Anatomy and Pathology of the Infrahyoid Neck
Frank Pameijer, Erik Beek, Frank Joosten and Robin Smithuis
Radiology department of the University Medical Centre of Utrecht, the Rijnstate Hospital in Arnhem and the Rijnland hospital in Leiderdorp, the Netherlands
Publicationdate
In this article we will focus on:
- a 3-step approach on how to analyze pathology of the infrahyoid neck on cross-sectional imaging..
- the 5 anatomical spaces of the infrahyoid neck.
Anatomy of the Infrahyoid Neck
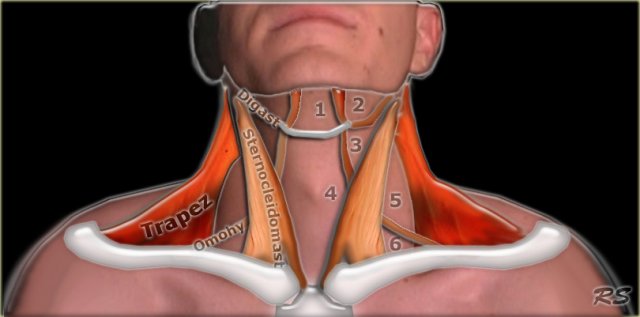
Surgical triangles
The infrahyoid neck is the region of the neck extending from the hyoid bone to the thoracic inlet.
Traditionally the anatomy of the infrahyoid neck has been subdivided into a group of surgical triangles whose borders are readily palpable bones and muscles (figure).
These triangles have a cranial-caudal orientation and therefore are difficult to correlate with cross-sectional imaging.
Another approach to the anatomy of the neck is the so-called 'spatial approach', which we shall use in this review.
Notice the musculus omohyoideus in the illustration.
This is one of the 'strap' muscles, an important landmark in the neck.
It is a group of four pairs of muscles in the anterior part of the neck: the sternothyroid, sternohyoid, thyrohyoid and omohyoid muscles.
They are all attached to the hyoid bone and look like a strap.
The other strap-muscles are not drawn in this illustration.
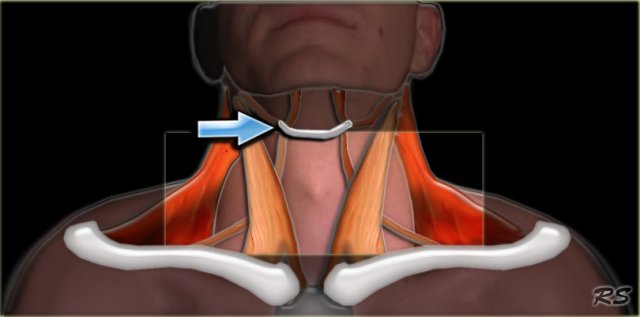
In the spatial approach to the anatomy of the infrahyoid neck, the cross-sectional anatomy is described as a series of spaces defined by the various layers of the deep cervical fascia.
This facilitates the understanding and interpretation of cross-sectional imaging modalities like CT and MRI (1).
Some of these infrahyoid spaces are continuous with the suprahyoid neck and some are continuous with the superior mediastinum.
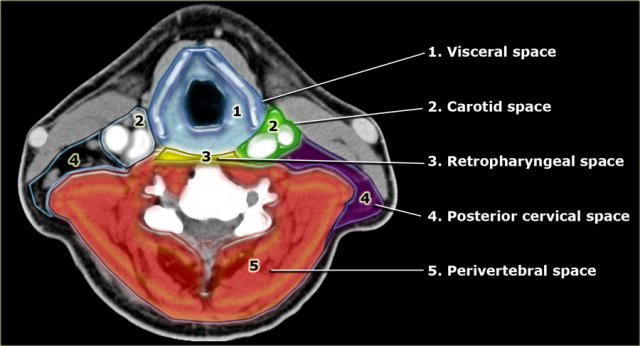
Spaces of the infrahyoid neck
The infrahyoid neck is divided into 5 major anatomical compartments or spaces by the various layers of the cervical fascia (2).
These spaces are well recognized in the axial plane and therefore suited for analysis on axial CT or MR.
- Visceral space
Central compartment containing several viscera like the larynx, thyroid, hypopharynx and cervical esophagus. - Carotid space
Paired space just lateral to the visceral compartment which contains the internal carotid artery, internal jugular vein and several neural structures. - Retropharyngeal space
A small virtual space containing only fat continuous with the suprahyoid space and the middle mediastinum. - Posterior Cervical Space
Paired space posterolateral to the carotid space.
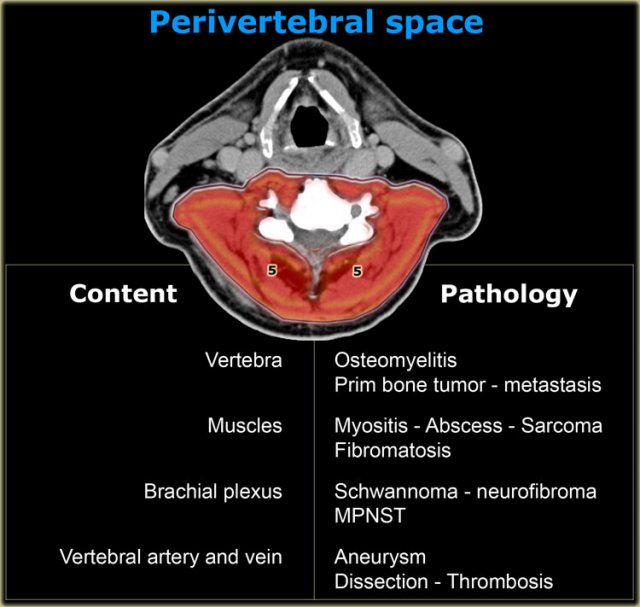
It contains fat, lymph nodes and neural elements. - Perivertebral space
This large space completely encircles the vertebral body including the pre- and paravertebral muscles.
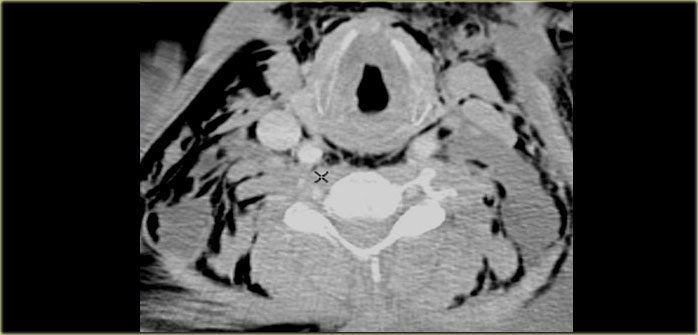
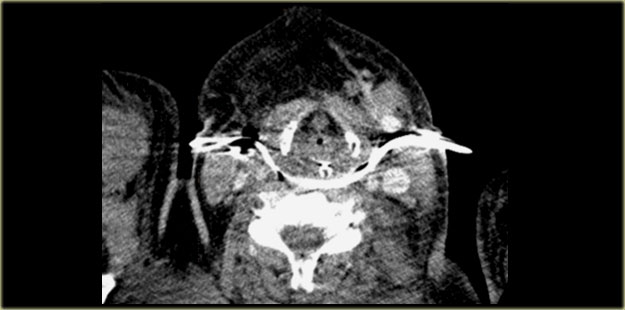
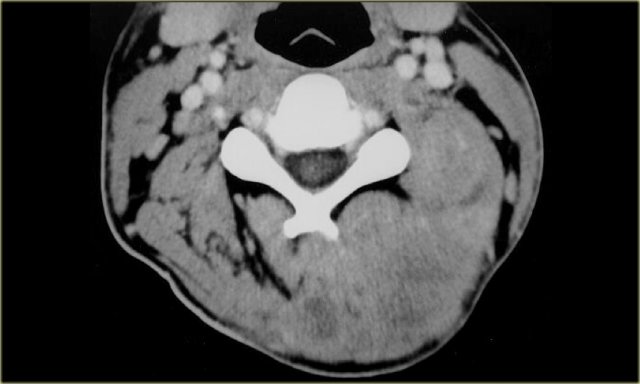
On the left a CT image of a patient with massive subcutaneous emphysema after a motor vehicle accident.
Air has dissected along the layers of the cervical fascia.
Notice that you are able to find all five spaces - they are now outlined by air.
