MRI traumatic changes
Mini Pathria and Jennifer Bradshaw
Department of Radiology of the University of California School of Medicine, San Diego, USA and the Medical Centre Alkmaar, the Netherlands
Publicationdate
This article is based on a presentation given by Mini Pathria and was adapted for the Radiology Assistant by Jennifer Bradshaw.
In part I we will discuss MR features of various muscle injuries.
In part II we will discuss non-traumatic muscle changes.
Introduction
Dr. Pathria is a Professor of Clinical Radiology at the University of California, San Diego .
Dr. Pathria's specific areas of interest include musculoskeletal trauma, emergency radiology, and musculoskeletal MR imaging.
She is the author of the book MRI of the Musculoskeletal System.
 Normal muscle is symmetrical with smooth convex borders, linear branching and feathery fat planes and low signal on all sequences
Normal muscle is symmetrical with smooth convex borders, linear branching and feathery fat planes and low signal on all sequences
When looking at muscle on MR there are a few rules to keep in mind:
- Normal muscle is quite symmetrical. An exception would be an active sporter with a dominant side
- The outside borders tend to be smooth and convex, so no bulging
- Muscle should have low signal on all sequences
- On T1-weighted images you will see fat in the muscle in very predictable patterns, with either linear, branching or feathery distributions, depending on the architecture of the muscle.
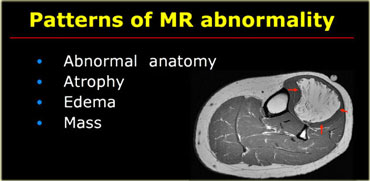
When looking at muscle pathology try to decide which one of the four basic patterns of abnormality is present:
- Abnormal anatomy with normal signal, i.e. accessory muscle
- Muscle atrophy, i.e. too much fat
- Muscle edema, i.e. too much water while retaining normal architecture due to muscle injury, myositis and imflammatory myopathy
- Mass within muscle, i.e. soft tissue tumor, hematoma or abscess
On the left an example of a lipoma creating a mass effect in the anterior compartment of the calf.
Muscle injury
The most common muscle injury is muscle strain (1).
It is an injury to the musculotendinous junction.
Typical for muscle strain is edema centered along the musculotendinous junction (1).
More severe muscle strains contain fluid collections such as hematomas and may contain grossly interrupted muscle fibers and thus may show masslike features on MR images in addition to muscle edema.
Muscle contusions are caused by a direct blow.
MR images reveal interstitial hemorrhage as well as edema at the injured site .
More severe contusions may contain hematomas and thus reveal a masslike lesion in addition to the edema.
Muscle Strain
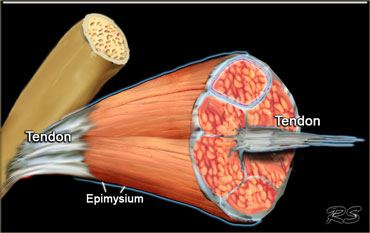
Muscle strain is an injury to the musculotendinous junction.
The tendinous junction is where the muscle fibers meet the tendon, and the shape of it varies in different muscles.
In many muscles, the tendon extends deeply into the muscle creating a long musculo-tendinous junction (figure).
This area is especially important in a trauma setting, because it is often involved.
The epimysium is the fibrous tissue that lies at the edge of the muscle.
It becomes the muscle sheath that fuses with the tendon.
This is also an important area to consider because when there is a tear in the muscle, fluid tends to leak out and collect in the epimysium.
The pattern of edema in muscle strain will depend on the architecture and shape of the musculotendinous junction involved.
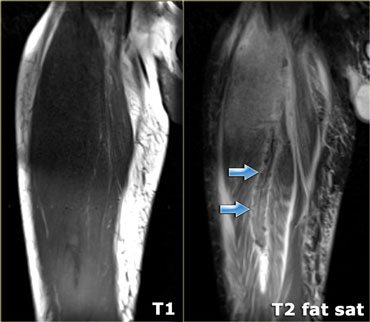
The image on the left nicely demonstrates the feather-like arrangement of the musculotendinous junction in an atrophic muscle.
The image on the left demonstrates edema surrounding the musculotendinous junction in a feather-like arrangement.
