Lumbar Disc Herniation
and other causes of nerve compression
Robin Smithuis
Radiology department of the Rijnland hospital in Leiderdorp, the Netherlands
Publicationdate
In this article a systematic approach to patients with nerve root compression in the lumbar region is presented.
We wil discuss disc herniation, facet arthrosis, synovial cysts, spondylolisthesis and epidural lipomatosis.
The images can be enlarged by clicking on them.
Systematic approach
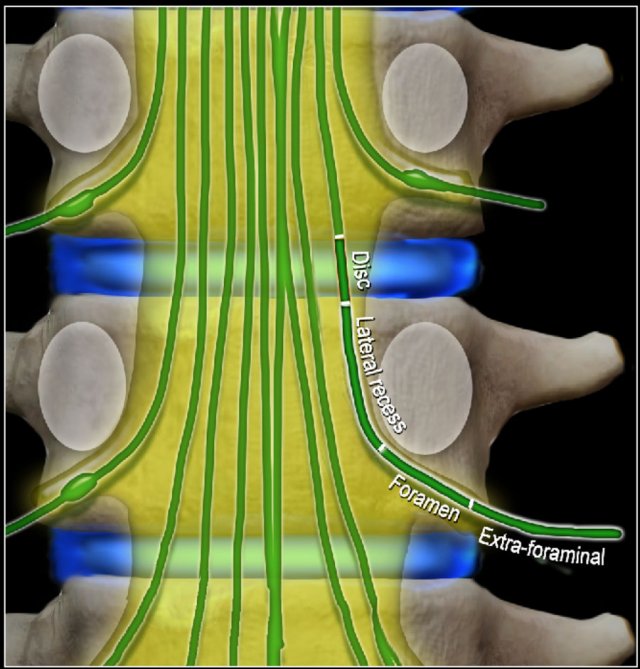
Four levels of nerve compression
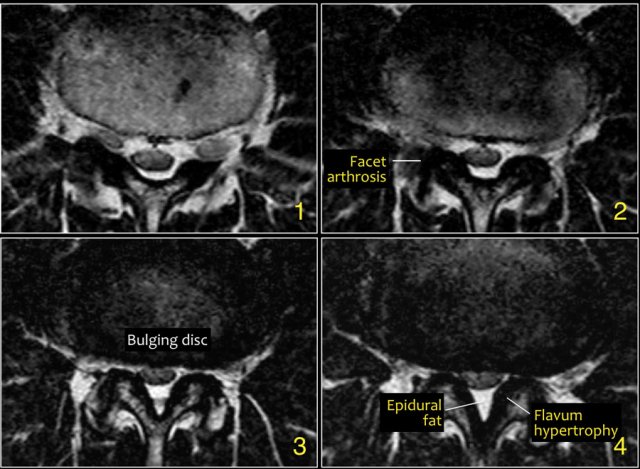
In patients with symptoms of nerve root compression, there are four levels that need to be studied:
- Disc level.
This is the most common area where nerves are compressed.
Mostly by herniated discs and less frequently due to spinal stenosis. - Level of lateral recess.
This is the area below the disc where the nerve runs more laterally towards the foramen.
Narrowing of the lateral recess is caused by facet arthrosis, usually in combination with hypertrophy of the flavum ligament and bulging of the disc. - Foramen.
This is the area between two pedicles, where the nerve leaves the spinal canal.
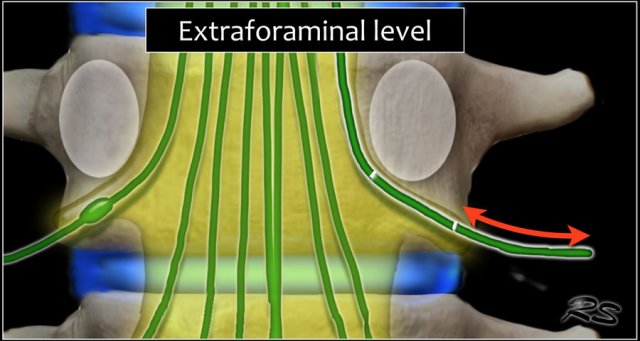
Narrowing of the foramen is seen in facet arthrosis, spondylolisthesis and foraminal disc herniation - usually a migrated disc from a lower level. - Extra-foraminal.
This is the area lateral to the foramen.
Nerve compression in this area is uncommon, but is sometimes caused by a laterally herniated disc.
At these four levels there can be a lot of overlap of pathology.
For instance a herniated disc can cause nerve compression at the level of the disc, but also at the level of the foramen or extra-foraminal when there is migration of the disc.
When you are looking for nerve compression, you have to study all these levels.
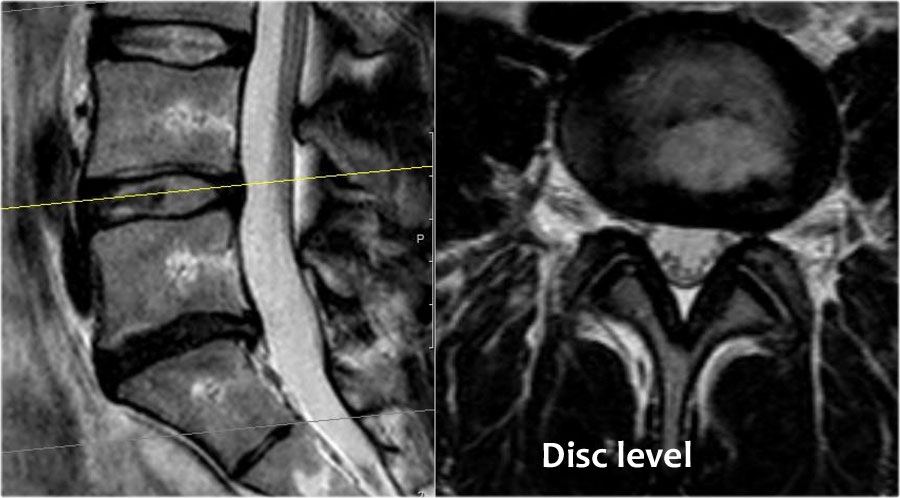
Scroll through the images to see how the nerves run at the level of the disc, lateral recess, foramen and extra-foraminal.
At each level specific pathology can be seen, but there is a lot of overlap.
For instance a disc can herniate and cause nerve compression at the level of the disc, but can also migrate to a lower level and compress the nerve in the lateral recess or move upward and cause compression at the level of the foramen or extra-foraminal.
In patients with facet arthrosis the bony spurs can move medially and narrow the lateral recess or move upward and narrow the foramen.