Systematic approach
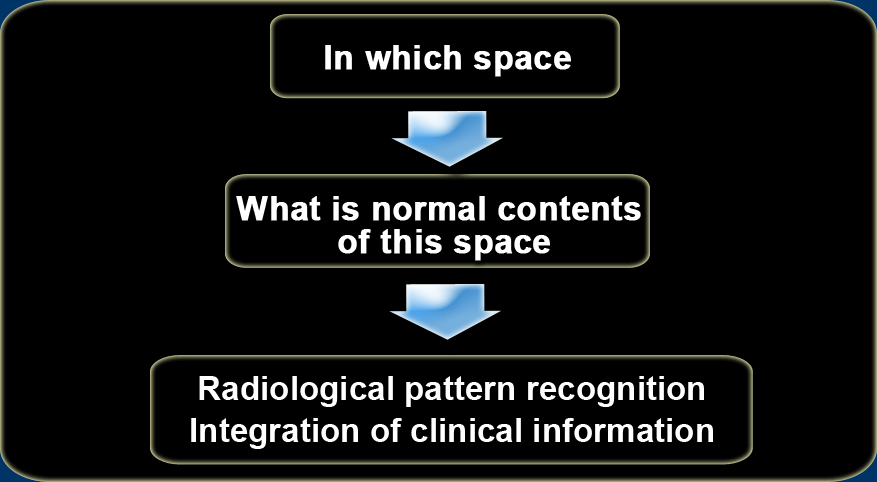
The systematic approach to pathology in the infrahyoid neck is a three-step procedure:
- Step 1:
In which space is the lesion located? - Step 2:
What are the normal contents of this space? - Step 3:
What pathology arises from these contents and can we recognize a specific radiological pattern and does this correspond to the clinical information?
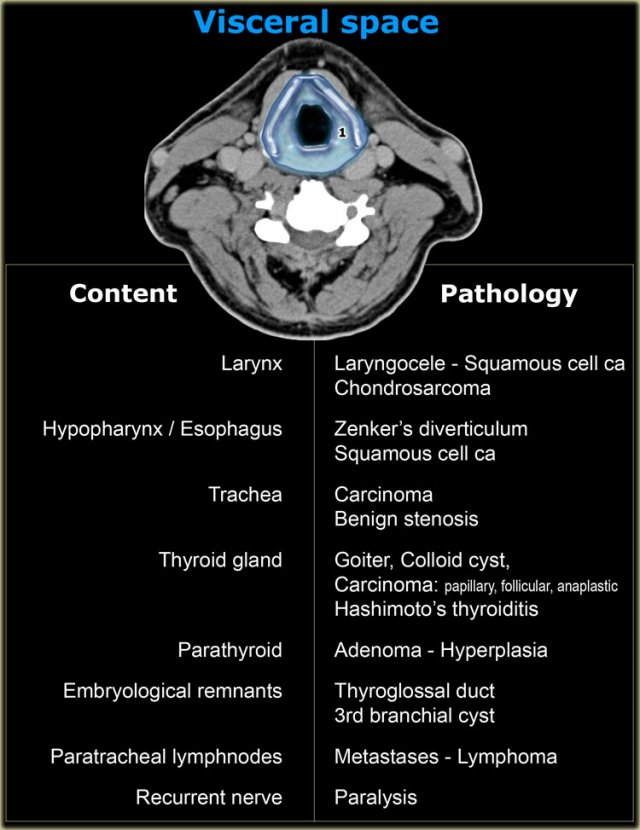
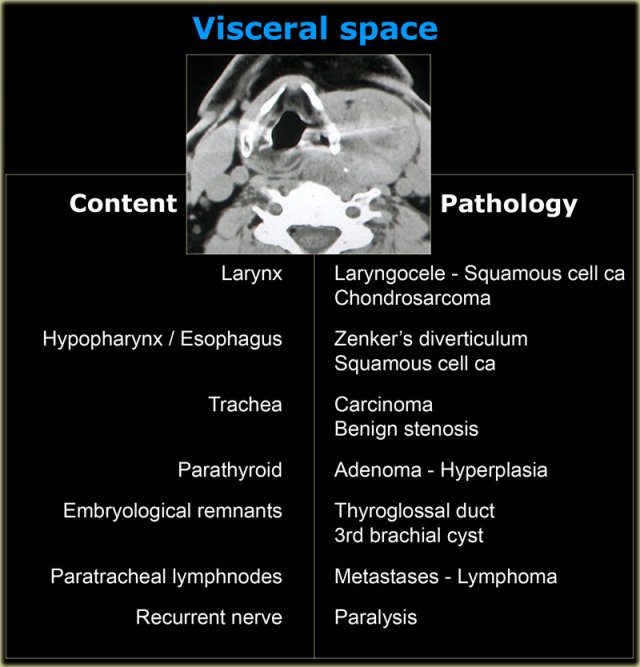
Visceral space
The visceral space extends from the hyoid to the anterior mediastinum and does not extend into the suprahyoid space.
On the left the normal contents and derived pathology of the visceral space.
The CT section is at the level of the supraglottic larynx and the thyroid cartilage.
Anterior to the thyroid cartilage are the 'strap' muscles: sternothyroid, sternohyoid, thyrohyoid and omohyoid .
They are all connected to the hyoid and depress the hyoid bone and larynx during swallowing and speaking.
These muscles are long and flat much like a strap.
We will now continue with a few cases.
Although we have provided the diagnosis in these cases, we still want you to follow the 3-step approach.
Laryngocele
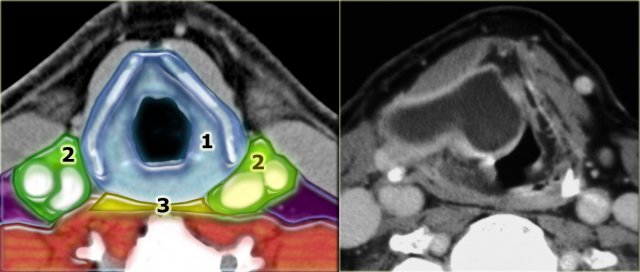
Step 1: which space
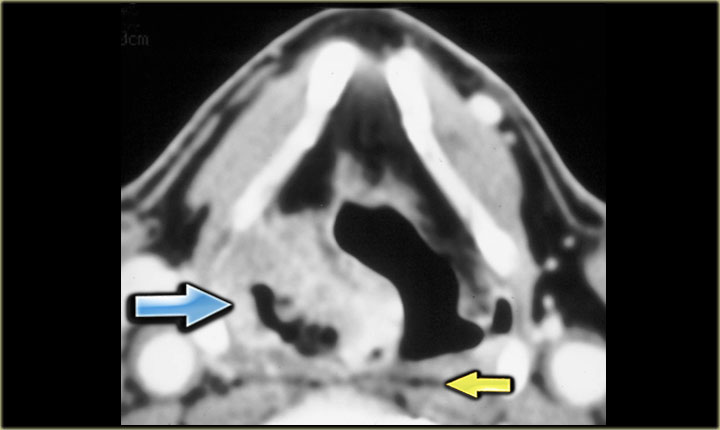
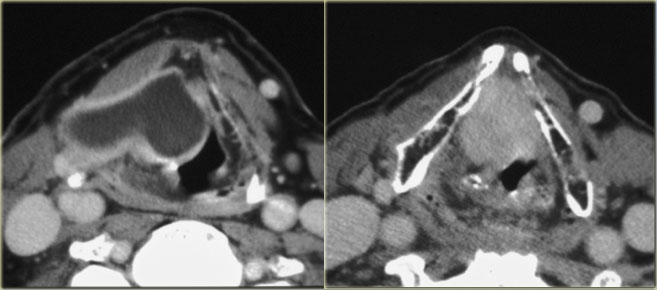
On the left a patient with a swelling on the right side of the neck.
Study the image and decide in which space the lesion is located.
Then continue reading.
The swelling is centered within the borders of the thyroid cartilage.
Therefore this must be pathology arising in the visceral space.
Step 2: normal contents
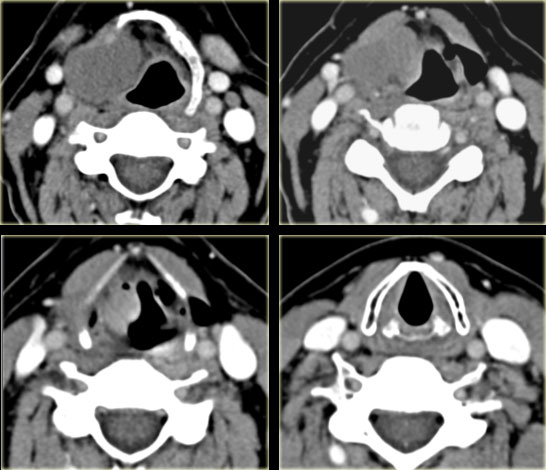
On the left an additional image is shown at a slightly lower level.