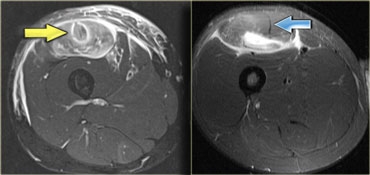
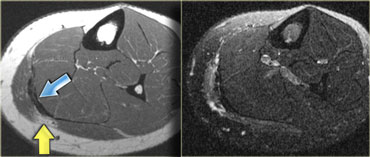
This is a complete tear to the rectus femoris (arrows).
The architecture can be very confusing.
For example on the left the rectus femoris, which can show a variety of edema patterns depending on where (anatomically)
the injury took place.
The blue arrow demonstrates the tendon of the indirect head, which comes from the hip, it has a vertical orientation
on this axial image.
Along the posterior portion of the muscle (yellow arrows), there is a flat area of tendon originating from the knee.
When a muscle has different orientations of the tendons it means that there are different patterns of edema possible
depending on the tendon injured.
Therefore this is a pattern of edema corresponding to an injury arising from the knee.
Muscle Strain (2)
Muscle strain is an acute injury.
The history is usually very concise.
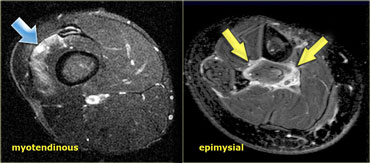
The muscles that are most prone to strain are the long fusiform muscles that cross 2 articulations.
Most at risk are the hamstrings, rectus femoris and medial gastrocnemius.
Strain involving the upper extremity is slightly less common and then usually involves the biceps brachii.
The hallmark of strain is a lot of edema around the myotendinous juntion because that is where the tearing takes place.
There is edema around the tendon and sometimes the tendon itself will show signal changes.
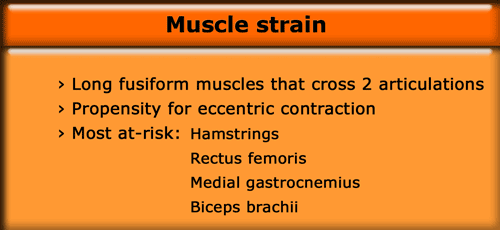
There are 2 patterns found with muscle strain.
By far the most common is the myotendinous junction pattern, which occurs roughly 97% of the time.
Depending on the severity of the strain, there might also be fluid collections.
The remaining 3% will show an epimysial strain pattern, with the abnormalities found at the periphery of the muscle.
Muscle Strain (3)
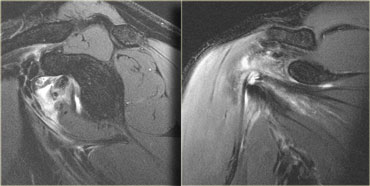
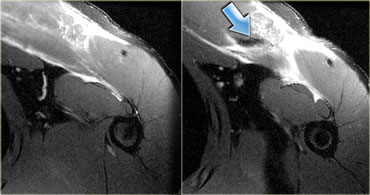
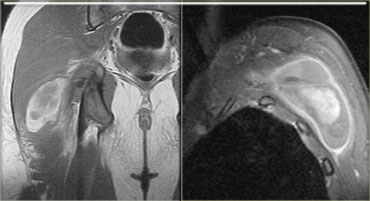
On the left an example of a weight-lifter with an epimysial strain pattern.
The tendon tears at the myotendinous junction, and the fluid leaks around the edge of the muscle showing an epimysial appearance.
Do not confuse this with a degenerative or impingement-type tear.
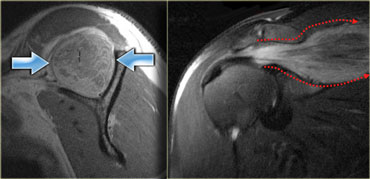
On the left a strain with partial tear of the subscapularis.
The subscapularis is a convergent muscle (like for example the pectoral muscle) with multiple tendons.
Edema will have a multipennate distribution pattern, as the edema tracks in different directions along the multiple tendons.
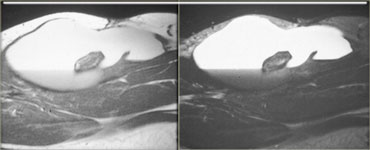
On the far left a complete tear of the indirect head of the rectus femoris (yellow arrow).
This tear originates in the hip.
The image next to it, which was also shown above, shows a completely different finding.
There is edema surrounding the distal tendon that is connected to the patella.
The other tendon is completely normal (blue arrow).
Grading muscle strain
Clinically the severity of a muscle injury is graded from 1-3.
Trying to grade a muscle injury by the signal intensity is tricky.