When there is extreme facet arthrosis bilaterally, it can cause stenosis of the spinal canal and compress all the nerve roots at that level.
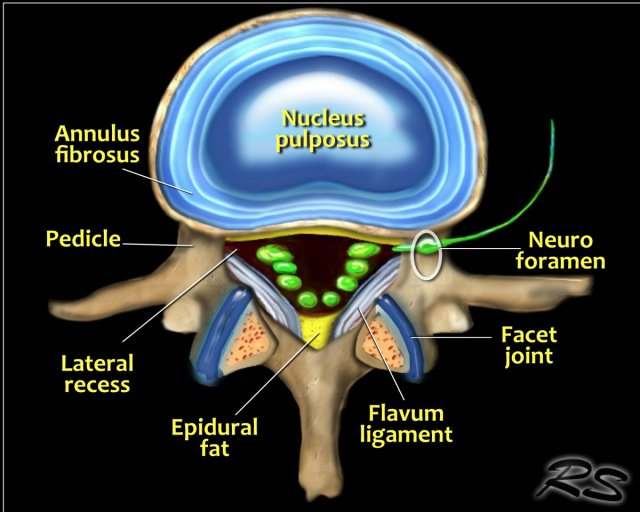
Anatomy
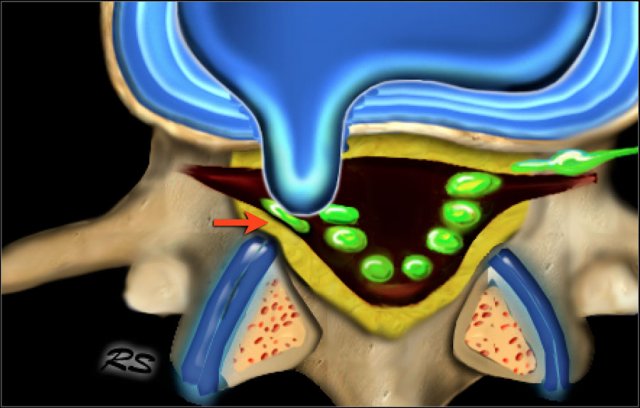
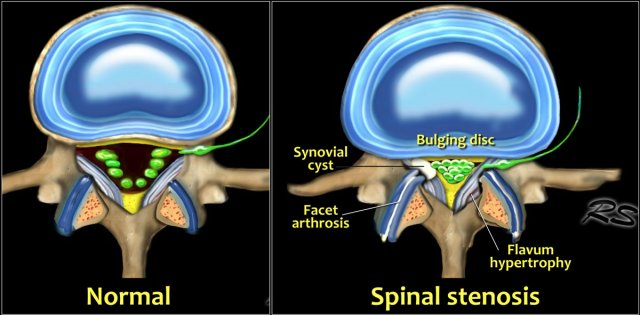
The illustration demonstrates the structures that surround the nerves within the spinal canal.
Flavum ligament
The flavum ligament is a strong ligament on the interior posterior side of the vertebral canal that connects the laminae of adjacent vertebrae.
As a result of aging and instability of the vertebral column due to facet arthrosis there will be more stress on the flavum ligament resulting in hypertrophy and fibrosis.
Hypertrophy of the flavum ligament is usually seen in combination with facet arthrosis and both result in stenosis of the lateral recess or when it is bilateral, in spinal stenosis.
Epidural fat
This is the fat that surrounds the dural sac, that contains the nerves.
Abundant fat can be seen in steroid therapy, extreme obesitas and rarely idiopathic.
Abundant epidural fat can contribute to stenosis of the spinal canal.
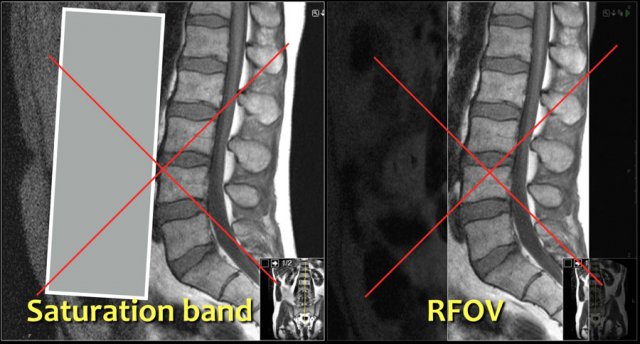
MRI protocol
The MRI protocol for examination of the lumbar spine in patients with symptoms of nerve compression is quite simple.
Basically we rely on the sagittal T1W- and T2W-images and correlate the findings with the transverse T2W-images of the levels of suspected pathology.
Do not use a saturation band on the anterior side or a rectangular field of view (RFOV), because you also want to image the prevertebral soft tissues.
Especially look for an aneurysm of the abdominal aorta, since this may also be the cause of low back pain.
Sometimes it can be difficult to clinically differentiate neurogenic claudication - which is caused by spinal stenosis - from vascular claudication - which is caused by arterial stenosis.
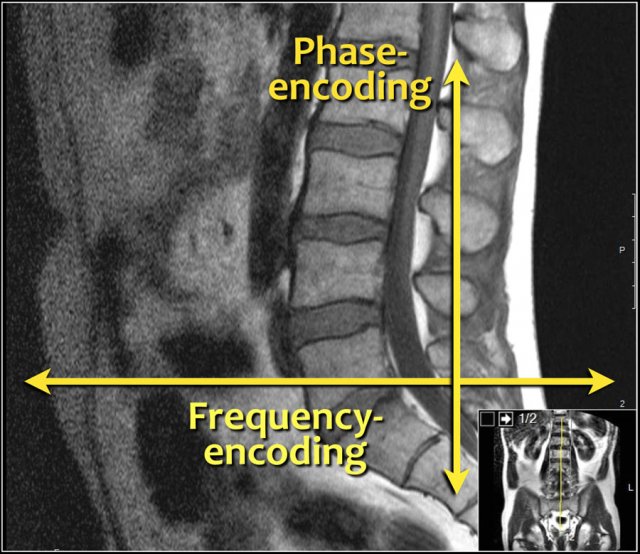
The frequency-encoding should be in the AP-direction and consequently the phase-encoding feet-head.
This has several advantages:
- The resolution is the highest in the frequency-encoded direction.
We want the highest resolution in the AP-direction to look for small herniations and delineation of nerve roots. - When you have the phase encoding in the AP-direction, you get breating artifacts. That is why some use a saturation band or the RFOV.
With the frequency-encoding in the AP-direction you do not have these problems and you do not need a saturation band. - Frequency encoding in the feet-head direction can result in poor deliniation of the vertebral endplates due to chemical shift artifact when the fat in the vertebral body meets the water in the disc.
