Osteolytic - well defined bone tumors
Henk Jan van der Woude and Robin Smithuis
Radiology department of the Onze Lieve Vrouwe Gasthuis, Amsterdam and the Rijnland hospital, Leiderdorp, the Netherlands
Publicationdate
In the article Bone Tumors - Differential diagnosis we discuss a systematic approach to the differential diagnosis of bone tumors and tumor-like lesions.
In this article we will discuss the differential diagnosis of well-defined osteolytic bone tumors and tumor-like lesions.
Abbreviations used:
- ABC = Aneurysmal bone cyst
- CMF = Chondromyxoid fibroma
- EG = Eosinophilic Granuloma
- GCT = Giant cell tumour
- FD = Fibrous dysplasia
- HPT = Hyperparathyroidism with Brown tumor
- NOF = Non Ossifying Fibroma
- SBC = Simple Bone Cyst
Introduction
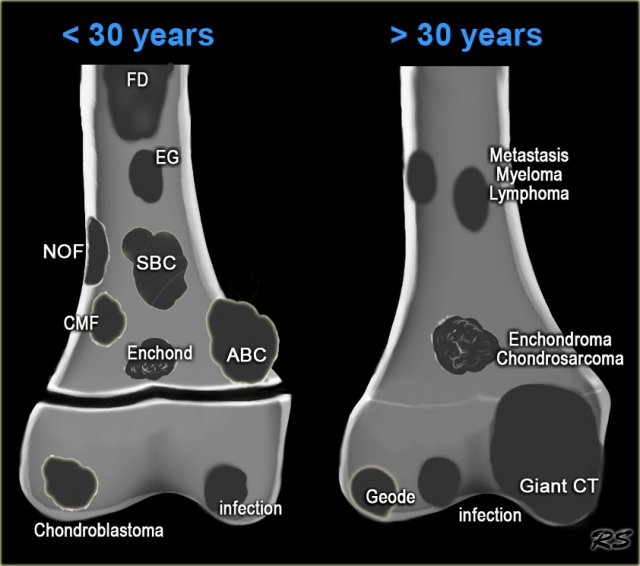
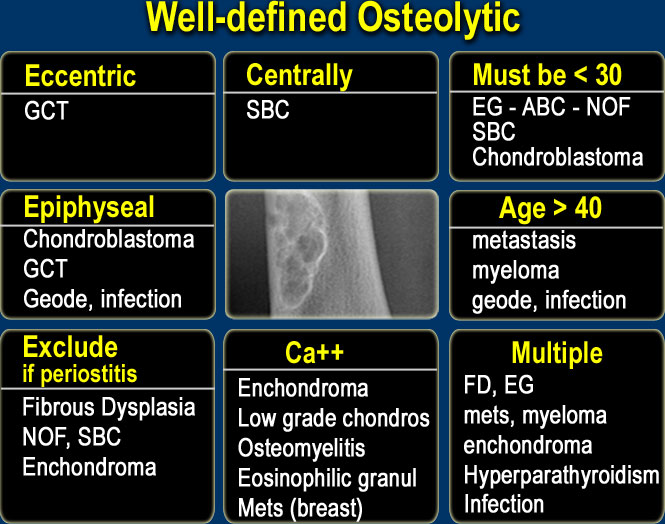
On the left the most common well-defined bone tumors and tumor-like lesions.
These lesions are sometimes referred to as benign cystic lesions, which is a misnomer since most of them are not cystic, except for SBC and ABC.
It is true that in patients under 30 years a well-defined border means that we are dealing with a benign lesion, but in patients over 40 years metastases and multiple myeloma have to be included in the differential diagnosis.