Chronic injuries can show mild signal changes and yet still be high grade injuries according to the clinical classification.
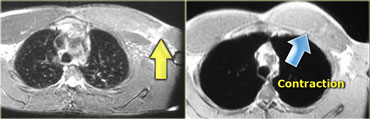
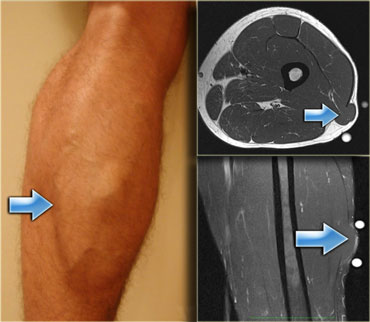
On the left an example of a tear in the left pectoral muscle.
On T1-weighted image there is a gap in the muscle with a small amount of fat filling it up.
The gradient echo demonstrates focal fluid accumulation and some increased signal within the muscle.
It does not look that severe.
However, when asked to fully contract the pectoral muscles there is an obvious asymmetry due to a complete tear in the muscle (blue arrow).
This clinically is a grade 3 injury, with a complete loss of function of the muscle.
Low grade muscle strain
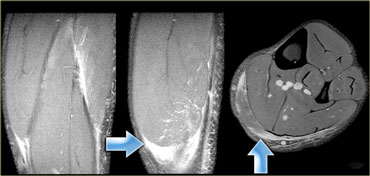
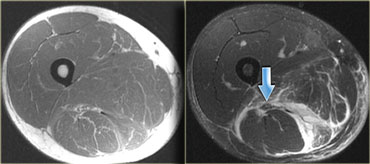
On the left a low grade injury of the flexor hallucis longus.
There is normal muscle architecture on the T1-weighted image, and increased signal on T2-weighted image and STIR.
The injury will heal completely within a couple of weeks.
This example shows edema with an epimysial pattern which is common around the flexor hallucis.
When grading acute injuries, look not only at the architecture but also at the length of the muscle.
Studies have shown that the length of the muscle strain is the best predictor of the duration of disability, with longer lesions requiring more time to recover.
(Reference article by Dr. Connell DA et al, AJR 2004, 83: 975-984).
So the longer the abnormality, the longer it takes for the injury to heal.
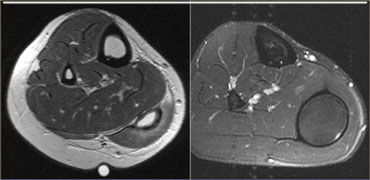
On the left a patient with 2 grades of injury to the gastrocnemius.
There is a low grade injury to the lateral head.
Moderate grade muscle strain
On the left the same patient.
There is also a moderate grade injury to the medial head.
Note the fluid accumulations around the muscle head.
The more fluid, the higher the grade.
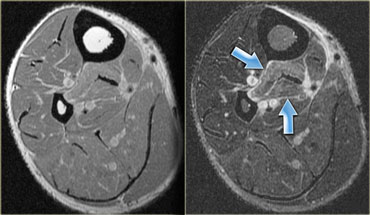
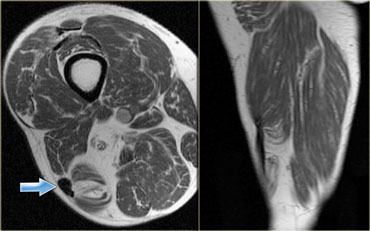
On the left an injured rectus femoris muscle.
The images demonstrate a moderate grade injury, with architectural distortion and a fluid collection (arrow).
Notice the edema at the bipennate musculotendinous junction.
High grade muscle strain
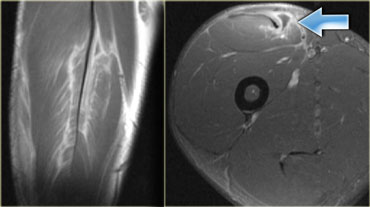
On the left an example of a high grade injury.
There is a complete tear of the tendon or myotendinous junction of the pectoral muscle.
This patient will lose all function in this muscle.
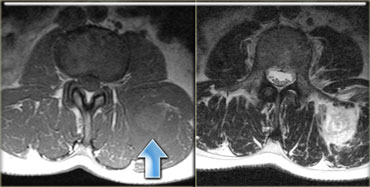
On the left a complete tear of the left hamstring at the musculotendinous junction.
Tthe tendons are avulsed and there is fluid accumulation.