This is another reason to use a feet-head phase encoding and an AP frequency encoding.
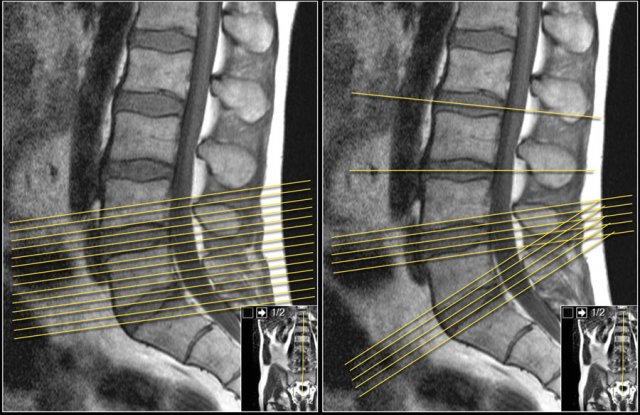
It is better to have continuous slices with the same angulation parallel to the level where nerve compression is suspected.
This has the advantage, that you can follow the involved nerve along the four levels of possible compression.
When you examine multiple levels with different angulation like in the example on the right, you will not be able to follow the whole nerve tract and you will not get the whole picture.
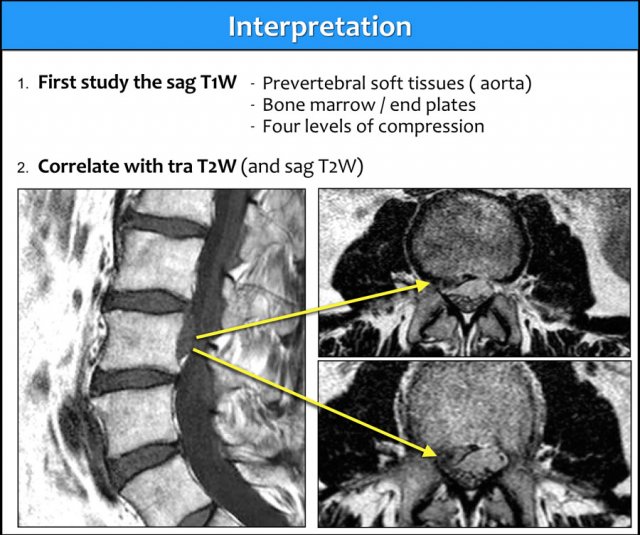
Interpretation
The sagittal T1W-images give you the most diagnostic information.
Before you start looking for any hernias, first take a good look at the prevertebral tissues and bone marrow.
Once you have detected any abnormality, correlate these findings with the T2W-images (figure).
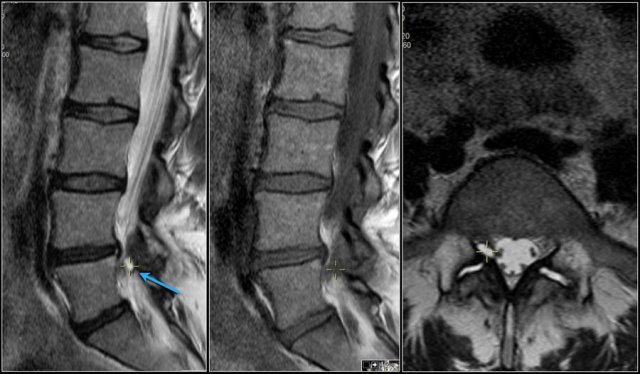
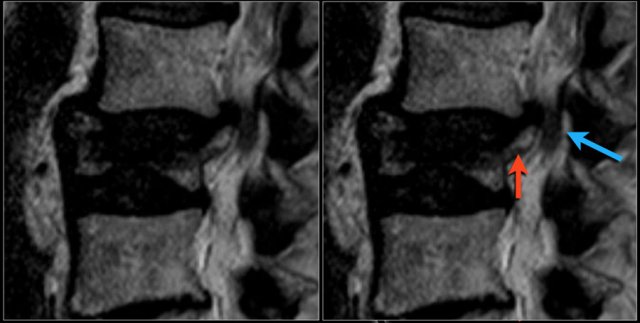
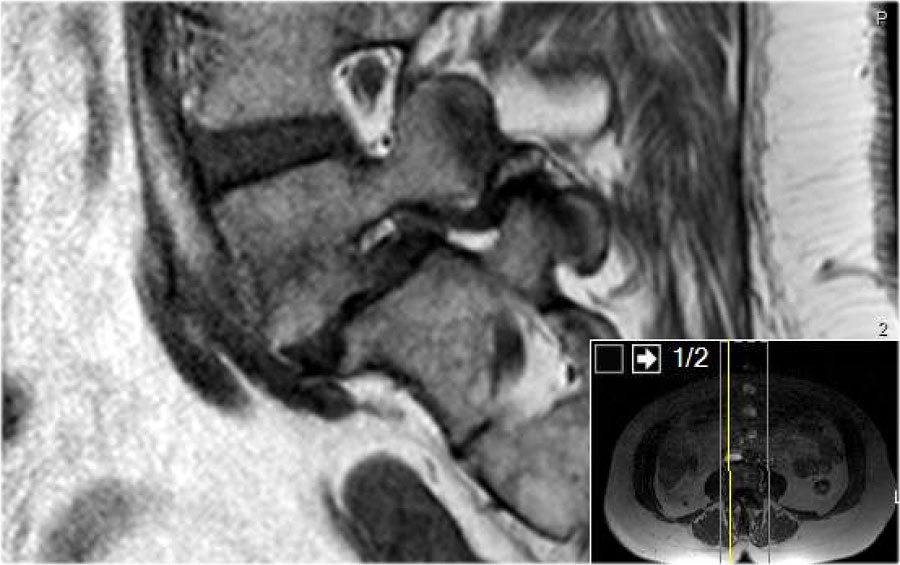
Use of a marker
When you notice an abnormality, it can be helpful to use a marker that correlates with the same location on the other series.
If you enlarge the image, you will see the small yellow cross, which indicates that you are looking at the exact same spot on the other series.
Here the L5 nerve on the right is compressed by a synovial cyst, which is the result of facet arthrosis with effusion within the intervertebral joints.