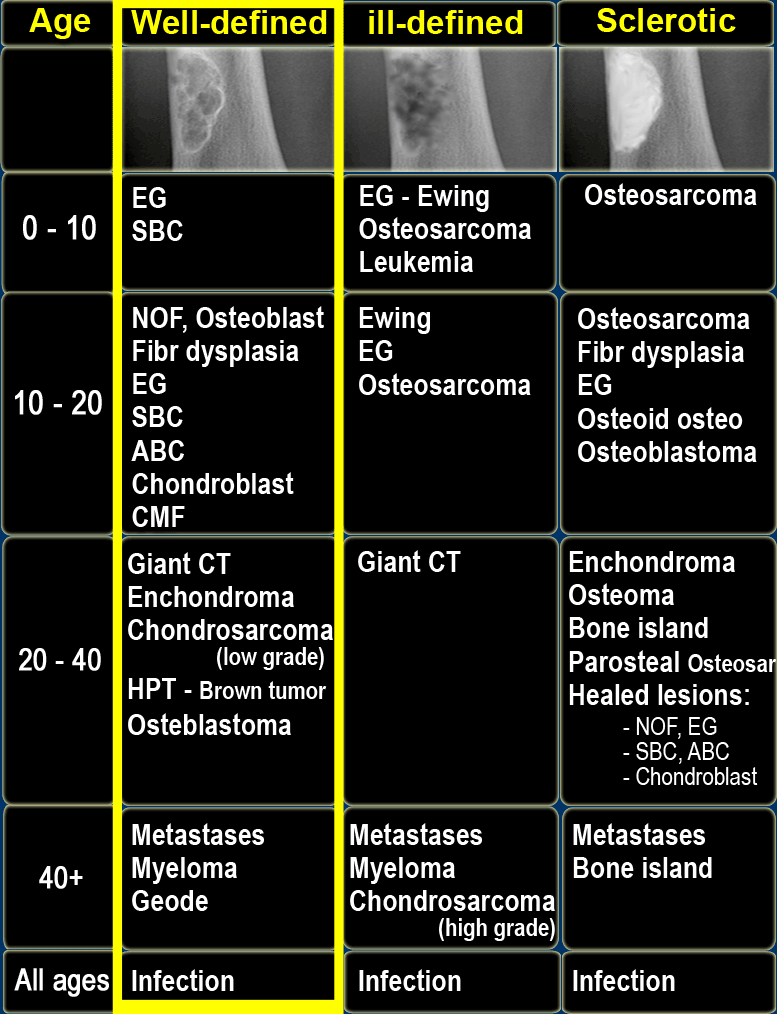
On the left a table with well-defined osteolytic bone tumors and tumor-like lesions in different age-groups.
Notice the following:
- In patients In patients > 40 years metastases and multiple myeloma are by far the most common well-defined osteolytic bone tumors.
- Patients with Brown tumor in hyperparathyroidism should have other signs of HPT or be on dialysis.
- Differentiation between a benign enchondroma and a low grade chondrosarcoma can be impossible based on imaging findings only.
- Infection is seen in all ages.
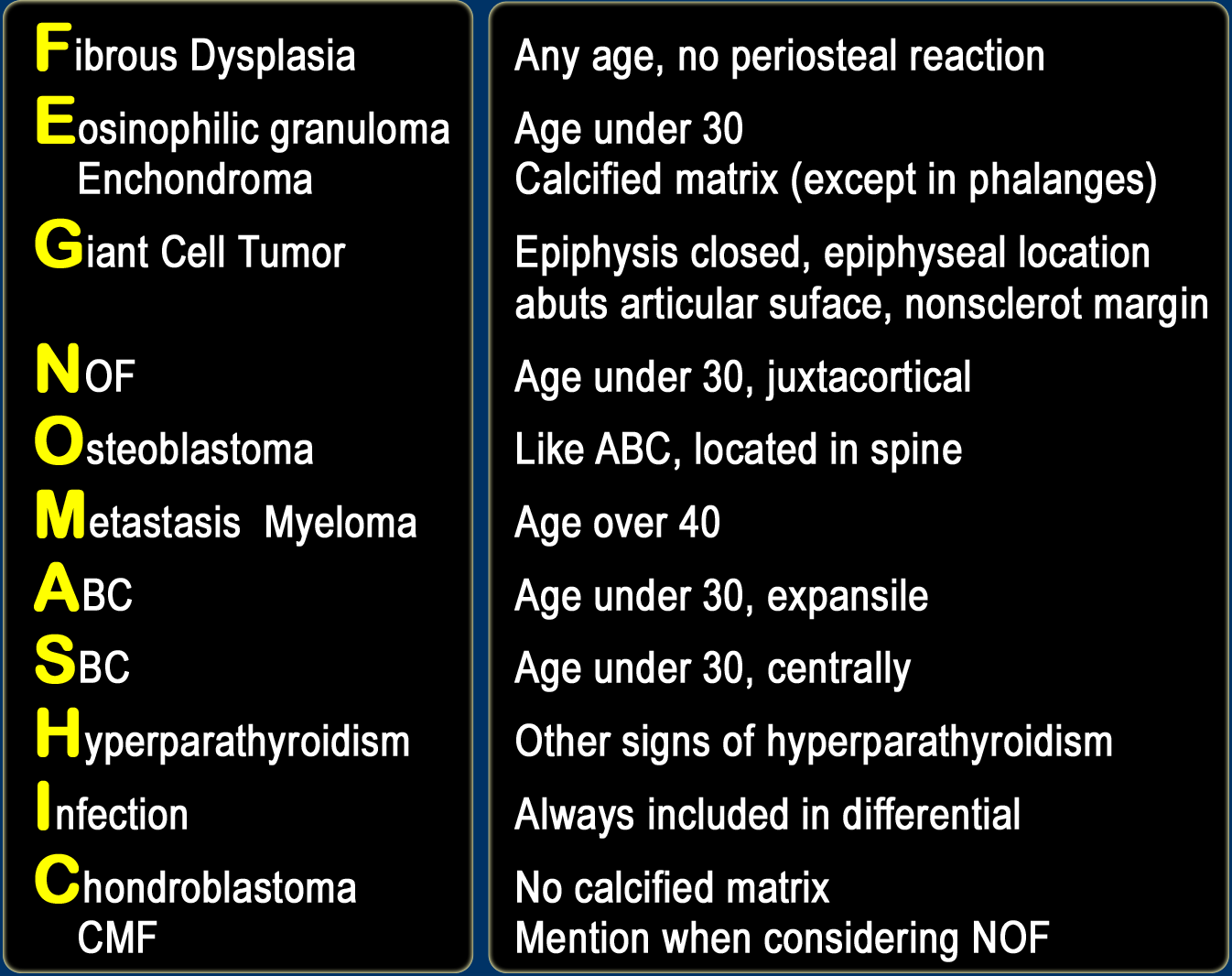
Fegnomashic
Most bone tumors present as well-defined osteolytic lesions, sometimes referred to as 'bubbly lesions'.
It is important to have a good differential diagnostic approach to these lesions.
You can use the table above, but another way to look at the differential diagnosis of well defined osteolytic bone lesions is to use the mnemonic Fegnomashic, which is popularized by Clyde Helms (1).
Some prefer to use the mnemonic Fogmachines, which is formed by the same letters, but is a real word.