Study the images and decide which structures in the visceral space are present at this level and which are not.
Then continue reading.
The CT section shows the lesion present at the level of the supraglottic larynx and the thyroid cartilage.
So we are much too cranial for trachea, thyroid gland, parathyroid glands and recurrent laryngeal nerve, which lies in the tracheo-esophageal groove.
Paratracheal Level VI lymph nodes are located around the larynx and not within the larynx, so they can be ruled out.
The hypopharynx is posterior to the lesion and has a normal appearance.
Embryological remnants like thyroglossal duct cyst can be considered, but these are typically embedded in the laryngeal strap musculature and therefore should be located anterior to the thyroid cartilage.
So the only normal anatomy from which this lesion could have arisen is the larynx.
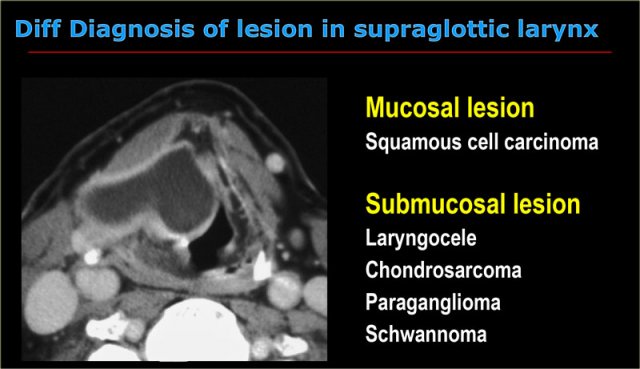
Step 3: Pattern recognition
This lesion presents as a cystic lesion with sharply defined, enhancing boundaries.
The lesion is located in the supraglottic larynx in the right paraglottic space and also has an extralaryngeal component, which explains the lump on the right side of the neck.
At endoscopy a large submucosal swelling on the right was seen in the larynx.
Squamous cell cancer, which is a mucosal disease, can therefore be dismissed.
When we think about the radiological appearance of the four submucosal entities mentioned in the table on the left, we can make the following remarks:
- Chondrosarcoma: we would expect irregular calcifications as in all malignant cartilage tumors. This lesion however has no calcifications.
- Paraganglioma: this is a hypervascular lesion and this lesion only has enhancing walls.
- Schwannoma: a rare lesion at this location and we would expect a more solid looking appearance, while this lesion is completely cystic.
- Laryngocele: which is the diagnosis
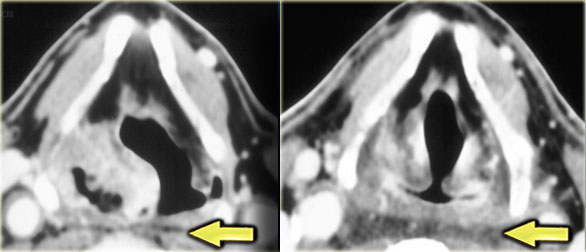
 Secondary internal and external laryngocele caused by a tumor at the level of the laryngeal ventricle ( enhancing mass on the right image)
Secondary internal and external laryngocele caused by a tumor at the level of the laryngeal ventricle ( enhancing mass on the right image)
Laryngocele (2)
When a larynocele is suspected you always have to search carefully for an underlying cause.
Primary laryngocele has no underlying cause.
Secondary laryngocele arises due to pathology in the laryngeal ventricle, which is a slit-like opening between the true and the false vocal cords.
A secondary laryngocele is frequently caused by a squamous cell carcinoma, as in this case.
At endoscopy the tumor may be obscured by the laryngocele itself.
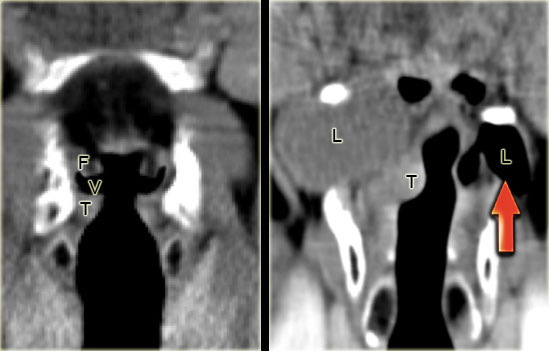 LEFT: Coronal CT image through the larynx with normal anatomy: false cords (F), true cords (T) and ventricle in between (V) RIGHT:Fluid-filled secondary internal and external laryngocele due to a small enhancing tumor in the laryngeal ventricle (T) obstructing the laryngeal ventricle. On the left side, an air-filled primary internal and external laryngocele.
LEFT: Coronal CT image through the larynx with normal anatomy: false cords (F), true cords (T) and ventricle in between (V) RIGHT:Fluid-filled secondary internal and external laryngocele due to a small enhancing tumor in the laryngeal ventricle (T) obstructing the laryngeal ventricle. On the left side, an air-filled primary internal and external laryngocele.
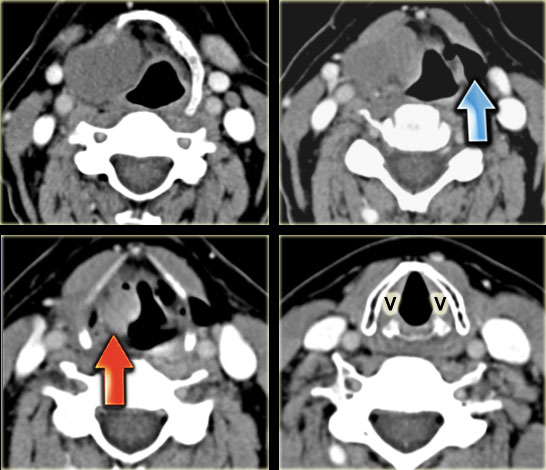
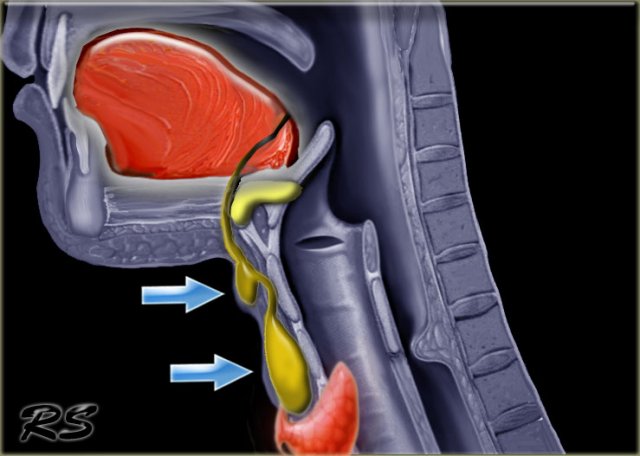
Mechanism of a laryngocele
The laryngeal ventricle (v) is a slit-like opening between the false and true vocal cords (image far left).
It is the anatomic landmark between supraglottis and glottis.
The ventricle extends laterally and then cranially into the paraglottic space.
When the opening of the laryngeal ventricle is completely obstructed by tumor, the mucosa in the paraglottic space continues to produce fluid.
This results in a fluid-filled internal laryngocele.
Eventually the paraglottic space becomes filled up and the internal laryngocele will become external by extending outside of the larynx through the thyro-hyoid membrane.
When the opening of the laryngeal ventricle is partially obstructed, a pressure-valve mechanism may result in an air-containing internal laryngocele which may, eventually, become external (right image, red arrow).
Squamous cell carcinoma
On the left, a CT-image at the level of the thyroid cartilage.
There is an irregular mass centered in the right piriform sinus.
This mass is in the visceral space.
In this region the most common tumor is a squamous cell carcinoma.
This was proven at biopsy.
Notice the retropharyngeal space (yellow arrow).
This is a virtual space containing only some fat.
Squamous cell carcinoma (2)
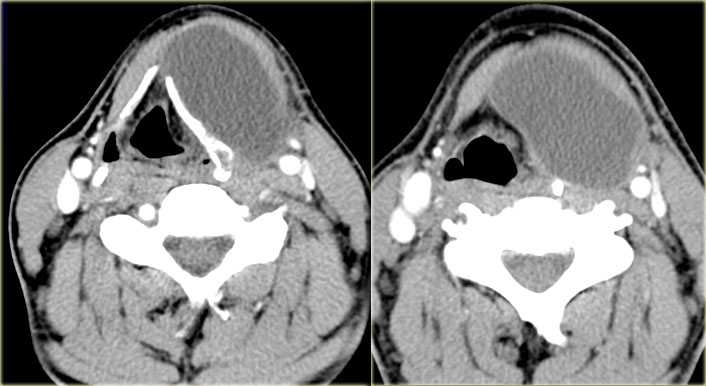
On the left, contiguous slices in a craniocaudal direction at the level of the larynx.