Prevertebral tissues
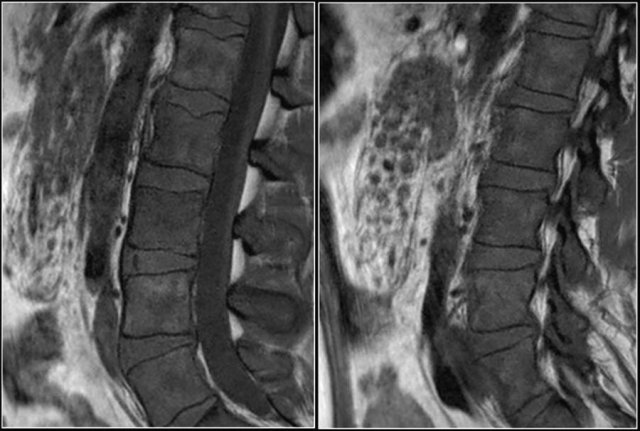
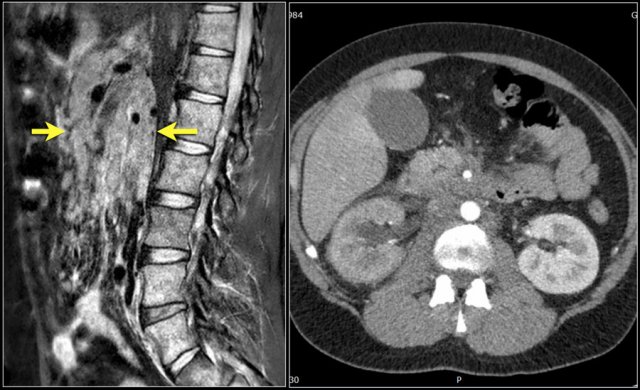
Here a 25 year old patient who presented with low back pain.
Notice multiple small masses in the abdomen surrounding the mesenteric vessels and abnormal low signal intensity of the bone marrow.
The signal intensity of the discus is a little bit higher compared to the bone marrow (bright discus sign).
This examination was the first indication of an abnormality in this patient.
This proved to be bone- and lymph node metastases of a carcinoma of the colon.
Here another patient with widespread lymphadenopathy in the mesenterium and retroperitoneum.
Here a patient, who presented with severe low back pain.
Notice the aortic dissection.
Sometimes these aortic abnormalities are incidental findings.
Disc herniation
Disc herniation is displacement of disc material like nucleus pulposus, parts of the annulus fibrosus and cartilage, beyond the limits of the intervertebral disc space.
It can be focal ( < 90º), broad-based ( 90º-180º) or caused by bulging of the disc (> 180º).
Protrusion indicates that the distance between the edges of the disc herniation is less than the distance between the edges of the base.
Extrusion is present when the distance between the edges of the disc material is greater than the distance at the base.
Read Spine - Disc Nomenclature for more information about disc herniation nomenclature.
Here a focal protrusion at the L5S1 level.
The S1 nerve is compressed (arrow).
Scroll through the images and describe the findings.
Then continue reading.
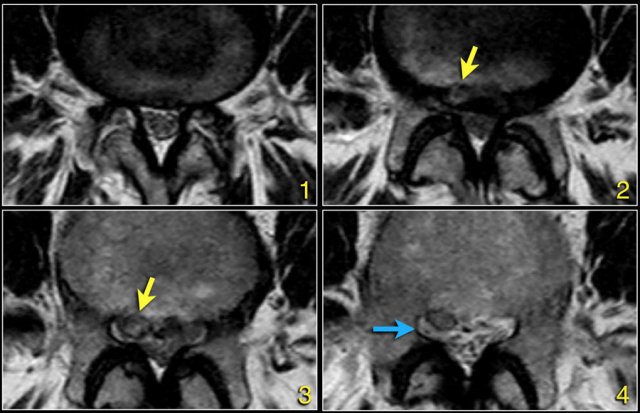
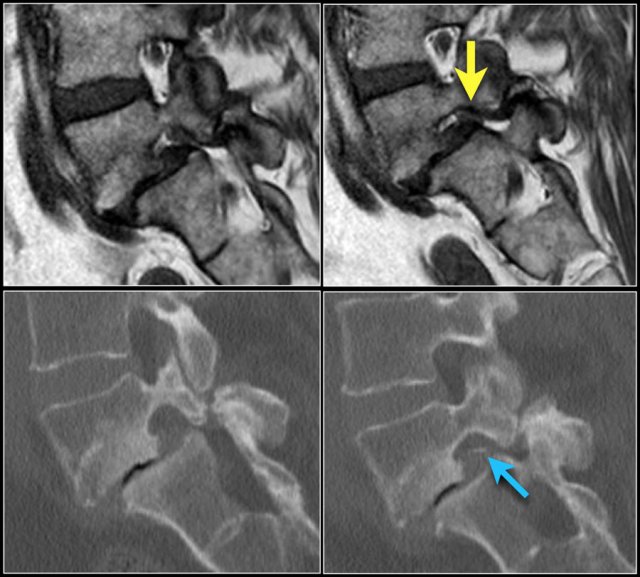
The findings at the different levels 1-4 are:
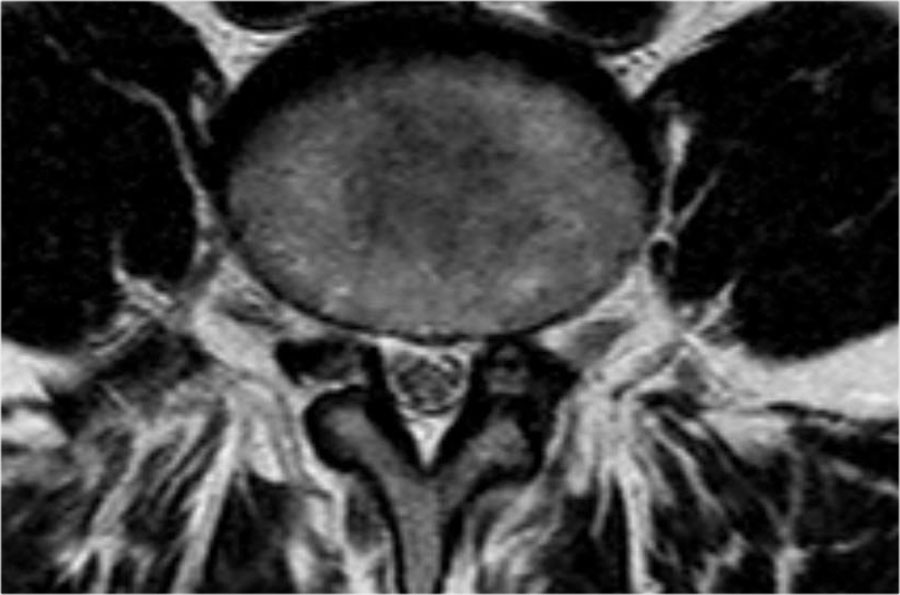
- At the level of the disc there is minimal spinal canal narrowing by bulging of the disc and facet arthrosis.