 Fibrous dysplasia: various presentations with or without sclerotic margin, with groundglass appearance, with calcifications or ossifications
Fibrous dysplasia: various presentations with or without sclerotic margin, with groundglass appearance, with calcifications or ossifications
Fibrous dysplasia
Fibrous dysplasia is a benign disorder characterized by tumor-like proliferation of fibro-osseus tissue and can look like anything.
FD most commonly presents as a long lesion in a long bone.
FD is often purely lytic and takes on ground-glass look as the matrix calcifies.
In many cases there is bone expansion and bone deformity.
The ipsilateral proximal femur is invariably affected when the pelvis is involved.
When FD in the tibia is considered, adamantinoma should be in the differential diagnosis.
Discriminator:
- If periosteal reaction or pain is present, exclude fibrous dysplasia, unless there is a fracture.
Enchondroma
Enchondroma is a benign cartilage tumor.
Frequently it is a coincidental finding.
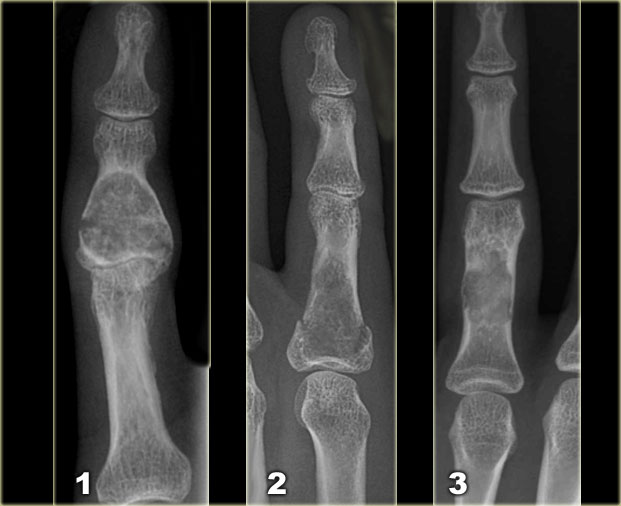
In the phalanges of the hand it frequently presents with a fracture.