Study this case, which is quite similar to a previously discussed case and then continue reading.
- Mass with fluid density on the right at the level of the supraglottic larynx, i.e. a laryngocele. There is a small extralaryngeal component. Caudal to this laryngocele is a small enhancing tumor in the laryngeal ventricle (red arrow). Biopsy revealed squamous cell carcinoma.
- On the left side there is an air-filled laryngocele (blue arrow).
- The vocal cords (v) are normal.
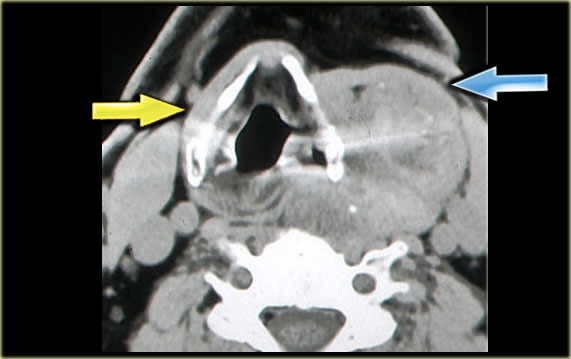 Multinodular goiter Strap muscles on right side (yellow arrow) and presumed position of strap muscles on the left (blue arrow)
Multinodular goiter Strap muscles on right side (yellow arrow) and presumed position of strap muscles on the left (blue arrow)
Multinodular goiter
Step 1: Which space
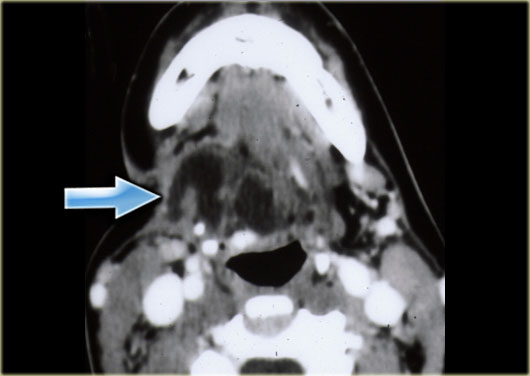
On the left a patient with a swelling on the left side of the neck, which has existed for years.
The swelling is adjacent to the left lamina of the thyroid cartilage.
The strap musculature seems to be draped over the lesion (blue arrow).
Therefore this lesion lies within the visceral space.
Step 2: Normal contents
Analysis of the normal anatomical contents of the visceral space rules out many possible tissues and organs from which this pathology may arise:
-
Larynx and hypopharynx
This mass is located outside of the larynx and hypopharynx.
The hypopharynx is slightly displaced due to the retropharyngeal extension of the mass and the lesion lies cranial to the trachea. -
Embryological remnants
Remnants like thyroglossal duct cyst can be considered but these lesions are usually cystic. -
Paratracheal lymph nodes
These are located outside of the strap musculature. -
Recurrent laryngeal nerve
This nerve is located within the tracheo-esophageal groove.
By exclusion we can say that this mass arises either from the thyroid gland or the parathyroid glands.
Step 3: Pattern recognition and clinical information
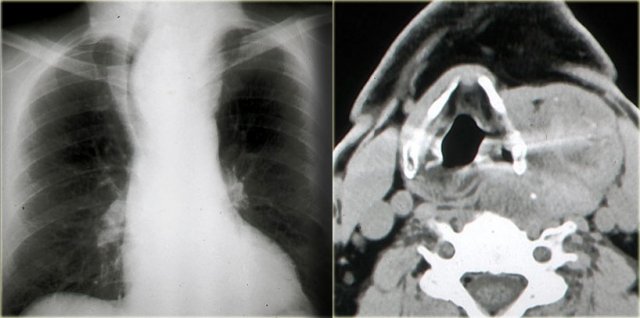
On the chest film we notice a displacement of the trachea to the right by an upper mediastinal mass.
So the mass is located within the visceral space and extends into the anterior mediastinum, since the trachea is located within the anterior mediastinum.
It is well-defined towards the surrounding fat and there are a few scattered coarse calcifications.
When we combine these findings, we recognize the radiological pattern of a benign multinodular goiter.
This diagnosis is compatible with the clinical information that the swelling in the neck has been present for years.
Thyroglossal duct cyst
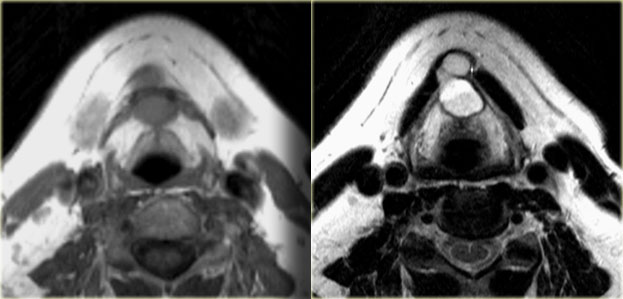
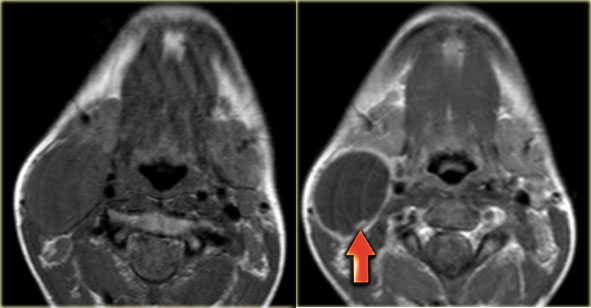
On the left axial T1- and T2-weighted images at the level of the hyoid bone.
There was no enhancement on the post Gadolinium study (not shown)
It is a midline cystic lesion, party external and partly internal to the hyoid bone and located in the visceral space.
The lesion is embedded in the strap musculature.
It is unlikely that this lesion arises from the trachea, thyroid gland, parathyroid glands or recurrent laryngeal nerve, since these structures are located more caudally.
Lymph nodes are usually seen in the subcutaneous fat around the larynx.
By exclusion a thyroglossal duct cyst is the most likely diagnosis.
Thyroglossal duct cyst (2)
Key facts
- The thyroglossal duct runs from the base of tongue at the foramen caecum to the thyroid gland.
- The embryonic thyroid gland or thyroid anlage travels through the duct to reach its final normal position. Normally, the thyroglossal duct then involutes, but when the duct persists, a thyroglossal duct cyst can develop anywhere along this tract (figure).
- The location is in the midline or paramedian.
- 65% are located infrahyoidal, 20% suprahyoidal and 15% at the level of the hyoid.
- Ddx: necrotic anterior cervical nodes and thrombosed jugular vein.
On the left an example of a paramedian thyroglossal duct cyst.
This lesion not in the midline, but the key finding is that this lesion is cystic and embedded in the strap musculature.
Thyroglossal duct cyst (3)
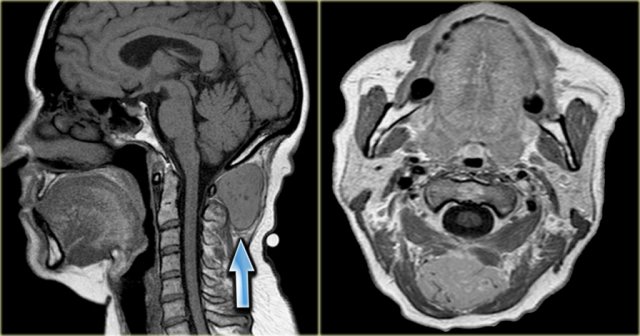
When the diagnosis thyroglossal duct cyst is made, always check if there is a thyroid in the normal position.
The thyroid anlage may never travel along the thyroglossal duct.
In that case it stays at the tongue base.
In these rare cases, the patient has a so-called lingual thyroid.
On the left another paramedian thyroglossal duct cyst
On the left, a child with a lingual thyroid.
This is the only functioning thyroid tissue that this child has.
It would be a disaster if such a 'lesion' were to be excised.
On the left images of a three-year old girl with a slowly enlarging tumor in the midline.
On ultrasound a hypoechoic ovoid smooth bordered lesion is seen at the level of the hyoid bone and slightly right off midline (left image).
During US examination, the lesion moves simultaneously with extrusion of the tongue.