- At this level there is severe spinal canal stenosis due to bulging disc and facet arthrosis.
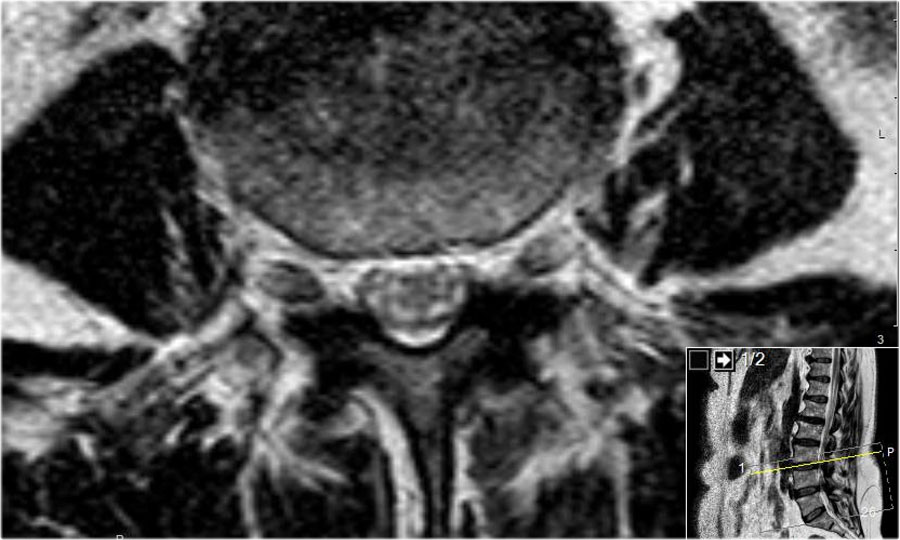
There is also an annular tear (high signal) through which the disc herniates (yellow arrow) - At the level of the lateral recess, there is a focal herniation of disc material compressing the L5 nerve (yellow arrow).
This is called an extrusion, because the distance between the edges of the disc material is greater than the distance at the base. - Compressed L5 nerve (blue arrow) within the lateral recess.
The herniated disc has migrated caudally and is seen as an oval structure anterior to the nerve.
The herniated disc is uncontained, i.e. not covered by fibers of the annulus.
First study the images.
Click to enlarge them.
Then continue reading.
The findings are:
- Herniation of the L3L4 disc.
- Migration cranially.
- Compression of the L3 nerve in the foramen.
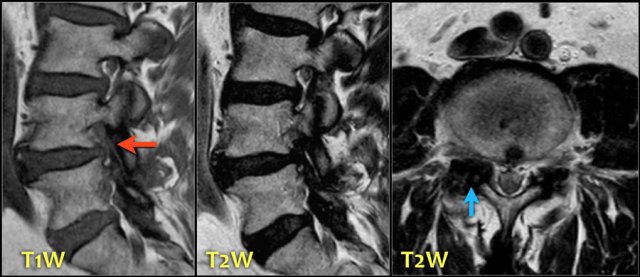
The signal intensity of a hernia on T1W-images is usually intermediate, while on T2W-images it can be a high signal fresh herniated nucleus pulposus or a somewhat older low signal intensity hernia.
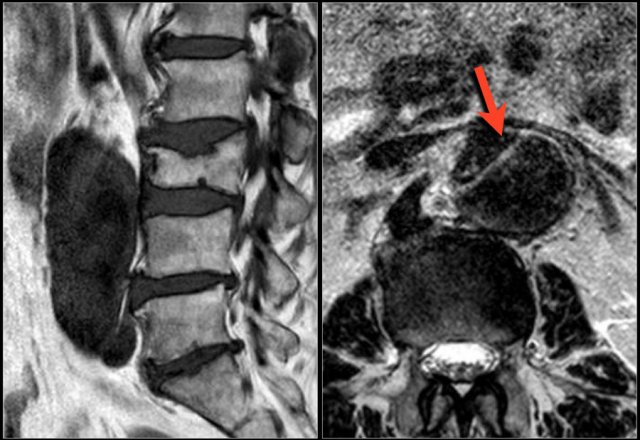
Here a herniation with high signal (yellow arrow on transverse images) sliding through the annular tear and compressing the left L5 nerve (blue arrow).
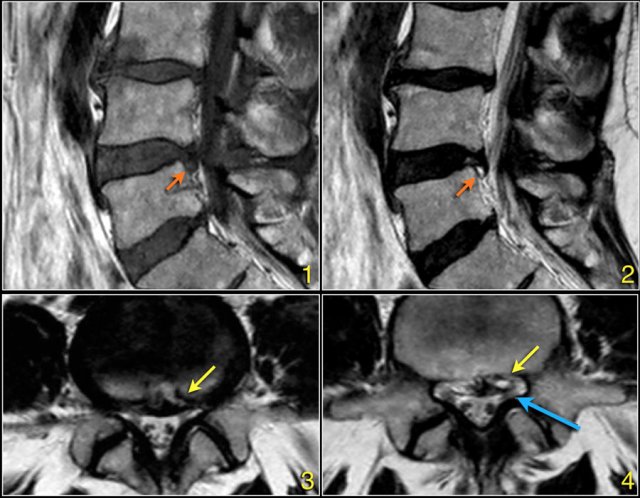
Here sagittal T1W-images demonstrating a structure of very low signal intensity at the L4L5 level (arrow) and at the L5S1 level.
Continue with the T2W-images.
Also on the T2W-images the signal intensity is very low.
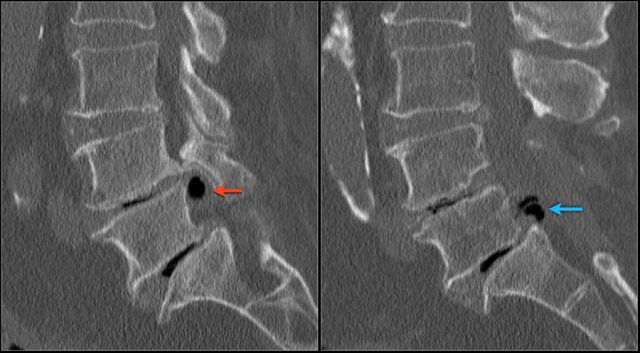
A CT-scan was performed to see if this could be a calcified herniated disc or some artifact.
Continue with the CT-images.