It is the most common lesion in the phalanges, i.e. a well-defined lytic lesion in the hand is almost always an enchondroma.
In some locations it can be difficult to differentiate between enchondroma and bone infarct.
It is almost impossible to differentiate between enchondroma and low grade chondrosarcoma based on radiographic features alone.
Ollier's disease is multiple enchondromas.
Maffucci's syndrome is multiple enchondromas with soft tissue hemangiomas.
Features that favor the diagnosis of a low-grade chondrosarcoma:
- Higher age
- Size > 5 cm
- Activity on bone scan
- Fast enhancement on dynamic contrast enhanced MR series
- Endosteal scalloping of the cortical bone
Discriminators :
- Must have calcification except in phalanges.
- No periostitis.
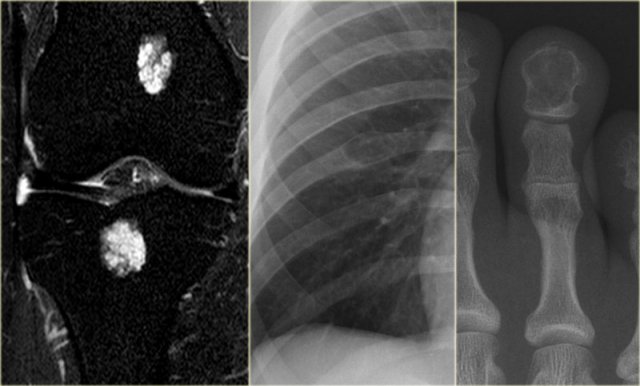
- left
Fat suppressed coronal PD-image of the knee. Typical enchondromas in the femur and tibia as seen frequently as coincidental finding in MR-examinations. - middle
Well-defined lytic lesion in the rib with cortical thinning. - right
Well-defined lytic lesion with a sclerotic margin and without calcifications in the end phalanx.
Eosinophilic granuloma
EG is a non-neoplastic proliferation of histiocytes and is also known as Langerhans cell histiocytosis.
It should be included in the differential diagnosis of any sclerotic or osteolytic lesion, either well-defined or ill-defined, in patients under the age of 30.
The diagnosis EG can be excluded in age > 30.
EG is usually monostotic, but can be polyostotic.
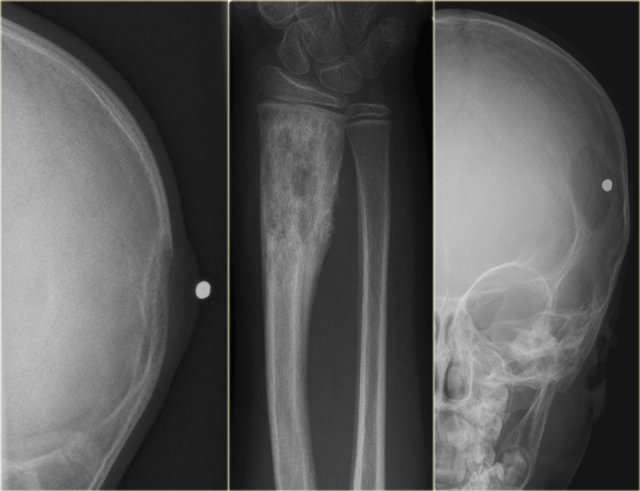
- left
Osteolytic lesion arising from the neurocranium with associated soft tissue swelling. - middle
Mixed lytic-sclerotic lesion, not well-defined with solid periosteal reaction. - right
Sharply defined osteolytic lesion of the skull. There is no 'button sequestrum', which is more or less pathognomonic.
Discriminator:
- Must be under age 30.
Giant cell tumor
Giant cell tumor is a lesion with multinucleated giant cells.