Cystic nature and close relation to the hyoid bone makes thyroglossal duct cyst the most likely diagnosis.
Notice that a normal thyroid gland is present (right image).
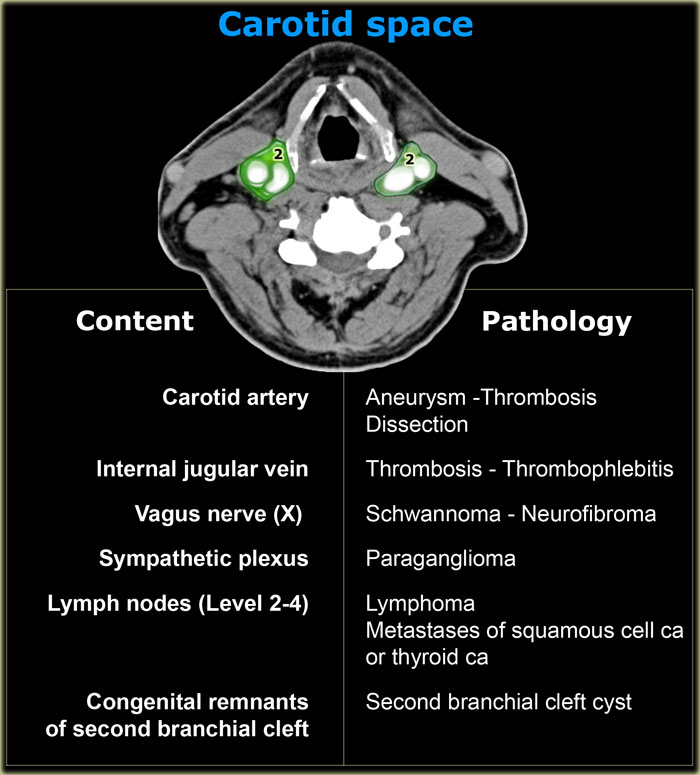
Carotid space
The carotid space extends from the skull base to the aortic arch.
It transverses the suprahyoid and infrahyoid neck into the anterior mediastinum.
On the left the normal contents of the carotid space and the derived pathology.
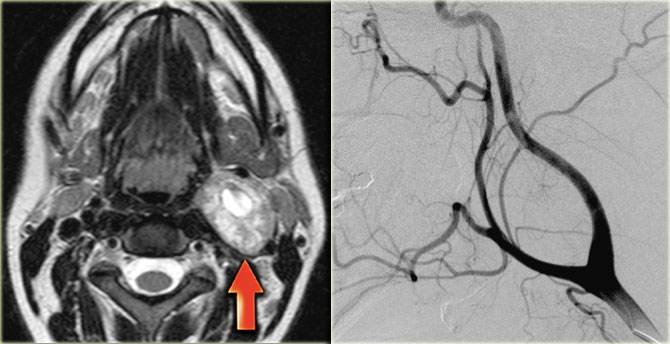
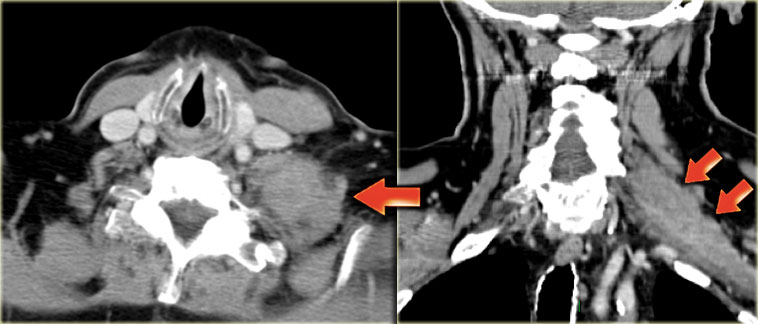
Paraganglioma
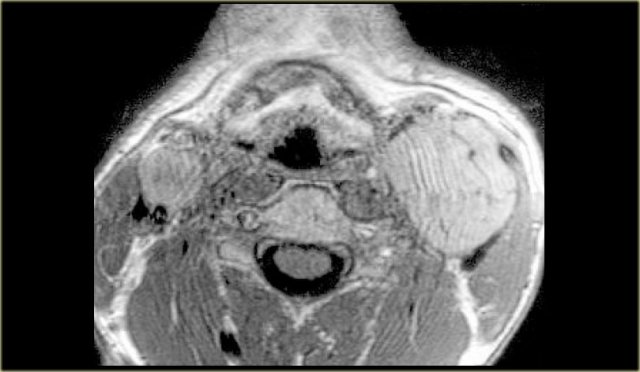
Step 1: Which space
On the left a patient with a swelling on the left side of the neck.
Study the MR-image at the level of the supraglottic larynx and decide in which space the lesion is located.
Then continue reading.
The swelling is centered between the external and internal carotid artery.
Notice that these vessels are compressed.
Evidently this lesion must be located in the carotid space.
Please note that there is a smaller, but identical, lesion present, located in the right carotid space.
Step 2: Normal contents
Now we must try to figure out the normal anatomical source that has caused this pathology.
Once again, we use exclusion:
- The carotid artery and internal jugular vein are compressed, but present.
- Level 2-4 lymph nodes are typically found lateral to the vessels and not in between.
-
Congenital remnants of the carotid space are usually second branchial cleft cysts.
As the name implies, these lesions are cystic. - Neural structures in the carotid space like the vagus nerve and sympathetic plexus are located between the great vessels.
Therefore it is very likely that the bilateral swellings of this patient are coming from these neural structures.
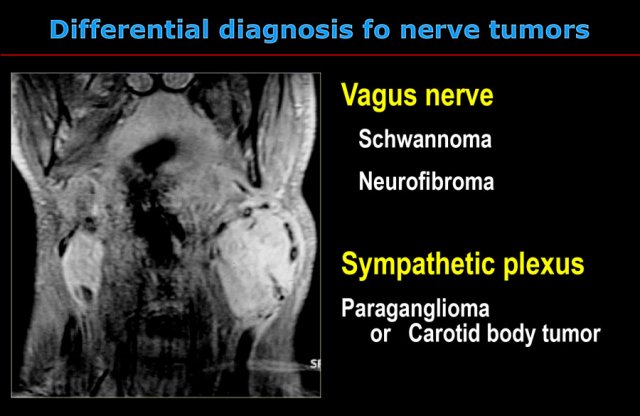
Now we are down to a fairly limited and space-specific differential diagnosis (see next image).
- Schwannomas and neurofibromas are rare tumors.
The only exception to this rule is in patients with neurofibromatosis.
Unlike this lesion, schwannomas and neurofibromas occur unilaterally.
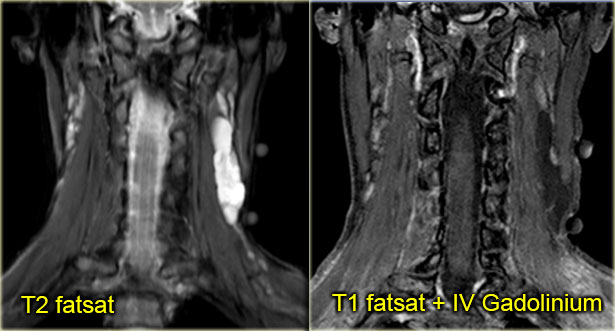
Although they enhance on MR, flow voids are usually absent. -
Paragangliomas are frequently multiple in 3% to 5% of patients overall and 20% to 30% with a positive family history.
These lesions show intense enhancement on CT and MR as seen on this coronal post-Gadolinium MR-image.
In the larger lesion on the left, typical flow voids are present (see also axial image).
So we can conclude that there are bilateral intensely enhancing lesions with flow voids in the carotid space, most likely carotid body tumors or paragangliomas.