The low signal intensity could finally be explained by the vacuum phenomena due to nitrogen gas within the herniated disc both on L4L5 (red arrow) and L5S1 level (blue arrow)

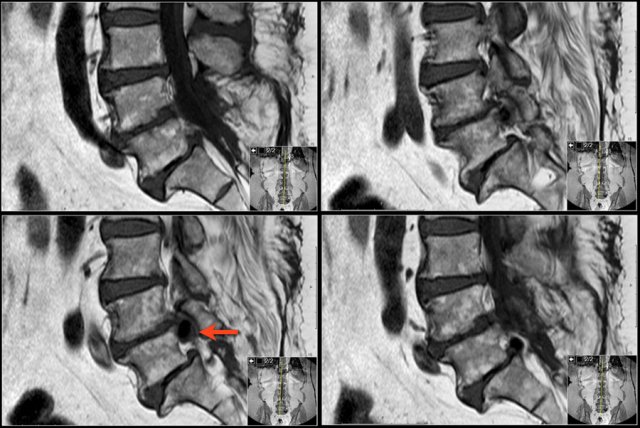
First scroll through these sagittal T1W-images.
What are the findings.
Then continue with the next series.

The most striking finding is a intermediate intensity structure posterior to the L3 vertebra (blue arrow).
It has the same signal intensity as the disc.
This is a hernia that has migrated cranially compressing the L3 nerve on the right side.

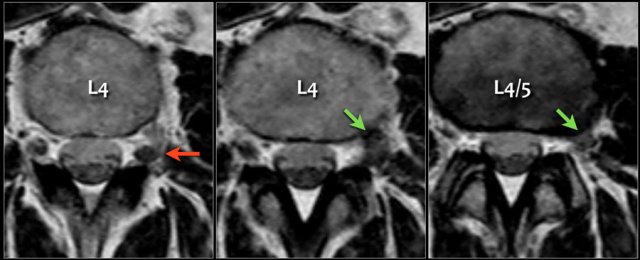
Here another example of disc migration.
Notice how the disc herniation at the L3L4 level migrates caudally behind the body of L4.
Notice that at the L4L5 level the migrated disc simulates a nerve root (green arrow), while in fact the nerve is compressed posteriorly and subsequently moves to the foramen (yellow arrow).
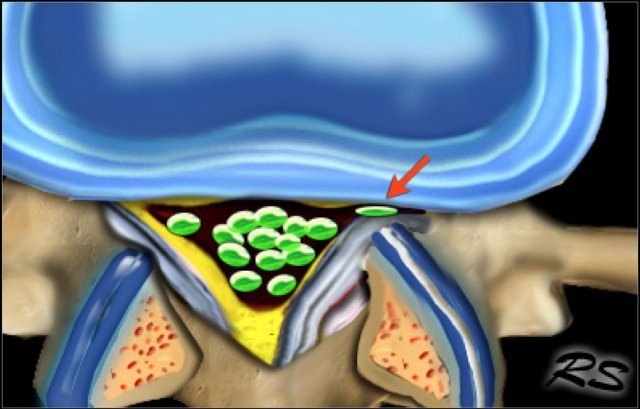
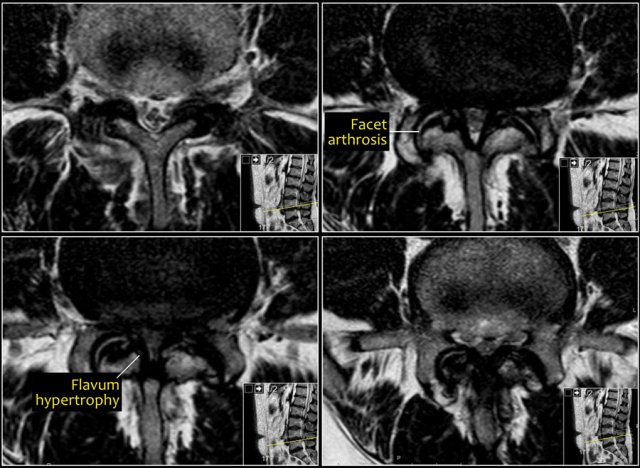
Lateral recess stenosis
Stenosis of the lateral recess is a common problem especially in older patients.
The stability of the vertebral column decreases, which results in instability.
This results in hypertrophy of the facet joints and arthrosis, bulging of the disc and more stress on the flavum ligament resulting in hypertrophy.
All these mechanisms lead to stenosis of the lateral recess (figure).
In advances cases of arthrosis a synovial cyst may form, which contributes to the narrowing.
Here a patient with bilateral facet arthrosis resulting in narrowing of the lateral recess on both sides with nerve compression.
Scroll through the images.
Synovial cyst
Synovial cysts are frequently seen in combination with facet arthrosis.
Mostly they lead to stenosis of the lateral facet.
When they are very large they can protrude into the foramen and cause foraminal stenosis.
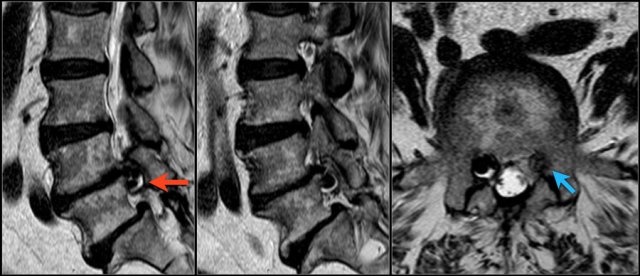
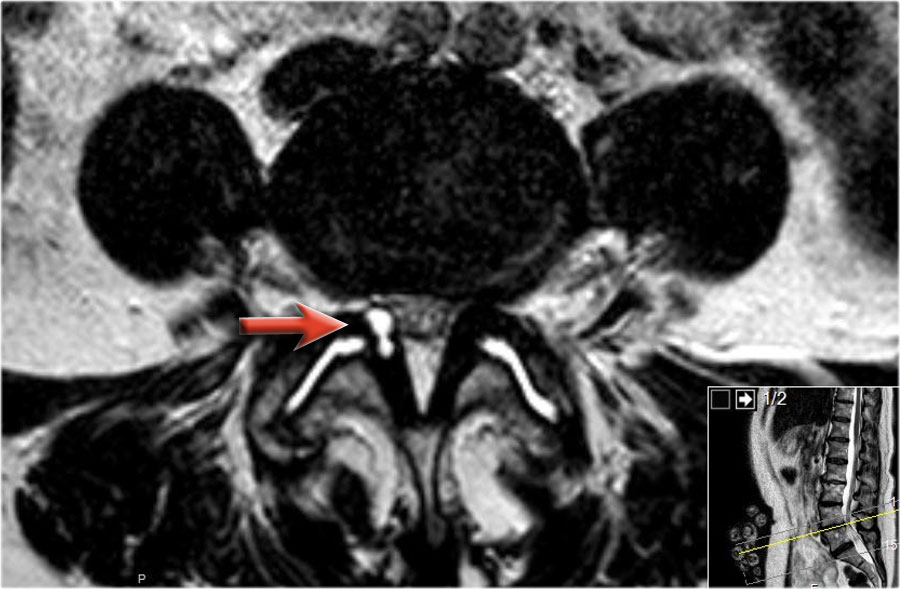
Here a patient with severe arthrosis of the facet joints.