In most cases it is a benign lesion.
Malignant GCT is rare and differentiation between benign or malignant GCT is not possible based on the radiographs.
GCT is also included in the differential diagnosis of an ill-defined osteolytic lesion, provided the age and the site of the lesion are compatible.
Discriminators:
- Epiphyses must be closed.
- Must be an epiphyseal lesion and abut the articular surface.
- Must be well-defined and non-sclerotic margin.
- Must be eccentric.
 NOF: typical presentation as an eccentric, multi-loculated subcortical lesion with a central lucency and a scalloped sclerotic margin.
NOF: typical presentation as an eccentric, multi-loculated subcortical lesion with a central lucency and a scalloped sclerotic margin.
NOF
NOF is a benign well-defined, solitary lesion due to proliferation of fibrous tissue.
It is the most common bone lesion.
NOF is frequently a coincidental finding with or without a fracture.
NOF usually has a sclerotic border and can be expansile.
They regress spontaneously with gradual fill in.
NOF may occur as a multifocal lesion.
The radiographic appearance is almost always typical, and as such additional imaging and biopsy is not warranted.
Discriminators:
- Must be under age 30.
- No periostitis or pain.
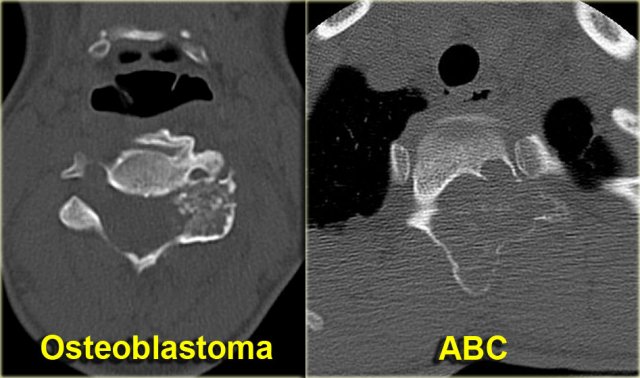
Osteoblastoma
Osteoblastoma is a rare solitary, benign tumor that produces osteoid and bone.
Consider osteoblastoma when ABC is in the differential diagnosis of a spine lesion (figure).
A typical osteoblastoma is larger than 2 cm, otherwise it completely resembles osteoid osteoma.
Discriminator:
- Mention when ABC is mentioned.
Metastases
Metastases are the most common malignant bone tumors.
Metastases must be included in the differential diagnosis of any bone lesion, whether well-defined or ill-defined osteolytic or sclerotic in age > 40.
Bone metastases have a predilection for hematopoietic marrow sites: spine, pelvis, ribs, cranium and proximal long bones: femur, humerus.
Metastases can be included in the differential diagnosis if a younger patient is known to have a malignancy, like neuroblastoma, rhabdomyosarcoma, retinoblastoma.
Most common osteolytic metastases: kidney, lung, colon and melanoma.
Most common osteosclerotic metastases: prostate and breast.
Discriminator:
- Must be over age 40.
Multiple Myeloma
Multiple myeloma must be included in the differential diagnosis of any lytic bone lesion, whether well-defined or ill-defined in age > 40.
The most common location is in the axial skeleton (spine, skull, pelvis and ribs) and in the diaphysis of long bones (femur and humerus).
Most common presentation: multiple lytic 'punched out' lesions.
Multiple myeloma does not show any uptake on bone scan.
Discriminator:
- Must be over age 40.
Multiple Myeloma (2)
Differential diagnosis:
- multiple lesions: metastases.
- solitary lesion: chondrotumor, GCT and lymphoma.
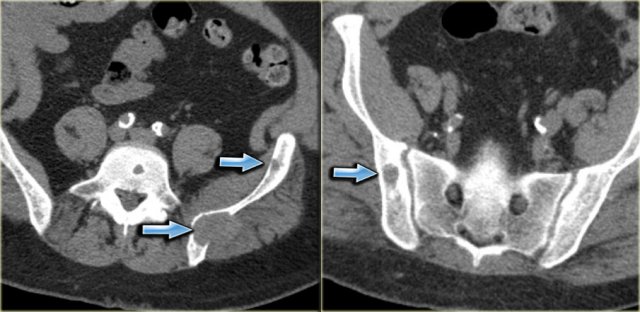
On the left a CT-image of a patient with multiple myeloma.
