecting the nidus and differentiating osteoid osteoma from other sclerotic lesions like osteoblastoma, osteomyelitis, arthritis, stress fracture and enostosis.
MRI also may detect the nidus, combined with abundant bone marrow and soft tissue edema.
Osteoid osteoma (2)
In most cases of osteoid osteoma the radiographic appearance is determined by the reactive sclerosis.
In some cases however the osteolytic nidus can be visible on the radiograph (figure).
Osteoma
key facts
Osteoma consists of densely compact bone.
It is most commonly located in the outer table of the neurocranium or in a paranasal sinus.
Osteomyelitis
Osteomyelitis is a mimicker of various benign and malignant bone tumors and reactive processes that may be accompanied by reactive sclerosis.
Acute osteomyelitis is characterised by osteolysis.
Sclerosis is usually the most prominent finding in subacute and chronic osteomyelitis.
A periosteal reaction with or without layering may be present.
Sometimes a more solid periosteal reaction is present combined with cortical thickening and broadening of the bone.
Here an image of a patient with chronic osteomyelitis.
Centrally there is an ill-defined osteolytic area.
The major part of the lesion consists of reactive sclerosis.
Osteosarcoma
Key facts
- 2nd most common primary bone tumor and highly malignant.
- 50% around the knee.
- Presentation: pain, mass, pathologic fracture.
- Sclerosis is present from either tumor new bone formation or reactive sclerosis.
- Age: most commonly seen in 10-25 years, but may occur in older patients.
- Plain films typically reveal lesions with moth-eaten or permeative pattern of the transition zone with irregular cortical destruction and an interrupted periosteal reaction with soft tissue extension.
- A periosteal reaction known as Codman's triangle appears as tumor elevates periosteum from underlying bone. Cortical soft tissue extension may produce radiating spicules of bone called sunray appearance.
Osteosarcoma (2)
Here images of an osteosarcoma in the right femur.
It is barely visible within the bone, but an agressive periostitis is seen (arrow).
Continue with the MR-images.
The sagittal T1WI and Gd-enhanced T1W-image with fatsat show a large tumor mass infiltrating a large portion of the distal femur and extending through the cortex into the soft tissues.
Parosteal osteosarcoma
Parosteal osteosarcoma is a sarcoma that has it's origin on the surface of the bone.
It grows primarily into the surrounding soft tissues, but may also infiltrate into the bone marrow.
It is nost commonly located on the posterior side of the distal meta-diaphysis of the femur.
Ossification in parosteal osteosaroma is usually more mature in the center than at the periphery. This is opposed to myositis ossificans which may present very close to the cortical bone, but maturation develops from the center to the periphery.
Paget's disease of bone
Paget disease is a chronic disorder of unknown origin with increased breakdown of bone and formation of disorganized new bone.
The most common appearance is the mixed lytic-sclerotic.
In this case we see the pathognomonic triad of bone expansion, cortical thickening and trabecular bone thickening in the mixed lytic and sclerotic phase of Paget's disease of right hemipelvis.
Reactive processes
Myositis ossificans
Here a patient with a mineralized mass in the soft tissues.
Notice that the mineralization is predominantly in the periphery of the mass and that there is a lucent zone between the mass and the cortical bone.
Contrast-enhanced T1-weighted MR image demonstrates heterogeneous enhancement of the mass with extensive surrounding edema.
This is consistent with the diagnosis of a reactive process like myositis ossificans.
Stress fractures
Stress fractures occur in normal (fatigue fractures) or metabolically weakened (insufficiency fractures) bones.
Usually stress fractures are easy to recognize.
Uncommonly it can be difficult to differentiate a stress fracture from a pathologic fracture, that occurs at the site of a bone tumor.
Uncommonly it can be difficult to differentiate a stress fracture from a bone tumor like an osteoid osteoma or from a pathologic fracture, that occurs at the site of a bone tumor.
Here an example of a patient with a stress fracture of the distal fibula.
Coronal MR image demonstrates subtle low intensity line representing the fracture.