Notice that there are many synovial cysts related to the arthrosis (red arrows).
At the L5S1 level a large cyst on the right compresses the S1-nerve (yellow arrow).

Here sagittal T2-weighted images of a patient with a synovial cyst, that completely fills the neuroforamen (arrow).
Notice that at first glance the foramen looks normal, but the nerve iseems to be missing.
The nerve is compressed by the cyst.
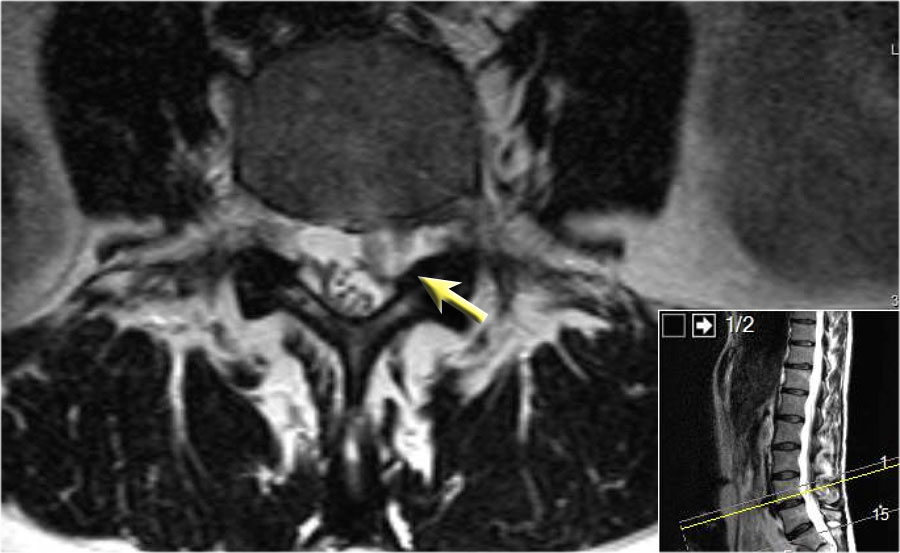
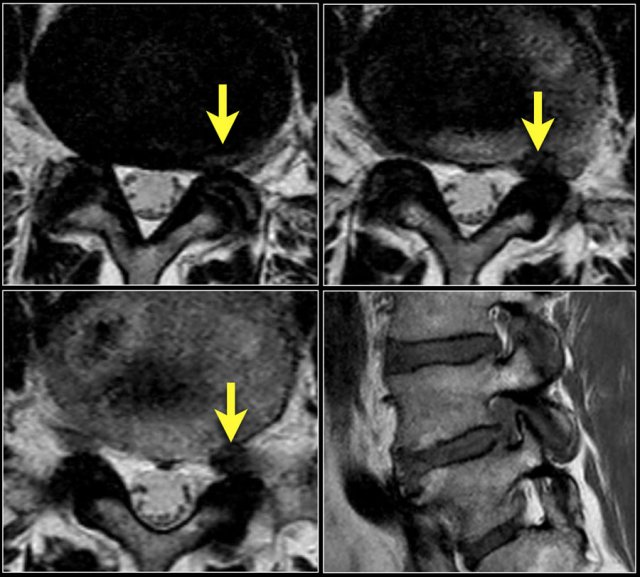
Here we have the axial images of the same patient.
Notice the dumbbell configuration of the synovial cyst at the level of the neuroforamen (yellow arrows).
Synovial cysts can be easily overlooked.
On these T2W-images it looks as if the foramen is normal.
Notice that the nerve is missing.
In fact the neuroforamen is almost completely filled by the synovial cyst, which compresses the nerve root against the vertebra (arrows).
The nerve can hardly be seen.
Stenosis of the Spinal Canal
Causes of spinal stenosis:
Most common
- Bilateral facet arthrosis in combination with bulging of the disc and hypertrophy of the ligamentum flavum
Less common
- Congenital narrowing with short pedicles
- Spinal injury and epidural hematoma
- Bone tumors
- Spondylodiscitis or epidural abscess
- Spondylolisthesis
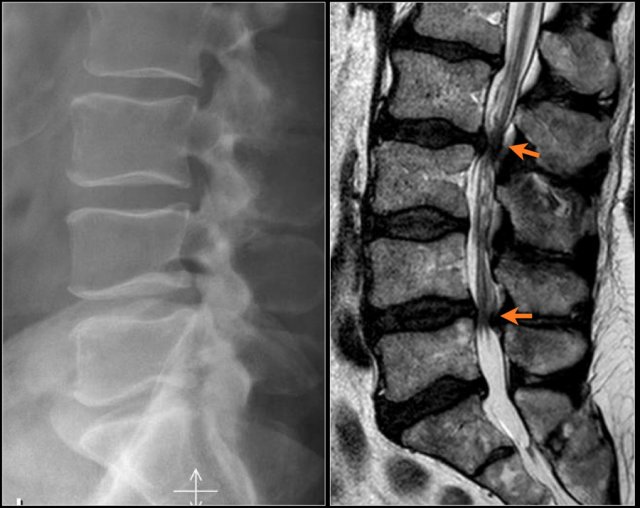
Notice the diffuse narrowing of the lumbar spinal canal.
It is best seen on the MR-images, but can already be suspected on the radiograph, because the pedicles are very short.
You may have to enlarge the image to appreciate this.
On the axial T2W-images you can see, that there is no CSF visible surrounding the nerve roots.
This means that there is a severe spinal stenosis.
The epidural fat compresses the nerves from posteriorly.
Here another example of spinal stenosis.
Again on the radiograph you can suspect congenital narrowing.
Usually a small hernia or bulging is enough to cause nerve compression in these patients.
On the axial T2W-images a severe spinal stenosis is seen.
Notice the short pedicles in combination with facet arthrosis and flavum hypertrophy.
Here a patient with multiple osseus metastases.
At the level of L1L2 this causes spinal stenosis with compression of the nerves (red arrow).
It is not that common for metastases to cause nerve compression at the lumbar level.
At the thoracic and cervical level metastases frequently cause compression because there is not much CSF surrounding the myelum.
Fractures can cause stenosis of the spinal canal especially when there is displacement of bony structures like in burst fractures and fractures with rotation and translation.