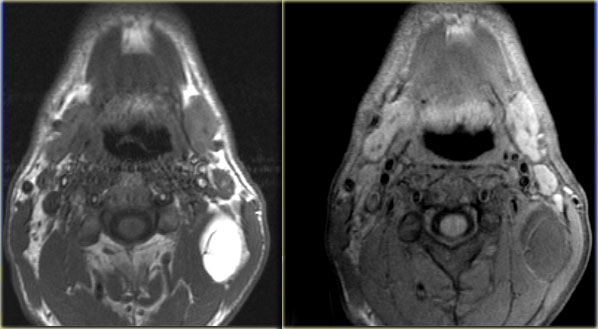
Paraganglioma (2)
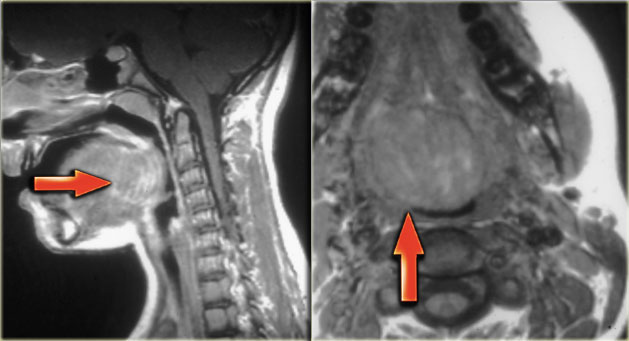
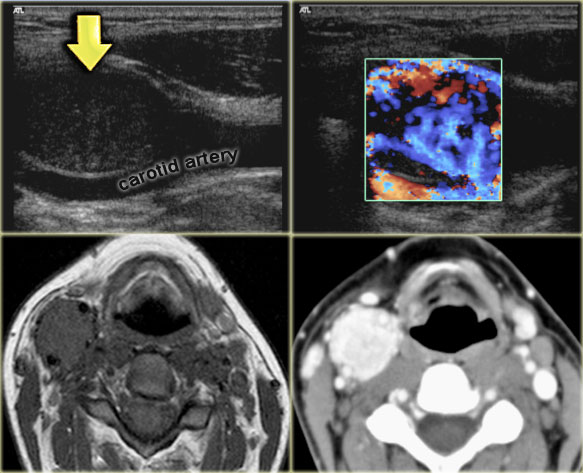
On the left images of a 21-year old female with a mass on the right.
This lesion is located between the internal and external carotid artery and therefore is a neural tumor.
The differential diagnosis is limited to tumors arising from the vagus nerve and sympathetic plexus.
On CT and color doppler the mass is clearly hypervascular and the only possible diagnosis is a paraganglioma.
Paraganglioma (3)
Key facts
- Also called carotid body tumor.
- Multiple in 4% of patients.
- 25% have a positive family history.
- Intense enhancement on CT and MR.
- Flow voids are frequently present.
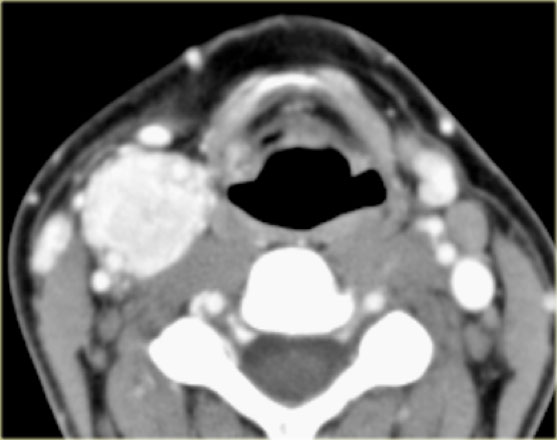
Schwannoma
On the left images of a 28-year old female with a nontender mass at the left mandibular angle.
Step 1
The mass is located in carotid space.
Step 2
Anatomical contents: carotid artery, internal jugular vein, vagus nerve, sympathetic plexus, lymph nodes (Level 2-4) and congenital remnants of the 2nd branchial cleft .
Step 3
- The carotid artery and internal jugular vein are displaced but look normal.
- Lymph nodes are typically found lateral to the vessels, not in between. On both sides an oval normal looking Level 2 lymph node is present.
- Congenital remnants of the carotid space are usually second branchial cleft cysts. As the name implies these lesions are cystic.
- Tumor of neural origin: the lesion is located between the great vessels.
Therefore it is very likely that this mass has a neural origin:
- Sympathetic plexus: a paraganglioma is unlikely, since a paraganglioma shows intense enhancement and multiple small vessels on an angiogram.
- Vagus nerve: Schwannoma or neurofibroma is the most likely diagnosis, since they can arise in this space.
They do enhance, but are not particularly hypervascular.
Flow voids are usually absent.
It is not possible to discriminate between these two possibilities based on their radiological appearance.
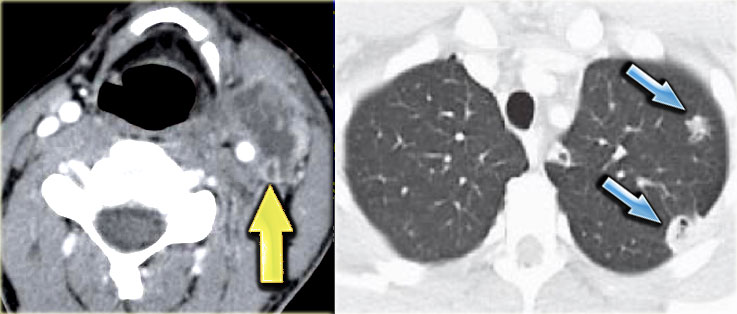
Jugular vein thrombosis
Thrombosis of the internal jugular vein is an under-diagnosed condition that may occur as a complication of head and neck infections, surgery, central venous access, and intravenous drug abuse.
An infected jugular vein thrombus caused by extension of an oropharyngeal infection is referred to as Lemierre's syndrome.
This is a bacterial infection that may have severe morbidity or even fatal outcome, as eventually septic emboli may spread to the lungs.
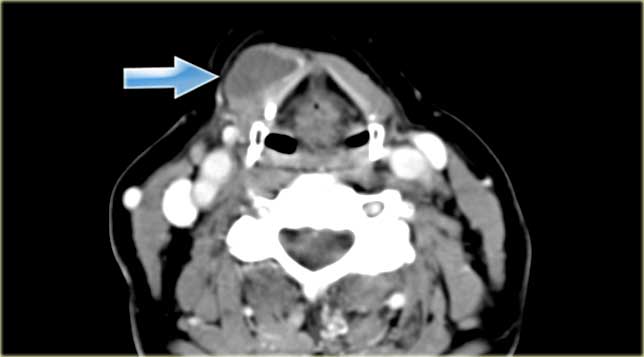
On the left a patient who had undergone a total laryngectomy several years previously.
The present complaint is a painful swelling on the left side of the neck since one day.
Step 1
Contrast-enhanced CT at mid-neck level shows the neopharynx with some surgical clips on the left and the enhancing right thyroid lobe which is still in situ.
In addition there is a round, hypodense lesion in the left carotid space.
Step 2
In this case, analysis of the normal anatomical contents of the carotid space can be short.
When we compare left to right it is clear that we are dealing with an internal jugular vein which is enlarged and does not enhance.
An image at a higher level shows the same appearance of the internal jugular vein (arrow).
Step 3
In combination with the clinical information of a painful swelling on the left side of the neck, there is only one possible diagnosis:
Acute thrombosis of the left internal jugular vein.
Lemierre' s syndrome
When you diagnose an acute thrombosis of the internal jugular vein, always look for pulmonary symptoms, i.e. Lemierre' s syndrome.
The oral infection spreads into the neck and causes internal jugular vein thrombophlebitis with subsequent septic emboli.
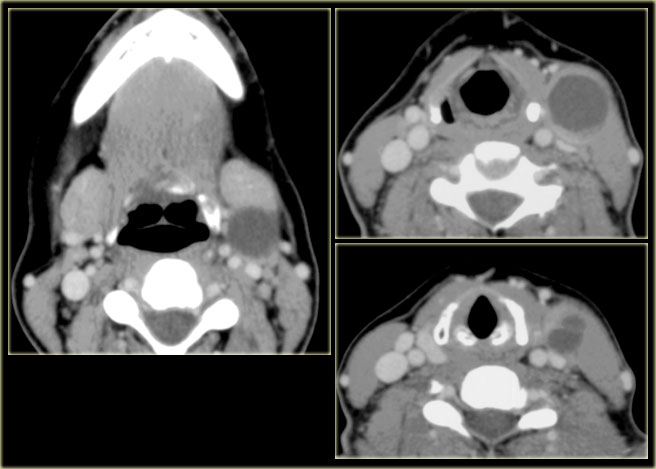
Second branchial cleft cyst
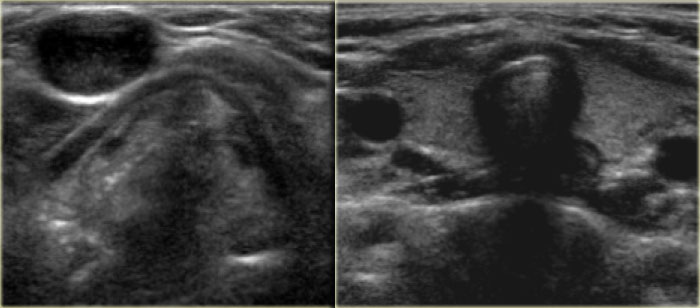
On the left images of a 36-year old female with a progressive swelling on the left side of the neck.