Notice the numerous osteolytic lesions and permeative cortical destruction pattern.
In the left sacral wing there is a larger lesion with a high density due to replacement of fatty bone marrow by myeloma (red arrow).
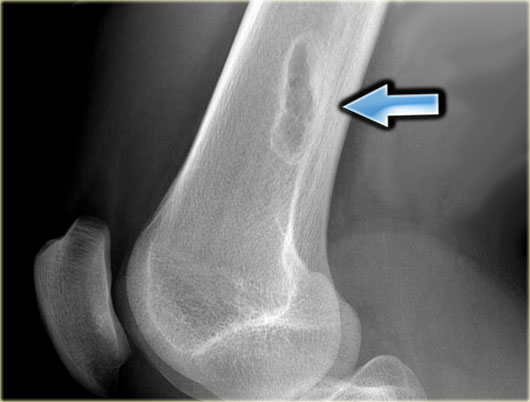
 ABC of the proximal fibula: well-defined, expansile osteolytic lesion with thin peripheral bone shell
ABC of the proximal fibula: well-defined, expansile osteolytic lesion with thin peripheral bone shell
Aneurysmal Bone Cyst
ABC is a solitary expansile well-defined osteolytic bone lesion, that is filled with blood.
It is named aneurysmal because it is expansile.
ABC is thought to be the result of a reactive process secondary to trauma or increased venous pressure.
Sometimes an underlying lesion like GCT, osteoblastoma or chondroblastoma can be found.
ABC can occur almost anywhere in the skeleton.
Discriminators:
- Must be under age 30.
- Must be expansile
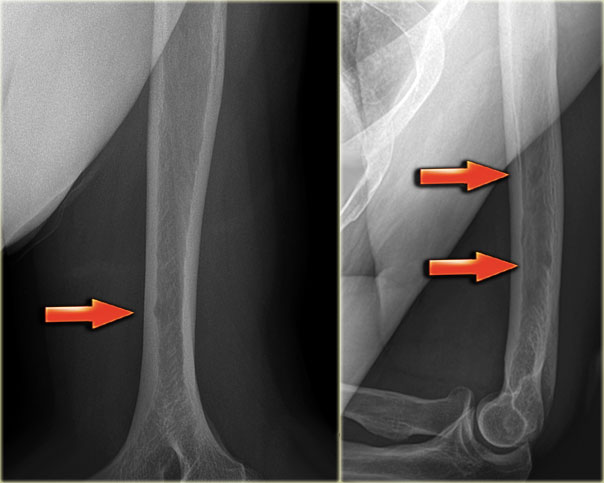
 SBC: well-defined osteolytic lesion without expansion of the proximal meta-diaphysis of the humerus with pathologic fracture
SBC: well-defined osteolytic lesion without expansion of the proximal meta-diaphysis of the humerus with pathologic fracture
Solitary Bone Cyst
Solitary bone cyst, also known as unicameral bone cyst, is a true cyst.
Many well-defined osteolytic lesions are often called cystic, but this is a misnomer.
SBC frequently presents with a fracture.
Sometimes a fallen fragment is appreciated.
Predilection sites: proximal humerus and femur.
Usually less expansion compared with ABC.
Differential diagnosis: ABC, FD when cystic.
SBC may migrate from metaphysis to diaphysis during growth of the bone.
Discriminators:
- Must be under age 30.
- Must be centric
Hyperparathyroidism
Brown tumors can occur in any bone and present as osteolytic lesions with sharp margins.
Septa and ridges may be seen.
Differential diagnosis: ABC, metastases and GCT depending on location and age.
On the left a patient who had a nefrectomy for renal cell carcinoma and who was on dialysis.
Multiple well-defined osteolytic lesions were found on a follow up CT scan.
The differential diagnosis included metastases and Brown tumors in hyperparathyroidism.
Biopsy revealed Brown tumor.
Discriminators:
- Must have other signs of HPT.
Infection
Infection or osteomyelitis is the great mimicker of bone tumors.
It has a broad spectrum of radiographic features and occurs at any age and has no typical location.