Here a patient with an old burst fracture.
There is retropulsion of the posterosuperior fragment (red arrow) compressing the cauda (blue arrow).
Epidural lipomatosis
Epidural lipomatosis is excessive amount of fat within the epidural space compressing the thecal sac.
Patients present with symptoms of spinal canal stenosis.
It is seen in patients with obesity, like in this case and in patients who are treated with steroids.
Continue with the axial images of this patient.

Scroll through the axial images.
Notice how the spinal canal is narrowed by the epidural fat.
Do not mistake the high signal intensity of the fat for CSF.
Foraminal stenosis
Causes of Foraminal stenosis:
- Facet arthrosis
- Disc herniation with upward migration
- Spondylolistesis
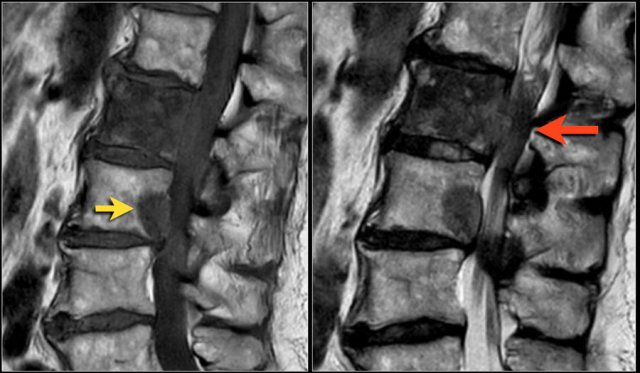
Stenosis of the neuroforamen is usually the result of a combination of upward disc herniation and facet arthrosis.
It is also frequently seen in patients with spondylolisthesis.
Spondylolisthesis is a condition in which one vertebra slips forward over the one below it, usually L4 upon L5.
The shift results from either spondylolysis (stress fracture of the pars interarticularis) or facetarthrosis with sliding of the facets.
Here a patient with severe facet arthrosis on the right side at the L4L5 level.
Scroll through the images of a patient with spondylolisthesis.
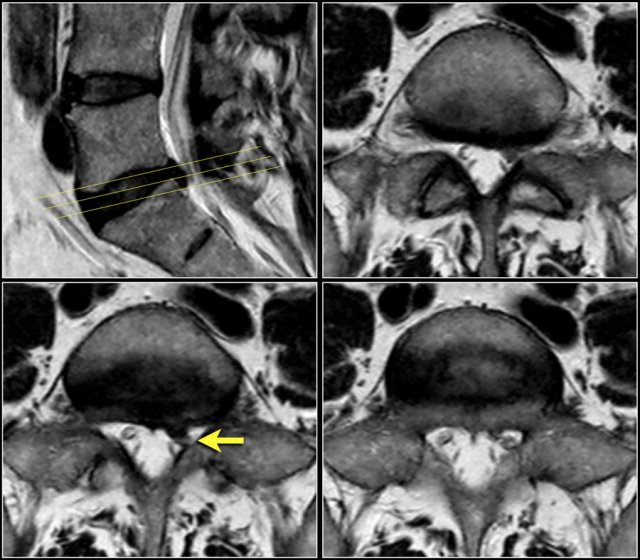
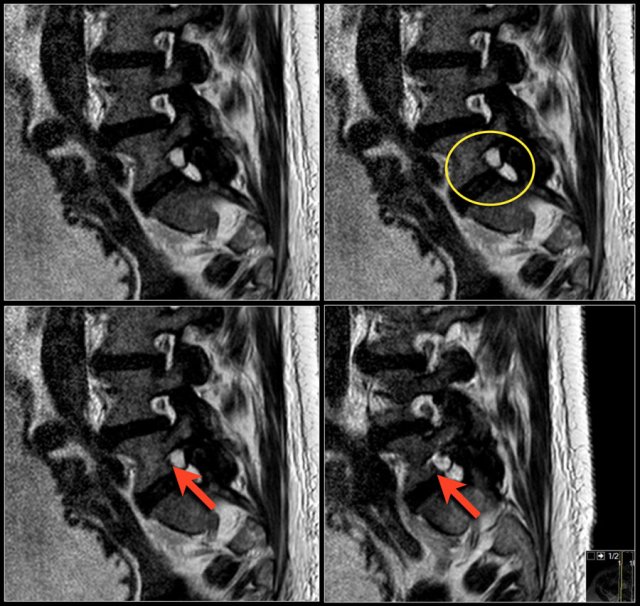
Here a disc herniation with upward migration.
By using the marker, you can correlate the abnormality on the T1W-image with the axial T2W-images.
On the T2W-image it is more obvious that this is a disc herniation.
The lower images are with the marker on.
you may have to enlarge the images to see it.
These foraminal disc herniations can be easily overlooked.
Notice how subtle the findings are on the axial T2W-images.
The herniated disc can be easily mistaken for the nerve root.
The sagittal T1W-image shows the upward migration of the disc.
Here a patient with a combination of spondylolysis (arrow), minimal listhesis and disc herniation resulting in compression of the L3 nerve within the foramen.
Here a patient with severe anterolisthesis due to bilateral spondylolysis.
The anteroposition in combination with the upward movement of the disc has resulted in severe narrowong of the foramen and nerve compression (yellow arrow).
Notice the calcification of the uppper part of the disc (blue arrow).
Extraforaminal nerve compression
Extraforaminal nerve compression is seen in about 5% of cases.
Almost always it is a lateral disc herniation from a lower level that compresses the extraforaminal part of the nerve.
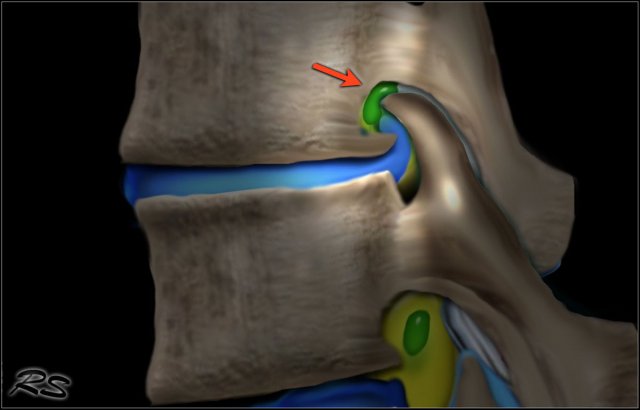
Here an example of a lateral disc herniation that produces compression of the superiorly exiting nerve root and ganglion.
Notice the L4 nerve (red arrow), which is being displaced posteriorly by a lateral disc herniation at the L4-5 level (green arrow).