She had recently recovered from a peritonsillar abscess.
ENT-examination showed a fistula orifice in the left tonsil.
The position of the mass on the CT indicates that it is located in the carotid space.
Analysis based on normal anatomical contents:
- Carotid artery and internal jugular vein: normal.
- Vagus nerve or sympathetic plexus: the mass is not in between the vessels, so neurogenic lesions can be scrapped.
- Lymph node: this could certainly be a necrotic lymph node.
- Congenital remnants: the cystic appearance of the lesion, in combination with the clinical information makes a second branchial cleft cyst the most likely diagnosis.
Second branchial cleft cyst (2)
Key facts
- 95% of all branchial cleft anomalies arise from the second branchial cleft.
- Most common presentation: cyst, sometimes in combination with a sinus or fistula.
- Infection indicated by increased density, septations and wall thickening.
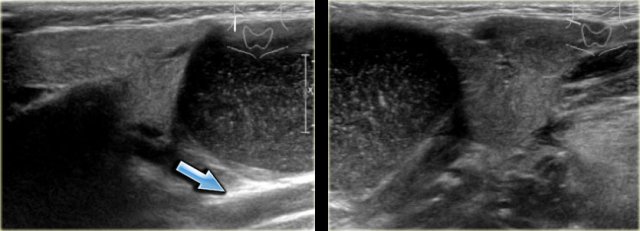
On the left a longitudinal and transverse image fo a large second branchial cleft cyst in a 12-year old girl situated between the parotid gland (left image) and the submandibular gland (right image).
It is superficial to the carotid artery and jugular vein (arrow).
The cyst contents is hypoechoic with freely moving debris.
The MR of the same patient confirms the presence of a cystic mass in the right carotid space.
The lesion is situated between the submandibular gland and the anterior margin of the sternocleidomastoid muscle, which is the classic position of a second branchial cleft cyst.
The lesion shows edge enhancement post-Gadolinium.
Notice that these lesions may contain small amounts of lymphoid tissue which is a possible explanation for the small area of enhancement inside the cyst wall (arrow).
Coronal STIR image of the same cyst.
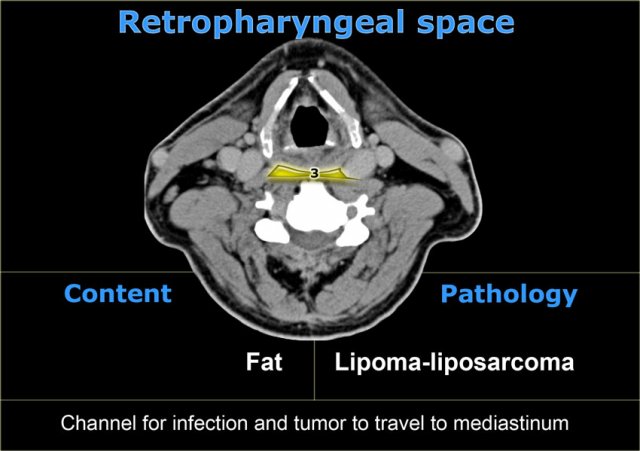
Retropharyngeal Space
The retropharyngeal space extends superiorly to the base of the skull and inferiorly to the posterior mediastinum at the level of the tracheal bifurcation.
In normal circumstances, the retropharyngeal space is a virtual space and contains the retropharyngeal lymph nodes superiorly as well as some fatty tissue.
Infections of the mouth can spread through this space into the posterior mediastinum.
There are two other spaces in close proximity to the retropharyngeal space: the danger space and the prevertebral space.
They are often confused with the retropharyngeal space.
The danger space actually lies between the alar fascia, which forms the posterior border of the retropharyngeal space, and the prevertebral fascia.
It extends from the cranial base above to the level of the diaphragm.
The prevertebral space is bounded anteriorly by the prevertebral fascia and posteriorly by the longus colli muscles of the spine.
It extends down the mediastinum and continues to the insertion of the psoas muscles.
All we need to realize is that pathology in this region can extend into the posterior mediastinum and we should not stop imaging until the tracheal bifurcation is reached.
Retropharyngeal abscess
On the left an axial contrast enhanced CT-image of an infant with fever.
The child cannot swallow.
This pathology is located in the retropharyngeal space.
The prevertebral muscles are pushed towards the vertebral body.
If this were a lesion located in the perivertebral space, these muscles would be pushed anteriorly.
The retropharyngeal space is expanded and contains multiple pockets of material with fluid density.
Obviously this is a retropharyngeal infection with multiple abscesses.
This is an emergency situation because the abscesses will expand and may eventually obstruct the airways.
Usually these deep abscesses require surgical drainage.
On the left an adult patient with a retropharyngeal abscess after surgical drainage.
The drainage catheters run from left to right through the retropharyngeal space.
The retropharyngeal space can become infected in two ways.
The 'classic' retropharyngeal abscess observed in pediatric patients occurs when an upper respiratory infection like pharyngitis or adenoiditis spreads to retropharyngeal lymph nodes.
Penetrating trauma, i.e. foreign bodies, fish bones or iatrogenic causes such as endoscopy or intubation, can also be involved in retropharyngeal space infection.
Retropharyngeal edema
On the left two images of a patient with a piriform sinus carcinoma (shown earlier).
On the far left the pirifrom sinus tumor before radiotherapy.
The image next to it shows complete response after the radiotherapy.
The retropharyngeal space is now distended and shows increased density of the fatty tissue due to post-radiotherapy edema.
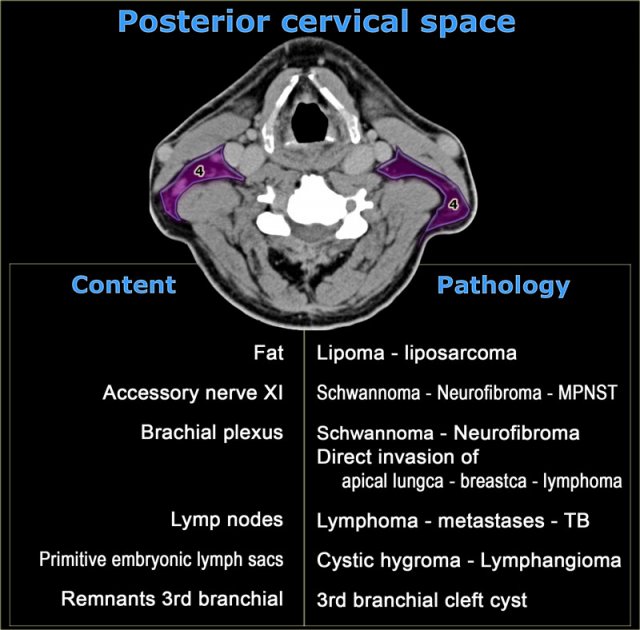
Posterior cervical space
On the left a table with the normal contents of the posterior cervical space and subsequent pathology.
MPNST is short for malignant peripheral nerve sheath tumor, which is the proper name for a malignant schwannoma.
Lymphoma
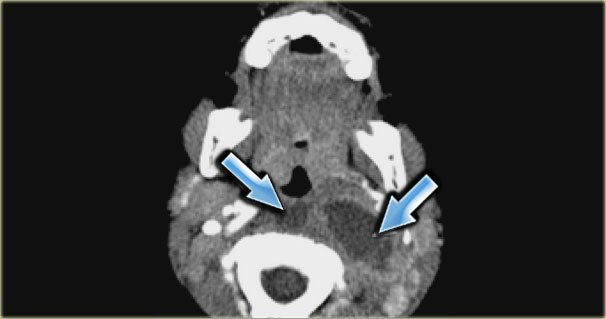
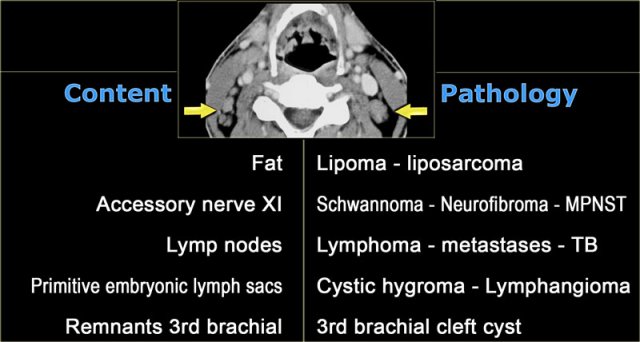
Step 1: Which space
On the left a patient with bilateral swelling in the neck.