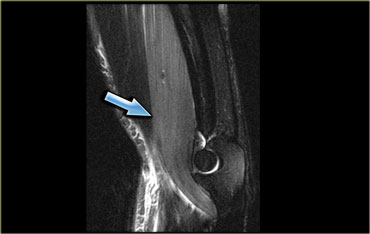
On the left a different patient with also a complete hamstring rupture.
There is an epimysial pattern of edema and sciatic nerve irritation.
A hamstring syndrome may occur.
This is a painful condition caused by post-traumatic scar formation around the sciatic nerve (arrow).
Chronic changes of muscle strain
On the left images of a patient who had a prior muscle strain.
There are typical chronic changes such as focal tendon thickening (blue arrow) and peritendinous muscle atrophy (yellow arrow).
On the left images of a patient who had an injury to the long head of the biceps femoris muscle.
There are typical chronic changes such as focal tendon thickening (blue arrow) and severe muscle atrophy.
Contusion
Muscle contusions are caused by a direct blow.
The MR findings in contusion are similar to strain but without the typical myotendinous junction localization seen in the latter.
Typically, there is also skin edema and sometimes, bone contusion.
MR images reveal edema at the injured site, frequently due to interstitial hemorrhage as well as edema.
More severe contusions may contain hematomas and thus reveal a masslike lesion in addition to edema.
It is mostly seen in the superficial muscles.
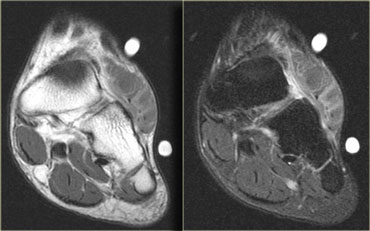
On the left images of a patient who has a mass-like swelling of the fore-foot.
The findings are nonspecific, but the history 'Slammed car door on foot' was specific.
Hemorrhage
Hemorrhage can present as a discrete hematoma or as parenchymal hemorrhage.
In the case on the left there is a mixed pattern.
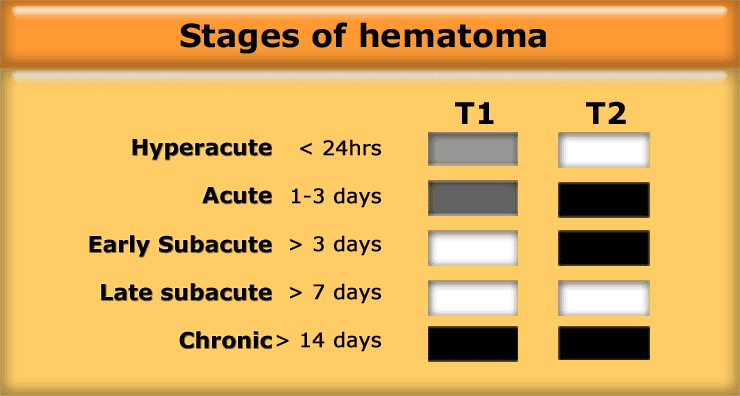
The signal intensity of a hematoma on T1W- and T2W-images depends on the stage of the hematoma (Table).
On the left images of a patient who fell on a slippery floor.
There is a hyperacute hematoma.
Low signal intensity on T1W and high signal on T2W.
On the left an acute hematoma.
It is isointense or hypointense to muscle on T1.
The hypointensity in T2WI in the acute period is due to the high concentration of intracellular deoxyhemoglobin.
On the left images of two different patients with an early subacute hematoma.
On the far left a T1-weighted image.
The hyperintensity at the periphery of the hematoma is due to methemoglobin which is seen after 2-7 days and can persist for months.
The image on the right shows the same hyperintensity on a T2-weighted image.
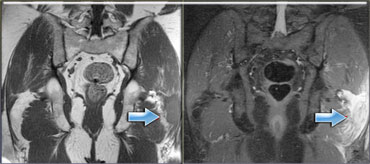
On the left a late subacute hematoma with layering.
On the left images of two different patients with a chronic hematoma in the calf.
On the left a T1-weighted image.
Notice the dark rim of hemosiderin surrounding the hematoma.
On the right a T2-weighted image of a similar case.
Notice that the hemosiderin is also dark on T2-weighted image.