In the chronic stage it can mimic a benign bone tumor (Brodies abscess).
In the acute stage it can mimic a malignant bone tumor with ill-defined margins, cortical destruction and an aggressive type of periostitis.
Only when there is a thick solid periosteal reaction we can recognize the non-malignant underlying process.
Discriminators:
- None.
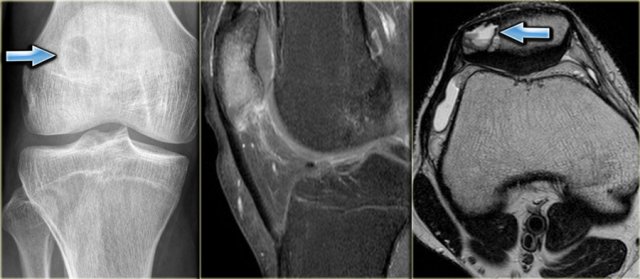
Chondroblastoma
The patella, carpal and tarsal bones can be regarded as epiphysis concerning the differential diagnosis.
On the left a chondroblastoma located in the patella.
Discriminators :
- must be under age 30.
- must be in the epiphysis.
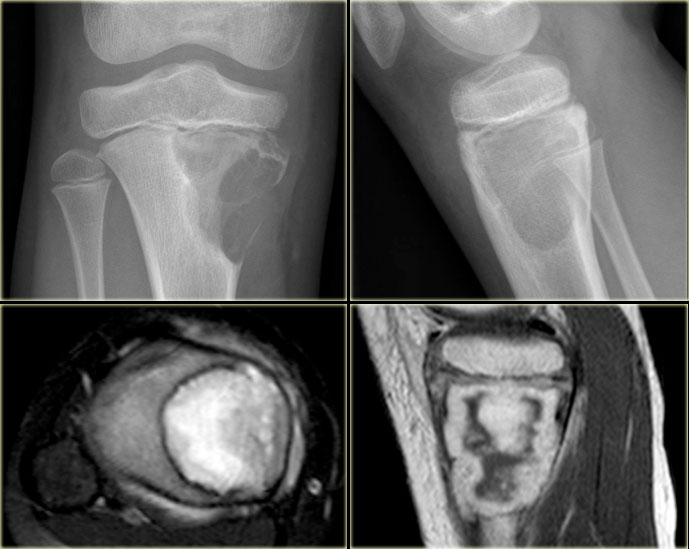
Chondromyxoid Fibroma
Chondromyxoid Fibroma is a rare lesion.
CMF resembles NOF.
Preferential sites: proximal tibia and foot.
Although the name suggests that CMF is a chondroid lesion, calcifications are usually not seen.
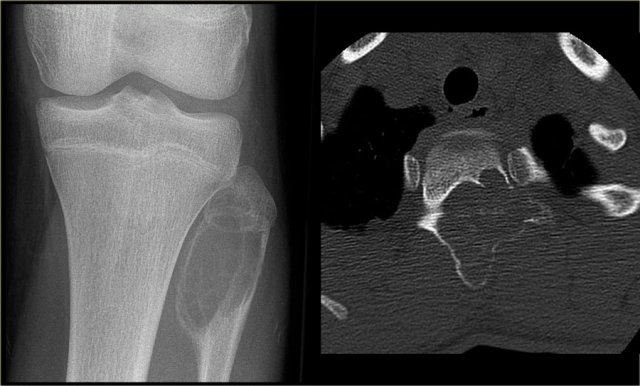
On the left images of a CMF.
There is an eccentric osteolytic lesion in the metaphysis of the proximal tibia.
On the inner side there is a sclerotic margin.
On the outer side there is a regular cortical destruction with peripheral bone layer.
The MR also shows a sclerotic margin with low signal intensity.
Discriminators :
- Mention when an NOF is mentioned.
On the left a summary of things to look for in well-defined osteolytic lesions.
Charity
All the profits of the Radiology Assistant go to Medical Action Myanmar which is run by Dr. Nini Tun and Dr. Frank Smithuis sr, who is a professor at Oxford university and happens to be the brother of Robin Smithuis.
Click here or on the image below to watch the video of Medical Action Myanmar and if you like the Radiology Assistant, please support Medical Action Myanmar with a small gift.