CT image at the level of the hyoid bone shows multiple rounded lesions medial to the sternocleidomastoid muscles and dorsal to the internal jugular veins.
These bilateral multiple lesions are located in the posterior cervical space.
Step 2
Analysis of the normal anatomical components of the posterior cervical space:
- Fat
The fat looks normal. - Accessory nerve
Accessory nerve pathology is expected to be unilateral. - Brachial plexus
Brachial plexus pathology like neurofibromatosis could be considered.
However we would expect continuous lesions like nerves and not these separate rounded lesions. - Primitive embryonic lymph sacs:
Congenital remnants like cystic hygroma can be bilateral.
These are confluent cystic low-density lesions.
Step 3
By exclusion we can conclude that these are bilaterally enlarged lymph nodes with homogeneous enhancement.
Homogeneous enhancement is typical for lymphoma.
Central necrosis is more typical for squamous cell carcinoma metastases.
Lymph node biopsy in this patient revealed B-cell Non-Hodgkin lymphoma.
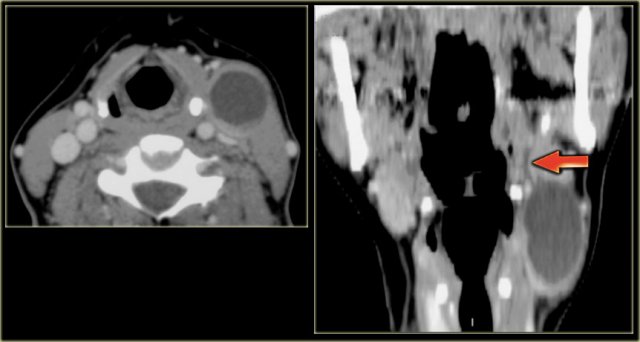
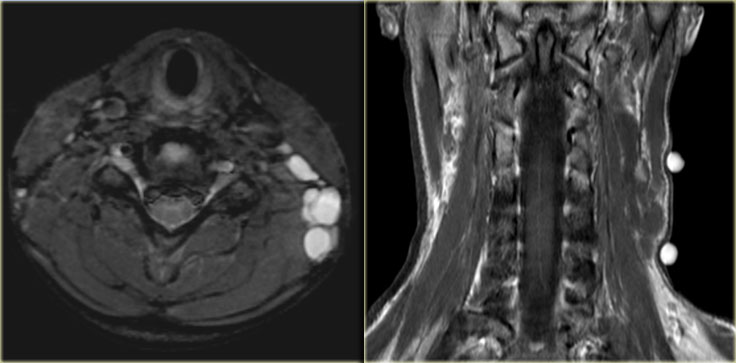
Lymphoma (2)
On the left images of a 67-year old woman who had a history of Non-Hodgkin lymphoma.
She had recently noticed a swelling on the left side of the neck.
Step 1
CT image at the level of the true vocal cords shows a mass, which is clearly located in the posterior cervical space.
Step 2
The mass is well-defined and isodense to muscle.
Coronal reformation shows the mass to be elongated and extending towards the axilla following rhe course of the cervico-brachial plexus..
Continue with the MR images.
The lesion originates at the left neural foramina and grows along the course of the brachial plexus (red arrow).
In fact, we are looking at a grossly thickened plexus.
Step 3
The radiological pattern confirms the neurogenic origin of the mass.
Combined with the history the final diagnosis is diffuse infiltration of the left brachial plexus by recurrent NHL.
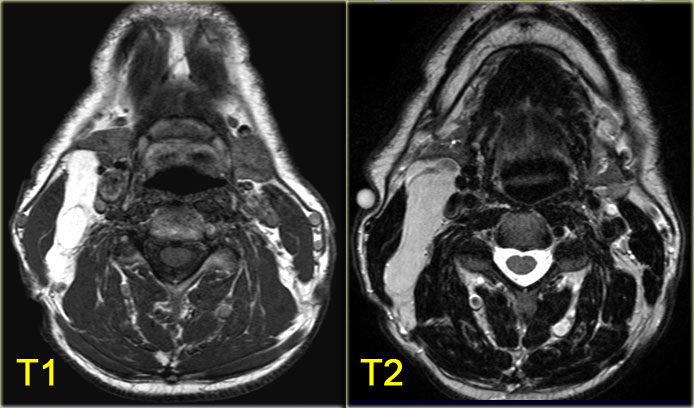
Lipoma
On the left images of a patient with a swelling posteriorly on the left side of the neck.
MR image at the level of the hyoid bone.
The lesion is located in the posterior cervical space.
Analysis of the normal anatomical components of the posterior cervical space can be short in this case.
The mass has the signal intensity of fat on a T1-weighted image and the signal is completely suppressed with fat suppression.
There was no enhancement (not shown), so we can conclude that this is a lipoma.
On the left T1- and T2-weighted images of another patient with a lipoma.
Lymphangioma or Cystic hygroma
On the left an axial T2-weighted image with fatsat and a coronal T1-weighted image of a 12-year old girl who presented with a soft swelling in the neck.
Step 1
A multiloculated lesion is present in the posterior cervical space.
Step 2
Analysis of the anatomical components:
- Fat:
The coronal T1-weighted image shows normal fat around the lesion. - Nerves:
Accessory nerve pathology is rare and we would expect a solitary solid lesion.
Brachial plexus lesions are expected to be located in a more paraspinal location. - Lymph nodes:
Can be considered, but these are solid or partly solid. Embryological remnants:
Remnants of the primitive lymphatic system like lymphangioma are most common in this age group and should be considered.
Step 3
On the T2-weighted image with fatsat the lesion is multiloculated and has a fluid intensity.
There is no enhancement on the T1-weighted image.
These findings, in combination with the fact that the swelling is soft and is present in a child, is specific for the diagnosis of a lymphangioma, also known as cystic hygroma.
 Cystic hygroma located in the right floor of the mouth in a young adult patient (courtesy: Tony Hasso)
Cystic hygroma located in the right floor of the mouth in a young adult patient (courtesy: Tony Hasso)
Lymphangioma (2)
Key facts
- Benign non-capsulated lesion arising from expanding embryonic lymph 'lakes' that do not develop normal lymphatic drainage.
-
90% in children
10% in young adults.
May occur anywhere in the head and neck. Mostly located in posterior cervical space. 10% extend into the mediastinum. -
High signal on T2-weighted images
Signal on T1-weighted images depends on protein content. - Hemorrhage results in rapid growth and fluid-fluid levels as seen on MR.
Perivertebral space
On the left a table with the normal contants of the perivertebral space and subsequent pathology.
Sarcoma
On the left a contrast enhanced CT image through the upper neck of a patient who complained of a slowly growing swelling posteriorly on the left side of the neck.
Step 1: Which space
There is a large soft tissue mass adjacent to the vertebral body centered in the perivertebral space.
Step 2
Analysis of the normal anatomical components of the perivertebral space:
- Vertebral body Is not involved.
- Brachial plexus. Lesions coming from the cervico-brachial plexus are expected to be found in a more paraspinal location.
- Vertebral artery and vein Are not involved.
- Prevertebral and paraspinal musculature. The lesion is clearly arising from the left paraspinal musculature.
Step 3
The normal fat planes between the individual muscles have disappeared. The imaging characteristics are otherwise non-specific.
This leaves us with a fairly large differential diagnosis of muscle pathology: sarcoma, fibromatosis, lymphoma and infection.
The clinical information of a slow-growing mass favors a malignant process.
Biopsy of the mass revealed sarcoma.
Benign fibrous tumor
On the left a 75-year old male with a slowly enlarging mid-line mass.
Step 1
The lesion is located in the perivertebral space.
Step 2
The vertebral body and vertebral vessels are not involved.
Lesions coming from the cervico-brachial plexus are expected to be found in more paraspinal locations.
There is vivid enhancement of the mass.
Centrally flow voids are present, indicating a hypervascular nature.
The imaging characteristics are otherwise non-specific.
Step 3
The clinical information of a slow-growing mass favors a malignant process.
A biopsy taken before excision revealed a benign fibrous tumor.
Charity
All the profits of the Radiology Assistant go to Medical Action Myanmar which is run by Dr. Nini Tun and Dr. Frank Smithuis sr, who is a professor at Oxford university and happens to be the brother of Robin Smithuis.
Click here to watch the video of Medical Action Myanmar and if you like the Radiology Assistant, please support Medical Action Myanmar with a small gift.