Differential diagnosis based on the periosteal reaction and the extensive edema:
- Osteomyelitis
- Eosinophilic granuloma
Posttraumatic calcifications
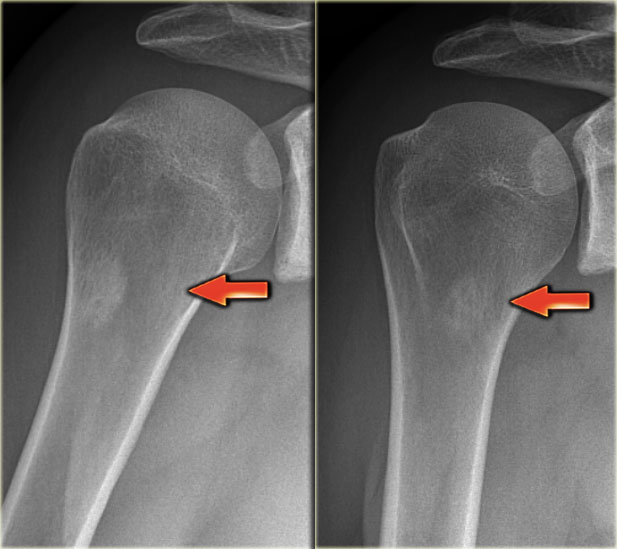
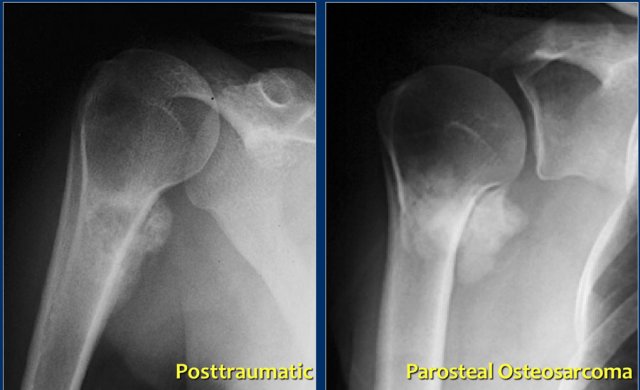
Here a patient with a juxtacortical sclerotic mass of the proximal humerus (left).
This proved to be a reactive calcification secondary to trauma.
Notice the resemblance to a juxtacortical mass in another patient (right), which was a biopsy proven parosteal osteosarcoma.
This shows that differentiating a tumor from a reactive proces scan be quite difficult in some cases.
When a reactive process is more likely based on history and imaging features, follow-up is sometimes still needed.
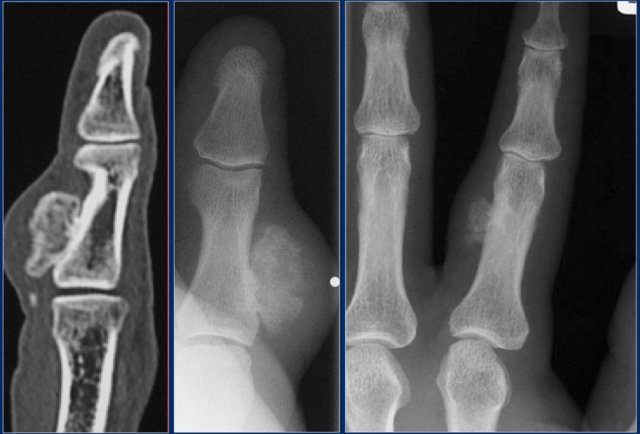
Subungual exostoses
Subungual exostoses are bony projections which arise from the dorsal surface of the distal phalanx, most commonly of the hallux.
These lesions are not osteochondromas, but consist of reactive cartilage metaplasia.
The radiographic appearance and location are typical.
Nora's lesion
Here two patients with a bizar parosteal osteochondromatous proliferation (BPOP), also called Nora's lesion.
This benign reactive process is most commonly found adjacent to the cortex of phalanges of hands or feet (75%).
The cortical bone and bone marrow compartment are not involved.
Rapid growth of the mineralized mass is not uncommon.
Charity
All the profits of the Radiology Assistant go to Medical Action Myanmar which is run by Dr. Nini Tun and Dr. Frank Smithuis sr, who is a professor at Oxford university and happens to be the brother of Robin Smithuis.
Click here or on the image below to watch the video of Medical Action Myanmar and if you like the Radiology Assistant, please support Medical Action Myanmar with a small gift.