Morel-Lavallee
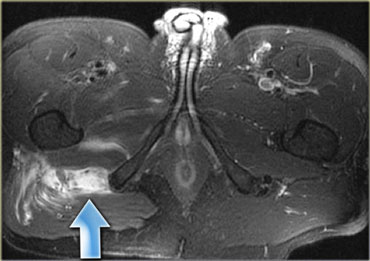
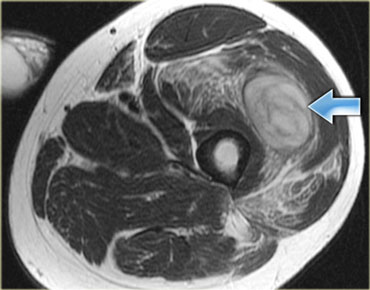
On the left a chronic hematoma known as Morel-Lavallee lesion.
A Morel-Lavallee lesion is the result of separation of the skin and subcutis from the fascia, producing a cavity that is filled with fluid and debris.
These lesions are found around the thigh and have a well-defined oval or fusiform shape.
They are usually partially or wholly encapsulated
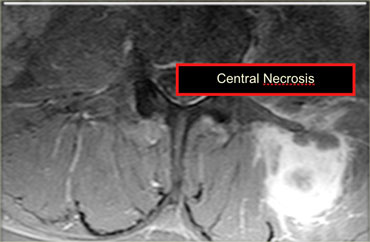
A hematoma can look like a tumor and vice versa.
On the left a metastasis of a renal cell carcinoma.
When in doubt use gadolinium to see if the abnormality enhances.
Continue with the post-Gad image.
The majority of the lesion enhances, making hematoma unlikely.
In the centre there is no enhancement as a result of necrosis.
Hematomas can show some enhancement, but only at edge.
Myositis ossificans
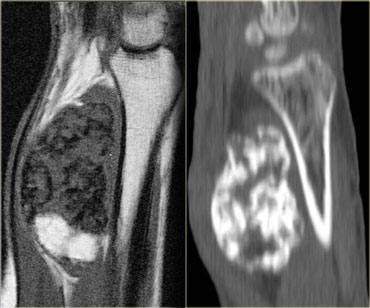
Severe blunt trauma causing an intra-muscular hematoma may result in delayed ossification in the soft tissues known as myositis ossificans.
Myositis ossificans has a variable appearance depending on the maturity:
- Nonspecific mass
- Peripheral ossification
- Marrow cavity formation
On MRI myositis ossificans can be difficult to differentiate from osteosarcoma.
On X-rays and CT soft tissue ossification not attached to bone is seen.
On the left another case of myositis ossificans with bone formation.
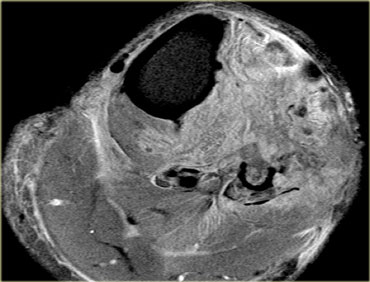
Compartment syndrome
Compartment syndrome is a limb-threatening and life-threatening condition observed when perfusion pressure falls below tissue pressure in a closed anatomic space.
A fasciotomy procedure with incision in the skin and the muscle fascia is necessary to release the pressure and regain normal function of the capillaries.
Compartment syndrome progresses to rhabdomyolysis if untreated.
Necrosis of tissue may begin at interstitial pressure as low as 30 mm
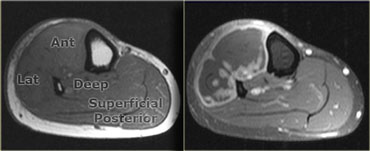
In the lower leg there are four compartments: the anterior, deep and superficial posterior compartment and a small lateral compartment.
On the left T1W-images of a patient one month post trauma.
On the post-Gadolinium image the necrosis in the anterior and lateral compartment is seen.
The posterior compartment is normal.
On the left a T2W-image of a patient with a chronic lateral compartment syndrome.
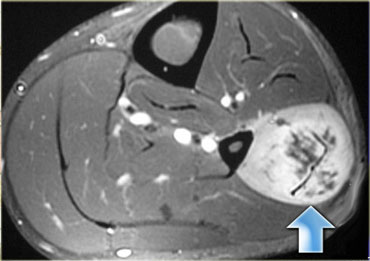
On the left a compartment syndrome in the upper leg which progressed to rhabdomyolysis.
Rhabdomyolysis is a dissolution of skeletal muscles that causes extravasation of toxic intracellular contents from the myocytes into the circulatory system and can lead to kidney failure.
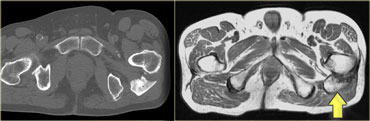
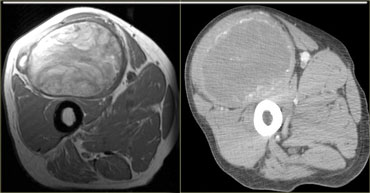
Calcific myonecrosis
Calcific myonecrosis is a rare post- traumatic entity characterized by latent formation of a dystrophic calcified mass occurring almost exclusively in the lower limb.
In calcific myonecrosis an entire single muscle is replaced by a fusiform mass with central liquefaction and peripheral calcification.
They can present as enlarging soft tissue masses with clinical features that suggest an enlarging soft-tissue neoplasm or infection.
Laceration
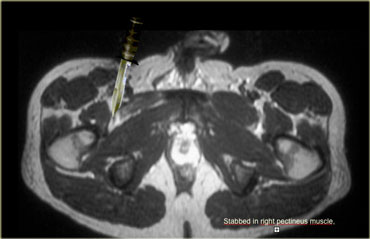
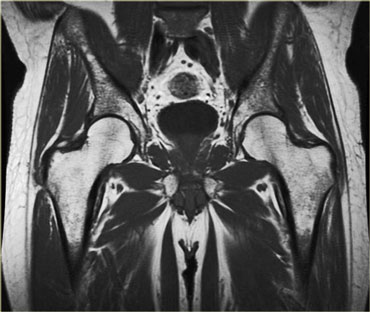
On the left a patient who met up with the wrong end of a knife.
The man was caught by his wife while cheating on her with another woman and he was rewarded with a stab into the groin.
This resulted in a laceration of his right pectineus muscle.
MR imaging is usually not required for laceration, since these patients usually go directly to the ER or OR for surgical exploration, but this case nicely demonstrates the atrophied muscle and the scar tissue.
Delayed onset muscle soreness
Delayed onset muscle soreness (DOMS) develops 1-2 days following exercise and resolves in 1-2 weeks (for example after the first days on the ski slopes).
DOMS is a type of overuse injury that does not become symptomatic until hours or days after the overuse episode, in contrast with a muscle strain or contusion, which usually is immediately painful.
The MR findings show diffuse muscle edema that does not localize to the myotendinous junction and can persist for weeks.
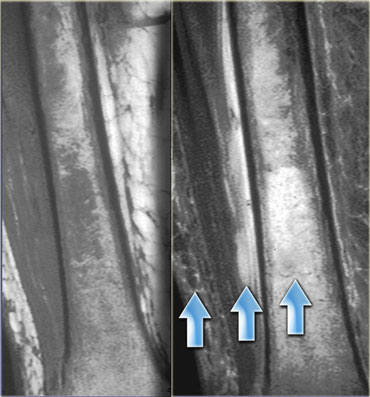
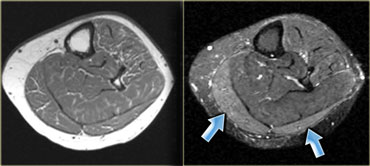
On the left a patient who had gone for a run for the first time in quite a while.
The muscle is irritated as illustrated by edema in the gastrocnemius (arrows).
Because there is a delay in symptoms, patients are not always aware of when or how the injury was actually caused.
On the left a navy recruit with delayed onset muscle soreness after weight-lifting.
Note the swollen edematous brachialis muscle.
These abnormalities can last for weeks.
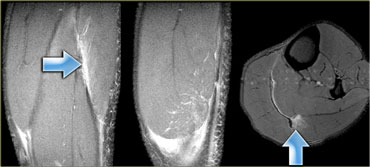
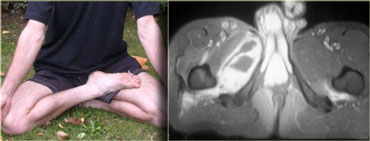
Fascial hernia
A fascial tear presents as a mass, the signal is usually normal (rather like an accessory muscle).
The muscle herniates through the fascial defect, protruding upon muscle contraction.
It is an intermittent mass and can be missed on MR if it is only visible during contraction.
A fascial tear is a typical sports injury and most commonly involves the calf (figure).
This type of muscle injury is well evaluated with ultrasound, because it is an dynamic examination.